Abstract
Background:
Hypospadias is a congenital anomaly on the penis, in which the meatal orifice opens ventrally and proximal to the tip of the penis. In this regard, two common treatment methods are tubularized incised-plate urethroplasty (TIP) and the Mathieu incised-plate (MIP) technique. The present study aimed to compare the early and long-term outcomes of TIP and MIP among patients with distal penile hypospadias.Objectives:
The study was also to evaluate the postoperative functional outcome of hypospadias over a long-term follow-up.Methods:
Fifty-nine patients were randomly selected and assigned to two groups (TIP (n = 31) and MIP (n = 28)). Demographic information, preoperative findings, and postoperative complications were collected from the two groups. The Hypospadias Objective Scoring evaluation (HOSE) questionnaire and uroflowmetry were obtained to evaluate the long-term outcome of hypospadias repair.Results:
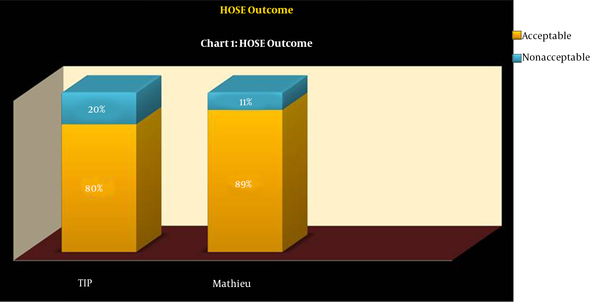
The success rates of the surgical TIP and MIP techniques were 71.0% and 82.1%, respectively. Postoperative complications in the TIP group were three (9.7%) distal UCF and four (12.9%) meatal stenosis. In the MIP group, two (7.1%) and three (10.7%) patients suffered from distal UCF and meatal stenosis, respectively. Moreover, 89.3% of the patients in the MIP group and 80% of the patients in the TIP group had acceptable HOSE. Regarding the uroflow rates in the MIP group, 12% and 58% of the participants were below the 5th percentile and above the 25th percentile, respectively. Concerning the uroflow rates of TIP, 32% of the patients were below the 5th percentile, and 18% of the participants were above 25th percentile.Conclusions:
Although there have been some reports on the superiority of TIP, we found these two techniques at approximately equal levels with a slightly higher success rate for the MIP regarding the early outcomes. With the exception of the long-term outcomes in cosmetic and functional evaluation, MIP is superior to TIP.Keywords
1. Background
Hypospadias is a congenital defect of the penis, in which the urethral meatus is located ventrally and proximal to the tip of the penis from the glance to the perineum (1, 2). Regarding many factors such as the severity of Chordee, the presence of adequate supportive tissue for urethral reconstruction, urethral plate quality, and surgeon's experience, there is no agreement among surgeons on the selection of an optimal hypospadias repair technique (3, 4).
UCF is one of the most common complication among patients suffering from hypospadias. The patient with UCF commonly needs to undergo surgery once more at 6-12-month intervals; however, its high failure rate is still high (5).
Tabularized incised-plate (TIP) urethroplasty is a standard surgical technique to treat distal hypospadias. Despite its widespread use, it still exposes patients to some complications, at the top of which is UCF. On the other hand, the Mathieu incised-plate (MIP) technique is also one of the most preferred alternative procedures, generally used in specialized centers (6).
The functional outcome of hypospadias repair is considered as a cosmetic outcome. In some studies, structured scoring systems and uroflowmetry were used to assess results of hypospadias repair. Holland et al. (7) described a scoring system incorporating an assessment of meatal location and shape, urinary stream, erection straightness, and the presence and complexity of any urethral complication.
2. Objectives
Considering the remarkable impacts of the disease on the physical and psychological status of the patients and their guardians, its inescapable needs for surgery, and its probable complications, this study discusses the long-term outcomes and complications of TIP and MIP.
3. Methods
3.1. Patients
The distal penile hypospadias cases referred to our surgery clinic during 2006 - 2011 were included in this study. All surgeries were undergone by a highly-experienced surgeon, who was competent in both TIP and MIP techniques.
Fifty-nine patients were randomly selected and assigned to two groups (TIP (n = 31) and MIP (n = 28)). After excluding the patients with a previous history of hypospadias surgery, urethral plate < 8 millimeters, penile Chordee > 30 degrees, and hypoplastic urethra proximal to hypospadias meatus as well as those who were unwilling to participate in the study, 59 patients with distal shaft hypospadias were included in the study. In all cases, an artificial erection test was performed on the operating table to check for the elimination of Chordee after penile de-gloving. In all cases, a single dartos flap was used. Moreover, all patients benefited from a standardized sandwich dressing.
The HOSE questionnaire (7) and uroflowmetry were used to evaluate the long-term outcomes of hypospadias repair. Furthermore, the patients were followed up at two stages (namely early and late). The patients were then appointed to participate in their first follow-up visit during Days 7 - 14 post-surgery. The second and the third follow-up visits were set three and six months after the surgery, and the last visit was about 90 months after surgery.
The required data were collected by importing the patient’s information into the certain forms developed by the researchers, which encompassed demographic indirmation, presence or absence of Chordee, duration of hospitalization, number of performed surgical procedures, postoperative complications (e.g., UCF and Chordee level), duration of urethral catheterization, and need for re-hospitalization. Then the participants were called and asked for a visit and uroflowmetry.
In the last visit, about 90 months after surgery, meatal location and shape, urinary stream, erection straightness, and presence of fistula were assessed, and scoring was performed based on the instructions of the HOSE questionnaire. Acceptable and non-acceptable HOSE scores were set to be 14 - 16 and ≤ 13, respectively.
Uroflowmetry procedures and its possible benefits and complications were explained to the patients’ guardians, and their informed consent to participant in the study was obtained. Then uroflowmetry was performed, and maximum flow rate (Q-max), average flow rate (Q-ave), voided volume (vv), time to maximum flow, flow time, and voiding time were recorded. Afterward, maximum urine flow rate to voided volume inserted in Iranian Kajbafzadeh et al. (8) Uroflowmetry nomogram (8). In definition, normal flow > 25th percentile, equivocal obstruction 5th - 25th percentile, and obstructed flow < 5th percentile considered.
3.2. Analyzed Factors and Statistical Analysis
The data on the demographic information, preoperative findings, perioperative outcomes, and postoperative complications were collected from the TIP and MIP groups, tabulated, and compared using the SPSS software (IBM SPSS Statistics for Windows, version 22.0. Armonk, NY, USA). The chi-square tests, Fisher’s exact-test, and Mann Whitney U-test were used to compare the results. In this study, P < 0.05 was set as the significance level.
3.3. Ethical Considerations
Type of assessment, uroflowmetry procedures, the possible benefits, and complications of uroflowmetry were explained to the patient's guardians. No additional intervention or cost was imposed on the patients in this study. Patients’ information was used in this study as encoded parameters observing the confidentiality principle. The personal information of no patient was included in this research, and only the statistical analysis of the data was presented in general. The informed consent was obtained from the legal guardian(s) of each participant, and the patients were excluded from the study if the patient or their parents were not willing to participate in the study. The study was approved by the Institutional Board Review and the Medical Ethics Committee of the Shahid Beheshti University of Medical Sciences.
4. Results
Of the 59 patients in the study, 31 patients underwent the TIP surgery, and 28 persons underwent MIP. The participants’ mean age at the first surgery was 29.53 and 30.33 months in the TIP and MIP groups, respectively. The age at the time of assessment ranged from 5 - 11 years old, with a mean follow-up age of 90 months.
Of the 31 surgically-treated patients with TIP, 28 patients (90.3%) revealed no concurrent anomalies, only two cases (6.5%) had unilateral undescended testis (UDT), and one case (3.25%) suffered from an inguinal hernia. Of the 28 patients treated with the MIP procedure, 23 cases (82.1%) showed no concurrent anomalies, and three cases (10.7%) of unilateral UDT, one case (3.6%) of an inguinal hernia, and one case (3.6%) of mental retardation were reported. In the two surgical groups, P = 0.853 for the concomitant anomalies with hypospadias, indicating no statistical difference between the two groups.
Three patients in the MIP group and three patients in the TIP group had Chordee < 30; hence, Chordee was repaired in all patients with dorsal plication.
There was no statistically significant difference between the surgical technique and the need for the homeostasis method (P = 0.141). Eleven patients in the TIP group required epinephrine, and nine persons needed a tourniquet to establish homeostasis, while two patients in the MIP group required a tourniquet, and 20 cases required to inject epinephrine to maintain homeostasis. In both groups, repairs were performed with polydioxanone (PDS) suture material. Among the patients treated by both techniques, a silastic dripping stent catheter was used after surgery.
The success rates were 71.0 % and 82.1% for the TIP and MIP techniques, respectively. Regarding the postoperative complications in follow-ups, the TIP group reported three cases (9.7%) of distal UCF, four cases (12.9%) of meatal stenosis, one case (3.2%) of urethral stricture, and one case (3.2%) of Chordee. In the MIP group, only two (7.1%) and three (10.7%) patients suffered from distal UCF and meatal stenosis, respectively, and no other postoperative complication was observed in this group (Table 1).
Participants’ Characteristics
| Characteristics | TIP Group | Mathieu Group |
|---|---|---|
| Frequency | 31 | 28 |
| Mean age at first surgery, mo | 29.53 | 30.33 |
| Concurrent anomalies, % | 9.2 | 17.9 |
| Chordee before surgery (frequency) | 3 | 3 |
| Suture material | Polydioxanone (PDS) | Polydioxanone (PDS) |
| Urinary stent | Silastic dripping stent | Silastic dripping stent |
| Duration of Urinary stent, d | 6 | 6 |
| Ucf1, % | 9.7 | 7.1 |
| Meatal stenosis, % | 12.9 | 10.7 |
| Urethral stricture, % | 3.2 | 0 |
| Chordee after surgery, % | 3.2 | 0 |
Regarding the incidence of complications in each technique, especially the presence of UCF and meatal stenosis, which are considered as the significant complications of hypospadias correction surgery, and especially which method is more appropriate to choose, the results of the present study indicated that the patients in the TIP group experienced UCF more frequently than the MIP group and that there was a significant relationship between the presence of UCF and the used technique.
On the other hand, the study revealed the same results for the complication of meatal stenosis in the two surgery groups (P = 0.795), and their correlation was considered statistically insignificant.
In all patients with UCF, a redo operation was performed successfully to repair the fistula. The HOSE results in the last follow up are demonstrated in (Table 2).
Hypospadias Objective Scoring Evaluation (HOSE) Outcome in Last Follow-up
| HOSE Outcome | Score | Frequency in TIP Group (N = 31) | Frequency in Mathieu Group (N = 28) |
|---|---|---|---|
| Meatal location | |||
| Distal glans | 4 | 25 | 24 |
| Proximal to glans | 3 | 6 | 4 |
| Coronal Proximally on the penile | 2 | 0 | 0 |
| Shaft | 1 | 0 | 0 |
| Meatal shape | |||
| Vertical slit | 2 | 25 | 25 |
| Circular | 1 | 6 | 3 |
| Urinary stream | |||
| Single stream | 2 | 25 | 25 |
| Spray | 1 | 6 | 3 |
| Erection | |||
| Straight | 4 | 23 | 25 |
| Mild angulation (< 10 u) | 3 | 8 | 3 |
| Moderate angulation (> 10 u but < 45 u) | 2 | 0 | 0 |
| Severe angulation (> 45 u) | 1 | 0 | 0 |
| Fistula | |||
| None | 4 | 31 | 28 |
| Single subcoronal or more distal | 3 | ||
| Single proximal | 2 | ||
| Multiple or complex | 1 | ||
| Acceptable HOSE outcome, % | 80 | 89.3 |
In the MIP group, 89.3% of the participants had an acceptable HOSE, and 80% of the cases in the TIP group had an acceptable score (Figure 1) (P = 0.893). This correlation was considered statistically insignificant. The mean voided volume and the flow rate regarding the type of surgery are presented in (Table 3 and Figure 2).
Comparing HOSE outcomes between two groups
Comparing Uroflowmetry parameters between two groups
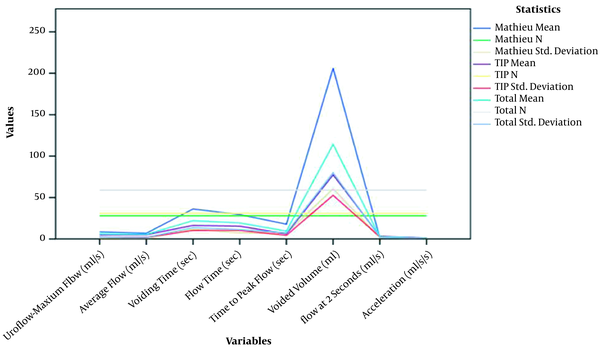
Uroflowmetry Parameter
| Surgical Technique | Uroflow-Maximum Flow, mL/s | Average Flow, mL/s | Voiding Time, s | Flow Time, s | Time to Peak flow, s | Voided Volume, mL | Flow at 2 Seconds, mL/s | Acceleration, mL/s/s |
|---|---|---|---|---|---|---|---|---|
| Mathieu | ||||||||
| Mean ± SD | 8.5000 ± 0.56569 | 6.9000 ± 0.28284 | 36.2000 ± 11.73797 | 29.4500 ± 7.42462 | 17.8000 ± 7.07107 | 206.1000 ± 60.38692 | 1.5500 ± 1.62635 | 0.4000 ± 0.14142 |
| N | 28 | 28 | 28 | 28 | 28 | 28 | 28 | 28 |
| TIP | ||||||||
| Mean ± SD | 5.1400 ± 2.48254 | 5.1000 ± 2.02978 | 16.4000 ± 10.31576 | 15.4000 ± 10.38581 | 6.1400 ± 4.42922 | 77.3800 ± 52.71216 | 3.3200 ± 2.56359 | 1.1200 ± 1.07098 |
| N | 31 | 31 | 31 | 31 | 31 | 31 | 31 | 31 |
| Total | ||||||||
| Mean ± SD | 6.1000 ± 2.61725 | 5.6143 ± 1.87921 | 22.0571 ± 13.68391 | 19.4143 ± 11.31804 | 9.4714 ± 7.33365 | 114.1571 ± 80.03191 | 2.8143 ± 2.35968 | 0.9143 ± 0.94415 |
| N | 59 | 59 | 59 | 59 | 59 | 59 | 59 | 59 |
Regarding the uroflow rates in the MIP group, 12% of the patients were below the 5th percentile, 31% patients were between the 5th and 25th percentiles, and 58% of the patients were above the 25th percentile. Regarding the uroflow rates in the TIP group, 32% of the cases were below the 5th percentile, 50% of patients were between the 5th and 25th percentiles, and 18% of the patients were above the 25th percentile (Figure 3).
Uroflowmetry nomogram in both groups
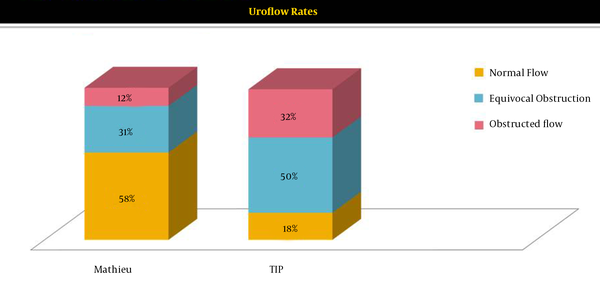
The uroflowmetry assessment results showed a statistically significant correlation between the presence of obstructive voiding and the surgery technique (P = 0.018). The development of obstructive voiding was significantly higher in the TIP group than the MIP group.
5. Discussion
Hypospadias is a congenital defect in the meatal orifice of the penis, the treatment of which requires surgical repair. Various urethroplasty techniques have been introduced for the hypospadias treatment; however, they have been associated with some complications regarding the severity of hypospadias, patients’ age, history of previous surgical repairs, and soft tissue support status. Moreover, the complications include a variety of rapid onset incidences such as surgical site infection and hematoma, or delayed events, including meatal retraction and stenosis, wound dehiscence, diverticulum, and urethrocutaneous fistula (UCF).
The treatment techniques aim to achieve the voiding in an upright position, develop a standard voiding stream, and maintain the normal penile shape and function (8-10).
In the present study, we compared the TIP and MIP techniques as the most popular urethroplasty techniques for hypospadias among most surgeons.
In this study, 59 patients met the inclusion criteria, and the collected data were recorded and evaluated. Of the participants, 31 patients underwent surgical repair using the TIP technique, and 28 persons were treated using the MIP techniques.
In Manzoni’s et al. (11) study, the age of 6 - 12 months was considered as the best age for performing a repair surgery for hypospadias. However, the patients’ mean ages in the first surgery in this study were 29.53 months in the TIP group and 30.33 months in the MIP group. Moreover, there was no significant difference between the two groups regarding age.
Many studies have reported the inguinal hernia and UDT as the most common concomitant anomaly among hypospadias patients, with the incidence rates of 9% and 6%, respectively (12-15). In our study, the incidence rate of the former was 1.7%, and the incidence of UDT was 8.5 % (5 out of 59 patients).
The presence of the bilateral UDT is much more highlighted among these patients because of the probability of underlying chromosomal disorders. However, none of the patients reported bilateral UDT in the present study.
In a systematic review, Wilkinson et al. investigated the outcomes of the TIP and MIP techniques and reported the incidence rates of postoperative complications in 6.7% of patients undergoing MIP surgery and 6.9% of the patients in the TIP group (6). Another two randomized clinical trials also reported the same complication rates for both of these techniques (16, 17).
Our study revealed a complication rate of 29.0% and 17.1% for the TIP and MIP techniques, respectively. This higher complication rate in this study could be explained based on the number of the participants. Further studies are recommended to detect the same issue with larger sample sizes.
The likelihood of complications, especially UCF and meatal stenosis in the TIP and MIP groups, was assessed in many studies and revealed a significant difference between the two groups in terms of complications (6, 10, 18-20). In our present study, we found a statistically significant difference between the TIP and MIP groups regarding UCF and meatal stenosis rates.
The effect of suturing material on developing complications in hypospadias patients has already been evaluated. For example, Ulman et al. stated a markedly greater likelihood of fistula formation in the group of patients treated with vicryl material stitch compared to the PDS group (21). However, Cimador et al. (22) found no significant difference between these two materials in their study. Accordingly, we used the same suture material for the two group.
HOSE and uroflowmetry are non-invasive and trouble-free means to evaluate the long-term outcomes of children after hypospadias repair. Regarding the uroflow rates in the MIP group, 12% of the subjects were below the 5th percentile, 31% patients were between the 5th and 25th percentiles, and 58% of the patients were above the 25th percentile.
Regarding the uroflow rates in the TIP group, 32% of subjects were below the 5th percentile, 50% of patients were between the 5th and 25th percentiles, and 18% of the cases were above the 25th percentile. The uroflowmetry assessment results revealed a statistically significant correlation between the presence of obstructive voiding and the surgery technique (P = 0.018). The development of obstructive voiding was significantly higher in the TIP group than the MIP group.
Given that many studies have reported remarkable improvement in functional obstructive voiding at puberty, watchful waiting and following the concerned parameters by examination and uroflowmetry are proposed to avoid unnecessary intervention (23).
5.1. Conclusions
The present study concluded the higher success rate and the better outcome of the Mathieu procedure, especially the long-term outcomes of cosmetic and functional evaluation, compared to the TIP method. One of the limitations of this study is small sample size; hence, future researchers are highly recommended to address this issue in further studies.
References
-
1.
Olsen LH, Grothe I, Rawashdeh YF, Jorgensen TM. Urinary flow patterns in infants with distal hypospadias. J Pediatr Urol. 2011;7(4):428-32. [PubMed ID: 20598640]. https://doi.org/10.1016/j.jpurol.2010.05.013.
-
2.
Dave S, Liu K, Garg AX, Shariff SZ. Secular trends in the incidence and timing of surgical intervention for congenital undescended testis and surgically treated hypospadias in Ontario, Canada between 1997 and 2007. J Pediatr Urol. 2018;14(6):552 e1-7. [PubMed ID: 30072120]. https://doi.org/10.1016/j.jpurol.2018.07.003.
-
3.
Andersson M, Doroszkiewicz M, Arfwidsson C, Abrahamsson K, Holmdahl G. Hypospadias repair with tubularized incised plate: Does the obstructive flow pattern resolve spontaneously? J Pediatr Urol. 2011;7(4):441-5. [PubMed ID: 20630805]. https://doi.org/10.1016/j.jpurol.2010.05.006.
-
4.
Djordjevic ML, Perovic SV, Slavkovic Z, Djakovic N. Longitudinal dorsal dartos flap for prevention of fistula after a Snodgrass hypospadias procedure. Eur Urol. 2006;50(1):53-7. [PubMed ID: 16707207]. https://doi.org/10.1016/j.eururo.2006.04.014.
-
5.
Kocherov S, Prat D, Koulikov D, Ioscovich A, Shenfeld OZ, Farkas A, et al. Outcome of hypospadias repair in toilet-trained children and adolescents. Pediatr Surg Int. 2012;28(4):429-33. [PubMed ID: 22331204]. https://doi.org/10.1007/s00383-012-3061-2.
-
6.
Wilkinson DJ, Farrelly P, Kenny SE. Outcomes in distal hypospadias: a systematic review of the Mathieu and tubularized incised plate repairs. J Pediatr Urol. 2012;8(3):307-12. [PubMed ID: 21159560]. https://doi.org/10.1016/j.jpurol.2010.11.008.
-
7.
Holland AJ, Smith GH, Ross FI, Cass DT. HOSE: an objective scoring system for evaluating the results of hypospadias surgery. BJU Int. 2001;88(3):255-8. [PubMed ID: 11488741]. https://doi.org/10.1046/j.1464-410x.2001.02280.x.
-
8.
Kajbafzadeh AM, Yazdi CA, Rouhi O, Tajik P, Mohseni P. Uroflowmetry nomogram in Iranian children aged 7 to 14 years. BMC Urol. 2005;5:3. [PubMed ID: 15771771]. [PubMed Central ID: PMC1079892]. https://doi.org/10.1186/1471-2490-5-3.
-
9.
Bae SH, Lee JN, Kim HT, Chung SK. Urethroplasty by use of turnover flaps (modified mathieu procedure) for distal hypospadias repair in adolescents: comparison with the tubularized incised plate procedure. Korean J Urol. 2014;55(11):750-5. [PubMed ID: 25405018]. [PubMed Central ID: PMC4231153]. https://doi.org/10.4111/kju.2014.55.11.750.
-
10.
Khalil M, Gharib T, El-Shaer W, Sebaey A, Elmohamady B, Elgamal K. Mathieu technique with incision of the urethral plate versus standard tubularised incised-plate urethroplasty in primary repair of distal hypospadias: A prospective randomised study. Arab J Urol. 2017;15(3):242-7. [PubMed ID: 29071159]. [PubMed Central ID: PMC5651952]. https://doi.org/10.1016/j.aju.2017.03.007.
-
11.
Manzoni G, Bracka A, Palminteri E, Marrocco G. Hypospadias surgery: when, what and by whom? BJU Int. 2004;94(8):1188-95. [PubMed ID: 15613162]. https://doi.org/10.1046/j.1464-410x.2004.05128.x.
-
12.
Mohajerzadeh L, Mirshemirani A, Rouzrokh M, Sadeghian N, Khaleghnejad-Tabari A, Mahdavi A, et al. Evaluation of Onlay Island Flap Technique in Shallow Urethral Plate Hypospadiasis. Iran J Pediatr. 2016;26(1). e660. [PubMed ID: 26848382]. [PubMed Central ID: PMC4733298]. https://doi.org/10.5812/ijp.660.
-
13.
Mohajerzadeh L, Ghoroubi J, Roshanzamir F, Alizadeh H. Outcome of tubularized incised plate (TIP) urethroplasty: A single-center experience with 307 cases. Iran J Pediatr Surg. 2015;1(1):22.
-
14.
Sabetkish S, Kajbafzadeh AM, Sabetkish N. Hypospadias and concomitant undescended testis: Comparison of no skin incision with inguinal and scrotal skin incision orchiopexy. Int J Surg. 2015;22:154-8. [PubMed ID: 26343974]. https://doi.org/10.1016/j.ijsu.2015.08.073.
-
15.
Springer A, van den Heijkant M, Baumann S. Worldwide prevalence of hypospadias. J Pediatr Urol. 2016;12(3):152 e1-7. [PubMed ID: 26810252]. https://doi.org/10.1016/j.jpurol.2015.12.002.
-
16.
Oswald J, Korner I, Riccabona M. Comparison of the perimeatal-based flap (Mathieu) and the tubularized incised-plate urethroplasty (Snodgrass) in primary distal hypospadias. BJU Int. 2000;85(6):725-7. [PubMed ID: 10759674]. https://doi.org/10.1046/j.1464-410x.2000.00479.x.
-
17.
Elganainy EO, Abdelsalam YM, Gadelmoula MM, Shalaby MM. Combined Mathieu and Snodgrass urethroplasty for hypospadias repair: a prospective randomized study. Int J Urol. 2010;17(7):661-5. [PubMed ID: 20438585]. https://doi.org/10.1111/j.1442-2042.2010.02537.x.
-
18.
Aminsharifi A, Taddayun A, Assadolahpoor A, Khezri A. Combined use of Mathieu procedure with plate incision for hypospadias repair: a randomized clinical trial. Urology. 2008;72(2):305-8. [PubMed ID: 18502484]. https://doi.org/10.1016/j.urology.2008.02.034.
-
19.
Moradi M, Moradi A, Ghaderpanah F. Comparison of snodgrass and mathieu surgical techniques in anterior distal shaft hypospadias repair. Urol J. 2005;2(1):28-31. [PubMed ID: 17629892].
-
20.
Hueber PA, Antczak C, Abdo A, Franc-Guimond J, Barrieras D, Houle AM. Long-term functional outcomes of distal hypospadias repair: a single center retrospective comparative study of TIPs, Mathieu and MAGPI. J Pediatr Urol. 2015;11(2):68 e1-7. [PubMed ID: 25824882]. https://doi.org/10.1016/j.jpurol.2014.09.011.
-
21.
Ulman I, Erikci V, Avanoglu A, Gokdemir A. The effect of suturing technique and material on complication rate following hypospadias repair. Eur J Pediatr Surg. 1997;7(3):156-7. [PubMed ID: 9241502]. https://doi.org/10.1055/s-2008-1071079.
-
22.
Cimador M, Castagnetti M, Milazzo M, Sergio M, De Grazia E. Suture materials: do they affect fistula and stricture rates in flap urethroplasties? Urol Int. 2004;73(4):320-4. [PubMed ID: 15604576]. https://doi.org/10.1159/000081592.
-
23.
Thakur ND, Mulay AR, Satav VP, Mane DA, Sabale VP, Kankalia SK. Uroflow nomogram for healthy, 15-40 year old Indian men. Indian J Urol. 2016;32(4):293-5. [PubMed ID: 27843212]. [PubMed Central ID: PMC5054660]. https://doi.org/10.4103/0970-1591.191253.
