1. Background
Recent advances in antenatal, obstetric, and neonatal care, including nursing care, have decreased the mortality of premature neonates (1). Functional immaturity of the gastrointestinal (GI) tract in premature infants causes several problems, including disturbed sucking and swallowing, delayed gastric emptying, ileus of prematurity, and intestinal immaturity, leading to delayed enteral feeding (2). Enteral feeding, even if very restricted, can cause improvements in the GI tract development, function, and movement, in addition to the release of hormones (3). It can also decrease several complications, such as necrotizing enterocolitis (NEC), prolonged hospitalization, sepsis, and problems related to prolonged total parenteral nutrition (3, 4). Therefore, use of strategies to increase the feeding tolerance seems necessary.
Massage is defined as the mechanical manipulation of soft tissues via rhythmic pressure to increase health and well-being. Generally, infant massage involves passive touch (5). Previous studies have shown that massage has several benefits for infants, such as modified sleep patterns, weight gain, and improved GI tract function and development (4). It also results in weight gain and decreased hospital stay in premature infants (6). Diego et al in 2007 indicated that a daily 15-minute massage of premature infants for five days resulted in increased vagal activity and gastric motility (7). On the other hand, increased vagal activity can lead to further food absorption because of higher gastric motility and increased level of hormones associated with food absorption (6).
Up to present, several studies have investigated the effect of massage for premature infants and focused on the effects of systemic massage. In this regard, Kazemian et al. in 2017 found that systemic massage causes weight gain and reduces the length of hospital stay in infants with very low birth weight (8). However, the effect of abdominal massage has been less studied.
2. Objectives
This study aimed to investigate the effect of abdominal massage on the feeding tolerance of neonates with very low birth weight.
3. Methods
3.1. Study Design and Participants
This randomized open-label trial was conducted on low-birth-weight neonates, who were hospitalized in the neonatal intensive care units (NICUs) of two tertiary university hospitals in Babol and Tehran, Iran, from March 2016 to March 2017. Randomization of the participants was performed through systematic sampling. Based on similar studies in the literature (9, 10), the total sample size was calculated to be 56, and the study had 80% power.
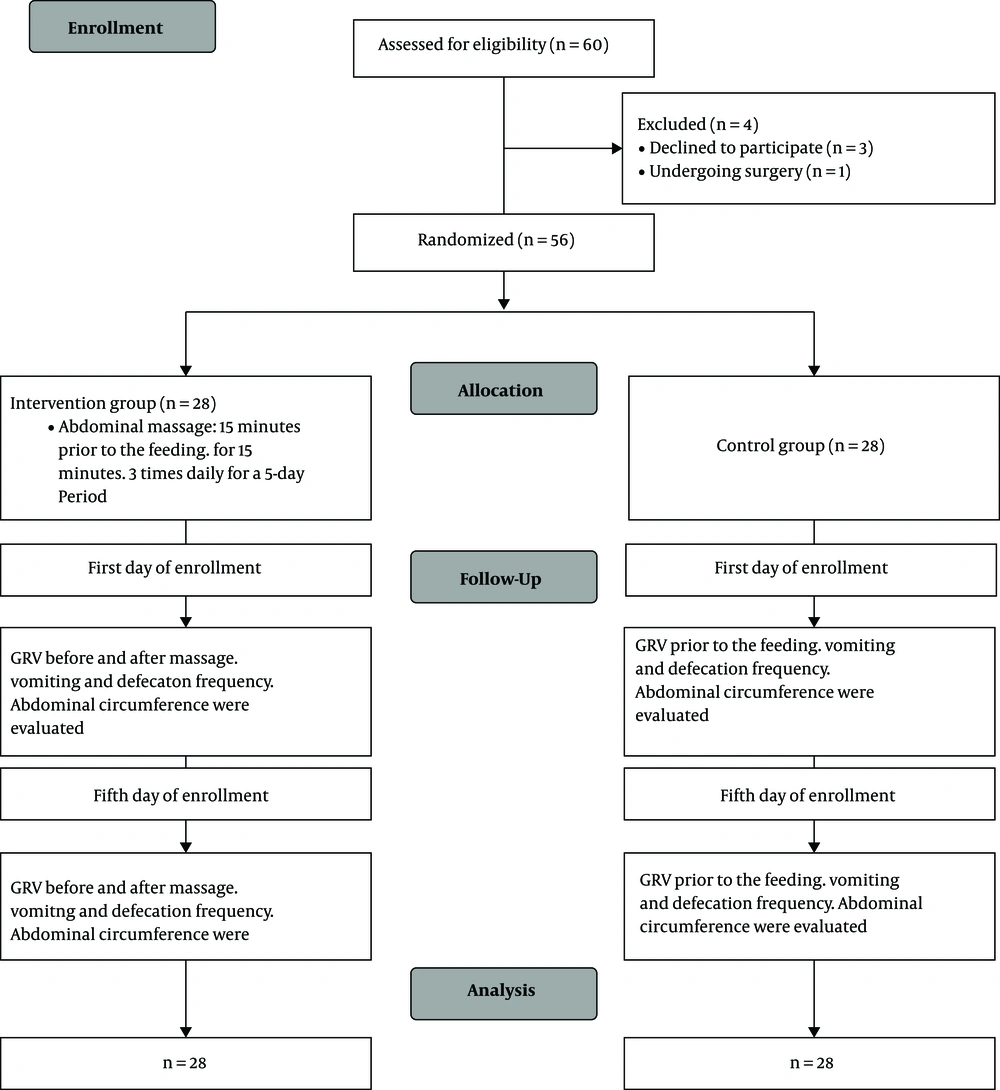
The inclusion criteria were as follows: (1) premature infants with an orogastric tube for enteral feeding in the NICU; (2) birth body weight below 1500 g; (3) gestational age of 28 - 32 weeks; (4) no history of intestinal obstruction, abdominal surgery, or NEC; and (5) no contraindications for abdominal massage. The exclusion criterion was defined as a history of major congenital malformations, including congenital heart diseases, gastrointestinal anomalies, hypoxic injury, respiratory failure with ventilator support, and gastroesophageal reflux, leading to respiratory apnea and feeding intolerance. Demographic data, including gestational age, birth weight, gender, age, and mode of feeding, were assessed in all subjects. The neonates were randomly assigned to two groups. The massage group received massage three times a day, while the control group received standard care (Figure 1).
3.2. Intervention
A nurse trained in massage therapy conducted the intervention, and a researcher performed the measurements. The researcher was blinded to the infants’ group assignments. The infants were not recruited in the study during the first five days of life if the feeding volume was less than 10 mL/kg/day. Abdominal massage was applied 15 minutes prior to feeding for 15 minutes three times a day for a five-day period. Massage was applied before feeding in order to prevent regurgitation of gastric contents.
Before massage, the gastric residual volume (GRV), presence of abdominal distension, and abdominal circumference were evaluated. GRV was measured by aspiration using a 5-mL syringe prior to each feeding episode. Positioning of the gastric tube was determined by auscultation with a stethoscope on the epigastric region while inserting 1 mL of air. During GRV measurements, the syringe piston was withdrawn slowly. When the stomach contents were no longer aspirated, measurement was repeated to make sure that the stomach is empty. Olive oil was used as the moisturizing lotion, and the infant was placed in the supine position with the head of bed elevated 30º - 45º during massage application.
We used the massage protocol previously described in the literature (1, 6, 10-12). Abdominal massage was applied in a clockwise direction over the intestines on the abdominal wall. The milk volume fed to preterm infants was 5 - 10 mL/kg/day, divided in 4 - 6 episodes per day. In case of the development of food tolerance, the amount was increased from 5 - 10 mL/kg/day to 140 - 160 mL/kg/day. During gavage feeding, no pressure was applied on the injector, as the flow rate continued due to gravity using the suspension technique. The weight of the infants was measured before 8:00 am every day for all participants. Abdominal massage was applied three times a day at 8:00 am, 2:00 pm, and 8:00 pm. GRV, presence of vomiting, and defection frequency were assessed every three hours (Figure 1).
3.3. Control Group
Feeding of infants in the control group was the same as the massage group. The control subjects received standard care. Data were collected in the same manner as the massage group.
3.4. Ethical Considerations
This study was approved by the Ethics Committee of Babol University of Medical Sciences (IRCT20180103038205N1). After presenting the necessary information to the families of the participants, written consent forms were obtained from all of the participants.
3.5. Statistical Analysis
Data were analyzed in SPSS version 22. Qualitative variables were analyzed using chi-square test or Fisher’s exact test. Independent and paired t-tests was also used for comparing the mean values. P value less than 0.05 was considered statistically significant.
4. Results
A total of 60 patients were considered eligible for this study. One patient was excluded due to surgery, and three refused to participate in the study. Fifty-six patients, including 28 patients in the massage group and 28 patients in the control group, were evaluated in this study. The results showed that 47% of subjects in the massage group and 50% of subjects in the control group were female. There was no significant difference between the massage and control groups regarding gender, birth weight, age, feeding mode, and gestational age (P = 0.711, 0.076, 0.082, 0.612, and 0.629, respectively) (Table 1). However, there was a significant difference in weight between the groups (P = 0.012), which is attributable to the randomized sampling of infants with different body weights (Table 1).
| Variable | Massage Group, No. (%) | Control Group, No. (%) | P Value |
|---|---|---|---|
| Gender | 0.711 | ||
| Male | 15 (53) | 14 (50) | |
| Female | 13 (47) | 14 (50) | |
| Birth weight, g | 0.076 | ||
| < 1000 | 6 (22) | 12 (42) | |
| 1000 - 1500 | 22 (78) | 16 (58) | |
| Age, d | 0.082 | ||
| < 10 | 21 (75) | 18 (63) | |
| > 10 | 7 (25) | 10 (37) | |
| Body weight, g | 0.012 | ||
| < 1000 g | 11 (39) | 14 (50) | |
| 1000 - 1500 | 17 (61) | 14 (50) | |
| Feeding mode | 0.612 | ||
| Breast milk | 25 (90) | 25 (90) | |
| Formula | 2 (7) | 1 (3) | |
| Breast milk and formula | 1 (3) | 2 (7) | |
| Gestational age | 0.629 | ||
| < 30 weeks | 16 (58) | 19 (68) | |
| > 30 weeks | 12 (42) | 9 (32) |
Based on the comparison of measurements on the first and fifth days, GRV before massage, GRV after massage, vomiting frequency, defecation frequency, and abdominal circumference changed significantly in the massage group (P = 0.001, 0.003, < 0.001, < 0.001, and < 0.001, respectively) (Table 2). On the other hand, GRV, vomiting frequency, defecation frequency, and abdominal circumference did not change significantly in the controls (P = 0.06, 0.264, 0.421, and 0.07, respectively) (Table 3).
| Variable/Time | Mean ± Standard Deviation | P Value |
|---|---|---|
| GRV prior to massage | ||
| Day 1 | 0.51 ± 0.59 | 0.001 |
| Day 5 | 0.16 ± 0.12 | |
| Vomiting frequency | ||
| Day 1 | 1.25 ± 0.79 | < 0.001 |
| Day 5 | 0.07 ± 0.26 | |
| Abdominal circumference | ||
| Day 1 | 21.97 ± 1.91 | < 0.001 |
| Day 5 | 21.30 ± 1.74 | |
| Defecation frequency | ||
| Day 1 | 1.89 ± 1.52 | < 0.001 |
| Day 5 | 3.78 ± 0.73 | |
| GRV following massage | ||
| Day 1 | 0.15 ± 0.24 | 0.003 |
| Day 5 | 0.004 ± 0.009 |
| Variable/Time | Mean ± Standard Deviation | P Value |
|---|---|---|
| GRV | 0.06 | |
| Day 1 | 0.39 ± 0.20 | |
| Day 5 | 0.83 ± 0.33 | |
| Vomiting frequency | 0.264 | |
| Day 1 | 1.53 ± 0/96 | |
| Day 5 | 1.85 ± 1.14 | |
| Abdominal circumference | 0.07 | |
| Day 1 | 21.64 ± 2.21 | |
| Day 5 | 22.49 ± 2.30 | |
| Defecation frequency | 0.421 | |
| Day 1 | 1.25 ± 0.75 | |
| Day 5 | 1.07 ± 0.72 |
5. Discussion
The present findings indicated the significant decrement of GRV, vomiting frequency, and abdominal circumference and the significant increment of defecation frequency in the massage group on the fifth day, compared to the first day of massage application. However, none of these variables changed significantly in the control group at the end of the study.
Immaturity of GI tract and feeding intolerance are common problems among premature infants. The GI tract of preterm infants has immature movements and lower digestive and absorptive abilities, compared to term infants. The presence of GRV and abdominal distension are signs of feeding intolerance among premature infants (10). Similar to our findings, Field et al. in 1986 reported accelerated gastric emptying, decreased GRV, and increased feeding tolerance in infants who received massage therapy (13). Moreover, Uysal et al. in 2012 investigated the effect of massage on GRV in 80 premature infants. They reported that 30% of subjects in the control group and 2.5% of subjects in the massage group had increased GRV at the end of the study (14).
In 2014, Tekgunduz et al. evaluated the effect of massage in 27 preterm infants at 28 - 32 weeks of gestation with a birth weight of 1000 - 1750 g (12). They applied massage for 15 minutes twice a day for five days. It was found that GRV decreased significantly at the end of the fifth day (12). Moreover, Kaisa et al. in 2017 reviewed the effects of massage on vagal activity and gastric mobility, as well as transcutaneous bilirubin level. They reported that in infants who received massage therapy, gastric mobility increased significantly during and after massage, which was associated with weight gain and vagal tone (15).
Uysal et al. also found that the abdominal circumference increased in 20% of subjects in the control group and 2.5% of subjects in the massage group. Increased vomiting frequency was observed in 10% of controls and none of subjects in the massage group (14). Their findings are in accordance with the findings of the present study and the study by Tekgunduz et al. (12). In line with our findings, Kaisa et al. reported a significant increase in the frequency of defecation in the massage group (15).
5.1. Conclusions
The effect of abdominal massage prior to enteral feeding of preterm infants was evaluated in this study. The results indicated a significant decrement in GRV, vomiting frequency, and abdominal circumference and a significant increment in defecation frequency among premature infants who received abdominal massage. Therefore, abdominal massage before enteral feeding results in less abdominal distension and GRV and is recommended for infants with very low body weights.