Abstract
Context:
Childhood obesity has become one of the most concerning public health issues and several innovative strategies are being applied to tackle the issue. Reformulation of children-oriented food products may play a role in improving childhood obesity. However, there is not sufficient evidence that shows the effectiveness of this policy. This paper provides a systematic review of the evidence to examine the efficacy of food product reformulation on calorie intake and weight modification of children with obesity.Evidence Acquisition:
A comprehensive literature search was undertaken for different types of studies. PubMed, Cochrane Library Database, EMBASE and SCOPUS were referred to as the source of literature.Results:
Seven thousand four hundred and three results were entered into our study for screening and evaluation. Our study showed that there was no clear evidence that supported the effectiveness of this intervention. However, some bodies of literature show calorie intake reduction, but no weight modification.Conclusions:
Although there is enough evidence to show that reformulation may promote healthy dietary patterns, its impact on weight status is not convincing. Long term running intervention needs to be applied to examine the possible implications of food reformulation policy on the weight status of the children.Keywords
1. Context
Recent statistics show that notable numbers of obese and overweight children and childhood obesity have become one of the most concerning public health problems of the 21st century. According to the 2016 estimates, almost in four decades, the prevalence of obesity among school-age children and adolescents has increased more than ten times, reaching from 11 million to 124 million. The same statistics show that over 216 million people were overweight but not obesep (1). This global problem is affecting many countries, from low and middle-income to affluent. Lifestyle preferences and cultural and environmental factors have a determining impact on the growing prevalence of childhood obesity. Most of the children are now living in an obesogenic environment, particularly in urban settings (2).
Early childhood is an important part of the life span for dietary habits and pattern formation and critical time for interventions for preventing overweight and obesity. For properly addressing dietary patterns and behaviors, it is crucial to understand the underlying factors causing these behaviors and patterns and implement evidence-based interventions (3). A poor and unbalanced diet is one of the major underlying causes of childhood overweight and obesity as well as widespread and rapidly growing consumption of high calorie and less nutritive and unhealthy foods (4) and sugar-sweetened beverages (SSBs). Food products have been recognized as an important cause of increased obesity prevalence in all ages, particularly in childhood (5). Several attempts and initiatives, including food reformulation, also have been ongoing to reduce the calorie content of packaged foods. However, there is a lack of robust evidence that indicates adopting food reformulation policies to what extent could prevent or halt the rise in obesity (6, 7).
A global shift in dietary pattern and food supply towards increased consumption and accessibility of affordable and energy-dense foods, along with the seductive marketing of the food products, is recognized as one of the main contributing factors of worldwide obesity. This trend has highlighted food supply systems as well as the food industry and its substantial role in the obesity prevalence (8). Food industries have taken numerous voluntary initiatives, such as reformulation, fortification, and functionalization of food products, as a part of their social responsibility agenda and commitments to improve the nutritional value of the products and to provide healthier choices for consumers (6).
The United States and several European countries have formulated and adopted several contextual and community-based programs that may help prevent the rise of childhood obesity, including in-school policies (9), regulating child-oriented calorie-dense food products advertisement (10), restricting the youth access to SSBs during school days, unhealthy food taxation aiming to address the burden of obesity and non-communicable diseases (NCDs) (11) and reformulating packaged food products to reduce total calorie intake by consumers (7, 12).
It is assumed that decreasing total calorie intake from high-calorie food products could help to halt the rise of obesity prevalence. Reformulation of foods and beverages with high per-capita consumption in order to modify the components associated with high caloric content has been recognized as one of the key emerging strategies and structural-based policies to reduce calorie intake by the population (6, 7).
The global market share of child-oriented food products is remarkable and high-calorie food products with low nutritional value make up a lion share of commercially promoted products (13). Childhood obesity: A plan for action in the United Kingdom (14), the Healthy Weight Commitment Foundation of the United States (7), the Charters of Voluntary Engagement of the French government (15) and Brazilian government agreement with representatives of the food industry to voluntarily reduce the sugar content in their products (16) are among significant policies to promote public health and improve food environments in the countries of interest. Food systems and major dietary patterns are already affected by leading packaged and processed food products and such policies welcomed by the food industry and key players in the food and health sectors. Meanwhile, it is evident that marketing unhealthy child-oriented food products negatively impacts children’s eating behaviors (13). This marketing procedure is a problem of serious concern as taste and dietary habits in children would develop through repeated exposure to these kinds of foods and would cause micronutrient deficiencies, as they usually have less nutritive value (17).
Developed food preferences during childhood are likely to persist through life and can, therefore, cause both short and long-term outcomes for health and weight status (18). It is acknowledged that tackling childhood obesity and overweight is unlikely to succeed if supportive structural and environmental factors, such as food supply, are not appropriately addressed (19). Several stakeholders are involved in creating the obesogenic environment. Governments, private sector and civil society organizations, donors, and several other stakeholders could have a crucial role in modifying the obesogenic environment, which in turn needs transparency, public accountability, social responsibility and conflict of interest management (20).
Reformulation of food products is a practical process, intending to improve the nutritional properties of food products by cutting down components associated with negative health effects such as fat, salt and sugar, or by decreasing portion size while keeping or improving their nutrient contents with positive health benefits and protecting their organoleptic characteristics such as color, taste, texture and shelf life (8). There is increasing attention toward interventions targeting the reformulation of processed foods to improve the nutritional environment (21, 22). However, the potential effectiveness of children-oriented food reformulation policies in reducing calorie intake and tackling childhood obesity is not clear enough. Although several studies show that increased consumption of high-calorie food and beverages will lead to the prevalence of overweight and obesity, there is limited evidence supporting the effectiveness of the reformulation policy in halting the increase in childhood obesity at the population level (23). This paper provides a systematic review by reporting the results of food reformulation interventions aimed at reducing food products' calorie content in weight modification in children.
2. Evidence Acquisition
2.1. Participants
In this systematic review, original studies performing on 2-year-old to 19-year-old children of any nationality who were of either normal BMI, overweight or obese without any underlying disease which might have interfered with their weight status, and who had specific anthropometric characteristics were considered. Children of normal BMI were also considered in the study as the aim of the study was to investigate both the preventive effect of the intervention and its impact on weight modification in the children.
2.2. Intervention
All interventions with any deliberate approaches to processed food reformulation or revising food standards that reduce their calorie content or total calorie intake by children were considered in this review.
2.3. Outcome Measure
This review aimed to examine the following outcome measures systematically:
Primary Outcomes: BMI and weight change.
Secondary Outcomes: Prevalence of overweight and childhood obesity and adiposity.
All short term (measured immediately after intervention) and long-term (at least six months after completion of the intervention) were included in this review.
2.4. Study Design
The studies included in this review were randomized controlled trials (RCT) or comparator group studies, controlled before and after studies (CBA), interrupted time series (ITS) and comparisons with historical controls, ecological studies, policies, cohort studies or national trends in our searching strategy.
2.5. Language and Date Restrictions
Searches included publications in English only, published to date (March 2020).
3. Search Strategy of Literature Sources
The strategy and procedure followed in the present review was PRISMA guideline. A two-step search strategy was applied for searching the databases. The first phase was a comprehensive search using identified keywords and index terms undertaken in PubMed, SCOPUS, Cochrane Library Database and EMBASE as well as an unstructured search in Google Scholar, through which the following keywords were identified:
Participants: Childhood obesity, pediatric obesity, overweight children, school children, pre-school children and adolescent obesity.
Intervention: Food reformulation, food products reformulation, packaged foods reformulation, beverage reformulation, drink reformulation, food standard, fat content reduction, sugar content reduction, calorie content reduction, food calorie restriction and food industry standards.
Outcome: Energy intake, calorie intake, excess calorie, weight change, weight modification, obesity modification and weight loss.
The second phase was a structured search in PubMed, SCOPUS, Cochrane Library Database, EMBASE and an unstructured search in Google Scholar on 19 July 2020 (Appendix A in Supplementary File). MeSH terms in different combinations were applied in all databases to best cover all relevant and existing literature. All studies identified during a comprehensive search and search of the reference lists were examined for relevance to the review based on information provided in their titles and abstracts. In the case of their relevancy, the full text of the papers was reviewed for further analysis of whether the studies met the inclusion criteria.
4. Methodological Quality
A tailored critical appraisal skills program (CASP) appraisal tool for case-control studies and randomized controlled trials was applied to evaluate and assess the quality of the studies based on the study objectives. Ten questions of the appraisal tools were used to score the quality of the included studies. Two CASP questions were not considered during evaluation of the studies, including “Can the results be applied to the local population?” and “Do the results of this study fit with other available evidence?”, as the scope of this review was not local context and limited included studies and their heterogeneity in terms of results (Table 1). The quality of the studies was evaluated based on the data relevant to this review and may not represent the overall quality of the studies. The included studies independently were scored by a team of two researchers who managed any disagreements through consensus. Differences between outcomes concerning study quality, setting, populations and, where applicable, the intervention's nature were qualitatively analyzed, and each of the selected criteria against the review evidence was systematically considered. As only a limited number of studies met the inclusion criteria, none of the studies were excluded based on their quality scores (Table 2).
Critical Appraisal Skills Program (CASP) Questions Used to Evaluate the Included Studies (Presented in Table 2)
| Number | Questions |
|---|---|
| 1 | Did the study address a clearly focused issue? |
| 2 | Did the authors use an appropriate method to answer their question? |
| 3 | Was the study recruited in an acceptable way? |
| 4 | Was the exposure accurately measured to minimize bias? |
| 5 | Was the outcome accurately measured to minimize bias? |
| 6 | Have the authors identified all important confounding factors? Have they taken account of the confounding factors in the design and/or analysis? |
| 7 | Was the follow-up of subjects complete enough? |
| 8 | Was the follow up of subjects long enough? |
| 9 | How precise are the results? |
| 10 | Do you believe the results? |
Study Characteristics Intervention Settings and Outcomes (Structured by Year of Publication)
| Study Information | Participants | Sample Size | Design | Method For Analysis | Diagnostic Criteria | Intervention Type | Intervention Period | Outcome |
|---|---|---|---|---|---|---|---|---|
| Rehm et al. (24), USA CASP 8/10 | Children and adolescent, 2 - 19 y. ((NHANES: 2001 - 2002 and 2003 - 2004) | 8112 | Cross sectional | survey-weighted linear regression models and chi-square | BMI percentiles by age and gender | Replacement of whole, reduced-fat, and flavored milk with skim and low-fat milk | 2001 - 2004 | 64 - 113 kilocalorie decrease in total calorie consumption |
| Meghan et al., USA CASP 7/10 | Children and adolescent, 2 - 18 y. (NHANES: 2007 - 2008 and 2012 - 2015) | 16692 + 2966 | Cross sectional | Would be released after NHANES 2012 - 2105 | Changes in total calories sold, average daily calories purchased and top sources of calories purchased and changes in average daily calories consumed and top sources of calories | Total calorie reduction in packaged food products | 2007 - 2015 | No outcome regarding the weight statues of children released |
| Hendrie and Golley (25), Australia CASP 8/10 | Children 4 - 13 y. | 145 | Cluster randomized controlled trial | Unadjusted univariate analyses, maximum likelihood mixed models | Not reported | Shifting from regular-fat to low-fat dairy products | 24 weeks | No significant group differences in total energy or adiposity measures |
| Wang et al. (26), USACASP 9/10 | Children 2 - 19 y. | 3098 | Cross Sectional | multivariate fixed-effects regression models and time-varying covariates | Changes in the consumption of SSBs and other beverages and changes in total energy intake (TEI) of the same individual. | replacing SSBs with alternatives | 2 nonconsecutive 24-hour dietary recalls from the 2003 - 2004 | Each 1% of beverage replacement was associated with 6.6-kcal lower TEI |
| Childhood obesity: A plan for action, Department of Health, 2016, UK | National health policy | N/A | Policy statement | N/A | The percentage decrease in sugar and calorie content of food products | Sugar and calorie reduction in food products | 4 years | A 2% reduction in sugar content of foods. No outcome regarding the weight statues of children released |
| Sugar content reduction in food and beverages, 2018, Brazil | National health policy | N/A | Policy statement | N/A | The percentage decrease in sugar and calorie content of food products | Sugar reduction (144,000 tons) in food products from food and beverages | 4 years | To be released |
5. Data Extraction
AMB, NK and AHR developed the study question and search strategies and imported the search results in Endnote (X8 Ed.). All Authors were involved in the screening of the results and extracting the data. AMB and AHR prepared the final report. Discrepancies at the designing the study, screening and data extraction stages were resolved by discussion.
Data, observing methodology, intervention type, and outcomes were systematically extracted using a customized extraction tool developed by the JBI (2) which includes general information of the study, sample size, design, population, methods for analyzing, diagnostic criteria for obesity, adjusted factors, intervention type, intervention length and outcome(s). Decisions regarding including data in the tables were made by two research members who were well-experienced in designing and conducting research projects in the field of childhood obesity.
6. Results
Based on our search strategy, 7601 results from the mentioned databases were entered into our study. After removing duplications, 7403 results were examined through reviewing their titles and abstracts. Twenty four studies that reported food reformulation impact on childhood obesity were considered for further evaluation based on their full texts. PRISMA Flow chart of included studies is presented in Figure 1.
PRISMA Flow chart of included studies. Flow chart indicates 7403 abstracts were examined further to excluding the duplicates, followed by exclusion of 7363 abstracts due to irrelevant titles and abstracts. 40 full text articles were assessed for eligibility and then 34 full text articles were further excluded.
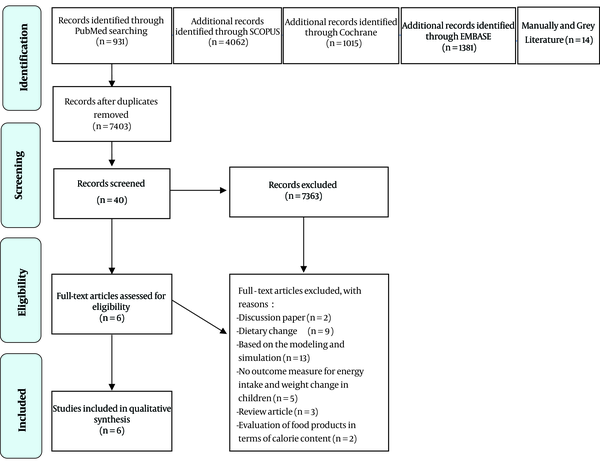
Further to the evaluation of the 56 full-texts of the included studies, two discussion papers were excluded from the review (8, 27). Nine papers were further excluded as they mainly focused on dietary change rather than the change in the formulation of food products (28-37). Four papers using simulation and modeled study method examined the possible impacts of industry-wide food and beverage reformulations in total calorie intake (38-50), which are not entirely in line with the scope of the review. Five papers had no outcome measure for energy intake and weight change in children (51-55), one review paper (23, 56, 57) and two, which were based on the total calorie content of food products rather than their consumption by children (58, 59). At the end of the screening, six articles were partially kept for further evaluation; still, three of them did not completely meet our criteria for data extraction as they did not directly address products reformulation, instead examined low-calorie food options’ impact on total calorie intake in children (24-26). Two reformulation policies and an action plan were considered for further evaluation at the final step. Wang et al., by reviewing the National Health and Nutrition Examination Survey dietary recalls from 2003 to 2004 in the United States, showed that replacing SSBs consumption with water will decrease total calorie intake and every 1% beverage substitution was correlated with 6.6-kcal lower total calorie intake. They also reported that replacing total SSBs consumption with water may decrease 235 kcal/d intake (26). In 2016, the government of the UK began implementing an action plan to tackle childhood obesity, in line with Public Health England (PHE). The plan aimed to promote a sugar reduction in child-oriented food products by 20% by 2020, with a 5% reduction by 2017 (14). However, the policy evaluation for the first year of the implementation showed a 2% reduction in sugar content of food products and the impact of the policy on obesity prevention had not been estimated. Simultaneously, the UK government started a calorie reduction program since 2017, which challenges food and drink and retailers to reduce the calorie content of foods by 20%, which are commonly consumed by children by 2024 (60). The Brazilian government in 2018 has also implemented a voluntary food reformulation policy, to cut out 144,600 tons of sugar from food products by 2022. However, no report or analysis of the effectiveness of this policy has been published yet (16).
Hendrie and Golley (25) assessed the effect of dietary intake and health benefits of replacing regular dairy products with low-fat ones among 4 - 13 years old children in New Zealand. After a 24-week intervention, it was found that promoting low-fat dairy products intake may lead to lower saturated fat intake by children but did not reduce total calorie intake or modify adiposity of the participants (25). Rehm et al. (24) estimated the potential nutritional impact of the substitution of whole and reduced-fat milk with low-fat and skimmed milk among children of 2 - 19 years old in the United States using a cross-sectional modeling study. They used data from the National Health and Nutrition Examination survey between 2001 - 2002 and 2003 - 2004. They reported that the replacement might lead to a projected cut in total energy intake by 113 kcal/d and reduced total energy intake from saturated fat (24). One prospective study directly examined the effectiveness of the food products’ reformulation and calorie cuts, specifically in modifying obesity, but the result of the intervention has not been released (7).
7. Discussion
Ironically, childhood obesity and the social responsibility measures of the food industry are, at least in several cases, in paradox. Although dietary guidelines recommend none-processed and convenient food products intake for different age groups, from a business perspective, food industries try to produce healthy processed food choices to ensure health-conscious consumers’ satisfaction and meet their social responsibility (61). Our review showed that the reformulation of food products is an innovative and new approach to improve nutrition status. However, there is a lack of clear evidence that explicitly show the real impact of this policy on the weight status of target groups (Table 2). Meanwhile, in some cases, the impact of the responsibility deals of food producers for decreasing the calorie content of food products have not yielded expected results (62). In most cases, the food monitoring system does not effectively track brand-specific changes in food composition or sales to understand its unique impact. Accordingly, the evaluation of the reformulation and its impact on the children’s diet required establishing a system that links sales and purchases of consumer packaged food products to individual dietary intake (7).
Most of the studies regarding the impact of cutting down the total calorie received from packaged foods have been conducted in the USA (7, 24, 26), United Kingdom (6) and Australia (25). The food products targeted for intervention vary based on the primary energy source of daily food intake. This review showed that by replacing whole fat milk and chocolate milk with skimmed milk, 64 - 113 kilocalories per day could be removed from children’s daily diet. However, the impact of this change on obesity prevalence and weight change is not assessed in this study (24). Evidence from another study showed that replacing whole and flavored ones with low fat or skimmed alternatives could have an impact on total calorie consumption provided by dairy products. A 24-week intervention change to low-fat dairy foods could significantly reduce the total energy intake from fats and decrease total saturated fats received from the diet. At the same time, there was no significant decrease in total calorie consumption as the intervention group derived a significantly greater percentage of energy from carbohydrates at week 24 (25). The point here is that, although dairy products are manufactured through an industrial process, the procedure could not be considered a complete reformulation procedure adopted by food industries as suppliers produce milk products with different fat content just as options for consumers.
High intake of SSBs also is highly seen by policymakers in controlling their negative health impacts. Per-capita daily caloric contribution from SSBs has been increased during recent decades, especially among children and there is a dramatic increase among children aged 6 to 11 years (63). Most policies for limiting total calorie received from SSBs have focused on improving food preferences and choices in children rather than structural-based intervention as reformulation (1, 33). The present review showed that according to NHANES (2003 - 2004) study replacing SSBs in schools by water could significantly decrease total calorie consumption; each 1% of beverage replacement was associated with 6.6-kcal lower total energy intake, a reduction not buffered by compensatory increases in other dietary sources of energy (26).
The Healthy Weight Commitment Foundation (HWCF), which made up of 16 leading consumer packaged food products manufacturers, voluntarily pledged to remove 1 trillion calories from their products together by 2012 (against a 2007 baseline), followed by 1.5 trillion calories reduction by 2015. This campaign has been launched based on the evidence which shows calories received from packaged foods provide 68.1% of total calories consumed by children and adolescents of 2 - 18 years. These results suggest that the 16 HWCF companies account for approximately 25% of the total reported calories consumed by this target group. The main food sources of calories (day/per capita) from stores and vending machines include grain-based desserts (134 calories), savory snacks (120 calories), pasta and noodle dishes (111 calories), bread (105 calories), and ready-to-eat cereals (83 calories). The top beverage sources of calories (day/per capita) from stores and vending machines include fluid milk (143 calories), SSBs (102 calories), and fruit juice (56 calories). The effect of the campaign on the prevalence of childhood obesity has not been estimated (7).
The Brazilian government in 2018 has also implemented a food reformulation policy, which is a voluntary commitment to reduce the sugar content in food products. About 87% of food industries have signed the agreement and a total of 144,600 tons of sugar is expected to be reduced from the processed food products by 2022. The results of the policy have not been released yet (16).
The present study also showed that applying food products reformulation policies to reduce weight gain trends and possibly weight modification is going to be considered one of the highly accepted interventions. On the other hand, the food industries are increasingly welcoming this strategy to realize their social responsibilities. However, there is not enough evidence showing its direct and indirect impacts on weight regulation. Although there is enough evidence that shows reformulation may promote healthy dietary patterns and NCDs prevention (23, 33) and promotes demand for healthier food and drinks (14), its impact on weight status is unclear as other sources of calorie intake may be increased in the diet (25). Consumers may assume that they have already received fewer calories via reformulated food products. To maximize the effect of the reformulation strategy, the simultaneous implementation of fiscal policies, such as selective taxation on high-calorie packaged foods, may help reduce childhood obesity (64). Moreover, to examine the impact of this intervention, long-term running intervention needs to be applied.
Several parallel public health policies are needed to make a significant impact on childhood obesity. It can also be argued that high-calorie food reformulation alone would not necessarily bring about improved childhood obesity. Food reformulation policies require a commitment not only from the food industry but also from food retailers, restaurants and franchises. Since the food reformulation policies are not usually mandatory, achieving the targets may not be guaranteed (65). Several underlying dietary causes are leading to obesity, which can be rooted in improper food choices. On the other hand, food choice itself has several social and economic components (66-68) and there should be multilateral and integrative policies to address childhood obesity comprehensively (69).
References
-
1.
Luger M, Lafontan M, Bes-Rastrollo M, Winzer E, Yumuk V, Farpour-Lambert N. Sugar-Sweetened Beverages and Weight Gain in Children and Adults: A Systematic Review from 2013 to 2015 and a Comparison with Previous Studies. Obes Facts. 2017;10(6):674-93. [PubMed ID: 29237159]. [PubMed Central ID: PMC5836186]. https://doi.org/10.1159/000484566.
-
2.
Munn Z, Tufanaru C, Aromataris E. JBI's systematic reviews: data extraction and synthesis. Am J Nurs. 2014;114(7):49-54. [PubMed ID: 25742352]. https://doi.org/10.1097/01.NAJ.0000451683.66447.89.
-
3.
Nixon CA, Moore HJ, Douthwaite W, Gibson EL, Vogele C, Kreichauf S, et al. Identifying effective behavioural models and behaviour change strategies underpinning preschool- and school-based obesity prevention interventions aimed at 4-6-year-olds: a systematic review. Obes Rev. 2012;13 Suppl 1:106-17. [PubMed ID: 22309069]. https://doi.org/10.1111/j.1467-789X.2011.00962.x.
-
4.
Malik VS, Schulze MB, Hu FB. Intake of sugar-sweetened beverages and weight gain: a systematic review. Am J Clin Nutr. 2006;84(2):274-88. https://doi.org/10.1093/ajcn/84.2.274.
-
5.
Ogden CL, Kit BK, Carroll MD, Park S. Consumption of sugar drinks in the United States, 2005-2008. US Department of Health and Human Services, Centers for Disease Control and …; 2011.
-
6.
Buttriss JL. Calorie reduction programme launched. Nutr Bull. 2018;43(2):106-11. https://doi.org/10.1111/nbu.12315.
-
7.
Slining MM, Ng SW, Popkin BM. Food companies' calorie-reduction pledges to improve U.S. diet. Am J Prev Med. 2013;44(2):174-84. [PubMed ID: 23332336]. [PubMed Central ID: PMC3583299]. https://doi.org/10.1016/j.amepre.2012.09.064.
-
8.
van Raaij J, Hendriksen M, Verhagen H. Potential for improvement of population diet through reformulation of commonly eaten foods. Public Health Nutr. 2009;12(3):325-30. [PubMed ID: 18671891]. https://doi.org/10.1017/S1368980008003376.
-
9.
Welker E, Lott M, Story M. The school food environment and obesity prevention: Progress over the last decade. Curr Obes Rep. 2016;5(2):145-55. [PubMed ID: 27066793]. https://doi.org/10.1007/s13679-016-0204-0.
-
10.
Harris JL, Graff SK. Protecting young people from junk food advertising: implications of psychological research for First Amendment law. Am J Public Health. 2012;102(2):214-22. [PubMed ID: 22390435]. [PubMed Central ID: PMC3483979]. https://doi.org/10.2105/AJPH.2011.300328.
-
11.
Villanueva T. European nations launch tax attack on unhealthy foods. CMAJ. 2011;183(17):E1229-30. [PubMed ID: 22025654]. [PubMed Central ID: PMC3225438]. https://doi.org/10.1503/cmaj.109-4031.
-
12.
Tedstone A, Targett V, Mackinlay B, Owtram G, Coulton V, Morgan K, et al. Calorie reduction: the scope and ambition for action. Publ Health Engl London. 2018.
-
13.
Boyland EJ, Halford JC. Television advertising and branding. Effects on eating behaviour and food preferences in children. Appetite. 2013;62:236-41. [PubMed ID: 22421053]. https://doi.org/10.1016/j.appet.2012.01.032.
-
14.
HM Government. Childhood obesity: a plan for action. HM Government London, UK; 2016.
-
15.
Vandevijvere S, Vanderlee L. Effect of Formulation, Labelling, and Taxation Policies on the Nutritional Quality of the Food Supply. Curr Nutr Rep. 2019;8(3):240-9. [PubMed ID: 31321705]. https://doi.org/10.1007/s13668-019-00289-x.
-
16.
Brazil Gov. Brazil to cut 144,000 tons of sugar from food and beverages. 2018.
-
17.
Carpentier A, Pataky Z, Bobbioni-Harsch E, Golay A. [Micronutrient deficiency in obesity]. Revue Medicale Suisse. 2013:666-9. French.
-
18.
Cornwell TB, McAlister AR. Alternative thinking about starting points of obesity. Development of child taste preferences. Appetite. 2011;56(2):428-39. [PubMed ID: 21238522]. https://doi.org/10.1016/j.appet.2011.01.010.
-
19.
Waters E, Swinburn BA, Seidell JC, Uauy R. Preventing childhood obesity: evidence policy and practice. Aging Cancer. 2010. https://doi.org/10.1002/9781444318517.
-
20.
Kraak VI, Harrigan PB, Lawrence M, Harrison PJ, Jackson MA, Swinburn B. Balancing the benefits and risks of public-private partnerships to address the global double burden of malnutrition. Public Health Nutr. 2012;15(3):503-17. [PubMed ID: 22014282]. https://doi.org/10.1017/S1368980011002060.
-
21.
Combris P, Goglia R, Henini M, Soler LG, Spiteri M. Improvement of the nutritional quality of foods as a public health tool. Public Health. 2011;125(10):717-24. [PubMed ID: 21890152]. https://doi.org/10.1016/j.puhe.2011.07.004.
-
22.
Griffith R, O'Connell M, Smith K. The importance of product reformulation versus consumer choice in improving diet quality. Economica. 2017;84(333):34-53. https://doi.org/10.1111/ecca.12192.
-
23.
Hu FB. Resolved: there is sufficient scientific evidence that decreasing sugar-sweetened beverage consumption will reduce the prevalence of obesity and obesity-related diseases. Obes Rev. 2013;14(8):606-19. [PubMed ID: 23763695]. [PubMed Central ID: PMC5325726]. https://doi.org/10.1111/obr.12040.
-
24.
Rehm CD, Drewnowski A, Monsivais P. Potential population-level nutritional impact of replacing whole and reduced-fat milk with low-fat and skim milk among US children aged 2-19 years. J Nutr Educ Behav. 2015;47(1):61-68 e1. [PubMed ID: 25528079]. [PubMed Central ID: PMC4315137]. https://doi.org/10.1016/j.jneb.2014.11.001.
-
25.
Hendrie GA, Golley RK. Changing from regular-fat to low-fat dairy foods reduces saturated fat intake but not energy intake in 4-13-y-old children. Am J Clin Nutr. 2011;93(5):1117-27. [PubMed ID: 21430121]. https://doi.org/10.3945/ajcn.110.010694.
-
26.
Wang YC, Ludwig DS, Sonneville K, Gortmaker SL. Impact of change in sweetened caloric beverage consumption on energy intake among children and adolescents. Arch Pediatr Adolesc Med. 2009;163(4):336-43. [PubMed ID: 19349562]. https://doi.org/10.1001/archpediatrics.2009.23.
-
27.
Food WHO Better. Nutrition in europe: A progress report monitoring policy implementation in the WHO european region. Entre Nous Cph Den. 2018.
-
28.
O'Connor TM, Yang SJ, Nicklas TA. Beverage intake among preschool children and its effect on weight status. Pediatrics. 2006;118(4):e1010-8. [PubMed ID: 17015497]. https://doi.org/10.1542/peds.2005-2348.
-
29.
Briefel RR, Wilson A, Gleason PM. Consumption of low-nutrient, energy-dense foods and beverages at school, home, and other locations among school lunch participants and nonparticipants. J Am Diet Assoc. 2009;109(2 Suppl):S79-90. [PubMed ID: 19166676]. https://doi.org/10.1016/j.jada.2008.10.064.
-
30.
Sichieri R, Paula Trotte A, de Souza RA, Veiga GV. School randomised trial on prevention of excessive weight gain by discouraging students from drinking sodas. Public Health Nutr. 2009;12(2):197-202. [PubMed ID: 18559131]. https://doi.org/10.1017/S1368980008002644.
-
31.
Kleiman S, Ng SW, Popkin B. Drinking to our health: can beverage companies cut calories while maintaining profits? Obes Rev. 2012;13(3):258-74. [PubMed ID: 22070346]. [PubMed Central ID: PMC3420345]. https://doi.org/10.1111/j.1467-789X.2011.00949.x.
-
32.
Perlman SE, Nonas C, Lindstrom LL, Choe-Castillo J, McKie H, Alberti PM. A menu for health: changes to New York City school food, 2001 to 2011. J Sch Health. 2012;82(10):484-91. [PubMed ID: 22954168]. https://doi.org/10.1111/j.1746-1561.2012.00726.x.
-
33.
Briefel RR, Wilson A, Cabili C, Hedley Dodd A. Reducing calories and added sugars by improving children's beverage choices. J Acad Nutr Diet. 2013;113(2):269-75. [PubMed ID: 23351631]. https://doi.org/10.1016/j.jand.2012.10.016.
-
34.
Pourshahidi LK, Kerr MA, McCaffrey TA, Livingstone MB. Influencing and modifying children's energy intake: the role of portion size and energy density. Proc Nutr Soc. 2014;73(3):397-406. [PubMed ID: 24886909]. https://doi.org/10.1017/S0029665114000615.
-
35.
Turner-McGrievy GM, Hales SB, Baum AC. Transitioning to new child-care nutrition policies: nutrient content of preschool menus differs by presence of vegetarian main entree. J Acad Nutr Diet. 2014;114(1):117-23. [PubMed ID: 24144990]. https://doi.org/10.1016/j.jand.2013.07.036.
-
36.
Mesirow MS, Welsh JA. Changing beverage consumption patterns have resulted in fewer liquid calories in the diets of US children: National Health and Nutrition Examination Survey 2001-2010. J Acad Nutr Diet. 2015;115(4):559-66 e4. [PubMed ID: 25441966]. https://doi.org/10.1016/j.jand.2014.09.004.
-
37.
Libuda L, Kersting M, Alexy U. Consumption of dietary salt measured by urinary sodium excretion and its association with body weight status in healthy children and adolescents. Public Health Nutr. 2012;15(3):433-41. [PubMed ID: 21929845]. https://doi.org/10.1017/S1368980011002138.
-
38.
Gressier M, Privet L, Mathias KC, Vlassopoulos A, Vieux F, Masset G. Modeled dietary impact of industry-wide food and beverage reformulations in the United States and France. Am J Clin Nutr. 2017;106(1):225-32. [PubMed ID: 28592599]. https://doi.org/10.3945/ajcn.117.153361.
-
39.
Pigat S, Connolly A, Cushen M, Cullen M, O'Mahony C. A probabilistic intake model to estimate the impact of reformulation by the food industry among Irish consumers. Int J Food Sci Nutr. 2018;69(8):938-45. [PubMed ID: 29457511]. https://doi.org/10.1080/09637486.2018.1438375.
-
40.
Crino M, Herrera AMM, Ananthapavan J, Wu JHY, Neal B, Lee YY, et al. Modelled cost-effectiveness of a package size cap and a kilojoule reduction intervention to reduce energy intake from sugar-sweetened beverages in australia. Nutrients. 2017;9(9). [PubMed ID: 28878175]. [PubMed Central ID: PMC5622743]. https://doi.org/10.3390/nu9090983.
-
41.
Masset G, Mathias KC, Vlassopoulos A, Molenberg F, Lehmann U, Gibney M, et al. Modeled dietary impact of pizza reformulations in us children and adolescents. PLoS One. 2016;11(10). e0164197. [PubMed ID: 27706221]. [PubMed Central ID: PMC5051708]. https://doi.org/10.1371/journal.pone.0164197.
-
42.
Legato MJ. Gender-specific aspects of obesity. Int J Fertil Womens Med. 1997:184-97.
-
43.
Briggs AD, Mytton OT, Kehlbacher A, Tiffin R, Elhussein A, Rayner M, et al. Health impact assessment of the UK soft drinks industry levy: a comparative risk assessment modelling study. Lancet Public Health. 2017;2(1):e15-22. https://doi.org/10.1016/s2468-2667(16)30037-8.
-
44.
Ma Y, He FJ, Yin Y, Hashem KM, MacGregor GA. Gradual reduction of sugar in soft drinks without substitution as a strategy to reduce overweight, obesity, and type 2 diabetes: a modelling study. Lancet Diabetes Endocrinol. 2016;4(2):105-14. https://doi.org/10.1016/s2213-8587(15)00477-5.
-
45.
Hendriksen MA, Tijhuis MJ, Fransen HP, Verhagen H, Hoekstra J. Impact of substituting added sugar in carbonated soft drinks by intense sweeteners in young adults in the Netherlands: example of a benefit-risk approach. Eur J Nutr. 2011;50(1):41-51. [PubMed ID: 20429009]. https://doi.org/10.1007/s00394-010-0113-z.
-
46.
Husoy T, Mangschou B, Fotland TO, Kolset SO, Notvik Jakobsen H, Tommerberg I, et al. Reducing added sugar intake in Norway by replacing sugar sweetened beverages with beverages containing intense sweeteners - a risk benefit assessment. Food Chem Toxicol. 2008;46(9):3099-105. [PubMed ID: 18639604]. https://doi.org/10.1016/j.fct.2008.06.013.
-
47.
Yeung CHC, Gohil P, Rangan AM, Flood VM, Arcot J, Gill TP, et al. Modelling of the impact of universal added sugar reduction through food reformulation. Sci Rep. 2017;7(1):17392. [PubMed ID: 29234031]. [PubMed Central ID: PMC5727294]. https://doi.org/10.1038/s41598-017-17417-8.
-
48.
Pearson-Stuttard J, Hooton W, Critchley J, Capewell S, Collins M, Mason H, et al. Cost-effectiveness analysis of eliminating industrial and all trans fats in England and Wales: modelling study. J Public Health (Oxf). 2017;39(3):574-82. [PubMed ID: 27613767]. https://doi.org/10.1093/pubmed/fdw095.
-
49.
Allen K, Pearson-Stuttard J, Hooton W, Diggle P, Capewell S, O'Flaherty M. Potential of trans fats policies to reduce socioeconomic inequalities in mortality from coronary heart disease in England: cost effectiveness modelling study. BMJ. 2015;351:h4583. [PubMed ID: 26374614]. [PubMed Central ID: PMC4569940]. https://doi.org/10.1136/bmj.h4583.
-
50.
Temme EH, Millenaar IL, Van Donkersgoed G, Westenbrink S. Impact of fatty acid food reformulations on intake of Dutch young adults. Acta Cardiol. 2011;66(6):721-8. [PubMed ID: 22299382]. https://doi.org/10.1080/ac.66.6.2136955.
-
51.
Alberti PM, Perlman SE, Nonas C, Hadler J, Choe J, Bedell JF, et al. Effects of switching from whole to low-fat/fat-free milk in public schools-New York City, 2004-2009. Morbid Mortal W. 2010;59(3):70-3.
-
52.
Pomeranz JL, Teret SP, Sugarman SD, Rutkow L, Brownell KD. Innovative legal approaches to address obesity. Milbank Q. 2009;87(1):185-213. [PubMed ID: 19298420]. [PubMed Central ID: PMC2879172]. https://doi.org/10.1111/j.1468-0009.2009.00552.x.
-
53.
Elfhag K, Tynelius P, Rasmussen F. Sugar-sweetened and artificially sweetened soft drinks in association to restrained, external and emotional eating. Physiol Behav. 2007;91(2-3):191-5. [PubMed ID: 17434544]. https://doi.org/10.1016/j.physbeh.2007.02.005.
-
54.
Berkey CS, Rockett HR, Field AE, Gillman MW, Colditz GA. Sugar-added beverages and adolescent weight change. Obes Res. 2004;12(5):778-88. [PubMed ID: 15166298]. https://doi.org/10.1038/oby.2004.94.
-
55.
Perez-Escamilla R, Lutter CK, Rabadan-Diehl C, Rubinstein A, Calvillo A, Corvalan C, et al. Prevention of childhood obesity and food policies in Latin America: from research to practice. Obes Rev. 2017;18 Suppl 2:28-38. [PubMed ID: 28741904]. https://doi.org/10.1111/obr.12574.
-
56.
Australia NHFo. Rapid review of the evidence: Effectiveness of food reformulation as a strategy to improve population health. National Heart Foundation of Australia; 2012.
-
57.
Federici C, Detzel P, Petracca F, Dainelli L, Fattore G. The impact of food reformulation on nutrient intakes and health, a systematic review of modelling studies. BMC Nutr. 2019;5:2. [PubMed ID: 32153917]. [PubMed Central ID: PMC7050744]. https://doi.org/10.1186/s40795-018-0263-6.
-
58.
Savio S, Mehta K, Udell T, Coveney J. A survey of the reformulation of Australian child-oriented food products. BMC Public Health. 2013;13:836. [PubMed ID: 24025190]. [PubMed Central ID: PMC3847458]. https://doi.org/10.1186/1471-2458-13-836.
-
59.
Domenech-Asensi G, Merola N, Lopez-Fernandez A, Ros-Berruezo G, Frontela-Saseta C. Influence of the reformulation of ingredients in bakery products on healthy characteristics and acceptability of consumers. Int J Food Sci Nutr. 2016;67(1):74-82. [PubMed ID: 26706903]. https://doi.org/10.3109/09637486.2015.1126565.
-
60.
2018.Sugar reduction : report on first year progress.
-
61.
Lewin A, Lindstrom L, Nestle M. Food industry promises to address childhood obesity: preliminary evaluation. J Public Health Policy. 2006;27(4):327-48. [PubMed ID: 17164800]. https://doi.org/10.1057/palgrave.jphp.3200098.
-
62.
Durand MA, Petticrew M, Goulding L, Eastmure E, Knai C, Mays N. An evaluation of the Public Health Responsibility Deal: Informants' experiences and views of the development, implementation and achievements of a pledge-based, public-private partnership to improve population health in England. Health Policy. 2015;119(11):1506-14. [PubMed ID: 26433565]. https://doi.org/10.1016/j.healthpol.2015.08.013.
-
63.
Wang YC, Bleich SN, Gortmaker SL. Increasing caloric contribution from sugar-sweetened beverages and 100% fruit juices among US children and adolescents, 1988-2004. Pediatrics. 2008;121(6):e1604-14. [PubMed ID: 18519465]. https://doi.org/10.1542/peds.2007-2834.
-
64.
Holm AL, Laursen MB, Koch M, Jensen JD, Diderichsen F. The health benefits of selective taxation as an economic instrument in relation to IHD and nutrition-related cancers. Public Health Nutr. 2013;16(12):2124-31. [PubMed ID: 23399106]. https://doi.org/10.1017/S1368980013000153.
-
65.
Goryakin Y, Aldea A, Lerouge A, Guillemette Y. Special focus: The health and economic impact of food reformulation. He heavy burden of obesity: The economics of prevention. OECD Publishing; 2019. p. 209-20. https://doi.org/10.1787/c031ce2c-en.
-
66.
Drewnowski A. Obesity, diets, and social inequalities. Nutr Rev. 2009;67 Suppl 1:S36-9. [PubMed ID: 19453676]. https://doi.org/10.1111/j.1753-4887.2009.00157.x.
-
67.
Roudsari AH, Vedadhir A, Amiri P, Kalantari N, Omidvar N, Eini-Zinab H, et al. Psycho-socio-cultural determinants of food choice: A qualitative study on adults in social and cultural context of Iran. Iran J Psychiatry. 2017;12(4):241.
-
68.
Haghighian-Roudsari A, Milani-Bonab A, Mirzay-Razaz J, Vedadhir A. Food choice as a social problem: A reflection on the socio-cultural determinants of food choice. Salamat IJTIMAI (Community Health). 2018;5(3):291-302.
-
69.
Struben J, Chan D, Dube L. Policy insights from the nutritional food market transformation model: the case of obesity prevention. Ann N Y Acad Sci. 2014;1331:57-75. [PubMed ID: 24593850]. https://doi.org/10.1111/nyas.12381.