Abstract
Background:
Despite effective treatments are available for depressive disorders, less than half of patients utilize them and the treatment gap is large.Objectives:
This study aimed to investigate factors associated with adherence to follow-up in patients diagnosed with a depressive disorder in the collaborative care program in Tehran between May 2017 to October 2017.Methods:
A retrospective cross-sectional study was performed in three community mental health centers (CMHCs) in Tehran.Results:
A total of 435 cases were recruited, and their adherence to follow-up rate was 41.6%. According to multivariate regression, being visited in a particular center, having a high school or higher level of education, having a positive family history with effective treatment, taking selective serotonin reuptake inhibitors (SSRIs), experiencing a lower level of perceived mental health before the first visit, and referral to a psychiatrist could predict adherence to follow-up. Patients who had a chief complaint of typical depressive symptoms and those who were employed were less likely to be adherent to follow-up.Conclusions:
More population-based studies in various settings and cultures are needed to enhance our knowledge regarding interventions necessary to deliver quality care to depressed patients.Keywords
Depressive Disorders Healthcare Access Adherence Follow-up Low- and Middle-income Countries
1. Background
Depressive disorders are the most common mental disorders worldwide (1), with an estimated prevalence of about 4.4%. According to the Iranian Mental Health Survey (IranMHS) in 2011, major depressive disorder is the most common mental disorder in the past 12 months in Iran, with a prevalence of 12.7% (2). It causes various consequences, including disability, suicide, and low social, interpersonal, and occupational functioning (1). Furthermore, depressive disorders are the largest cause of years lived with disability (YLD) in the world (1).
While effective treatments are available to address depressive disorders, less than half of patients receive such services (3-5), and the treatment gap is large (6, 7). Underdiagnosis, cost, unavailability, inadequate treatment, and stigma are some of the reasons for inadequate treatment of depression (8, 9). Additionally, non-adherence is a major problem in the effective treatment of depression (10-12). According to the available estimates, about 40 - 70% of patients in developed countries (13, 14) and 46 - 83% in the Asian countries (12, 13) are non-adherent to antidepressants.
To address adherence and improve the quality of care in patients with depressive disorders, it is necessary to recognize factors associated with adherence in different settings and cultures (15). Limited studies have been published on adherence to follow-up in patients with common mental disorders in Iran (16). According to the IranMHS report, utilization of health services by patients with psychiatric disorders was 34.7% in the past 12 months. According to this survey being women, middle-aged, illiterate, separated, widow, divorced, resident of rural areas, housewife, insured and having middle socioeconomic status were associated with higher health service utilization for those suffering from mental problems. The most common barriers for service utilization were symptoms relief and hoping to get better on your own (17). Another study has investigated adherence to treatment in 2600 patients with depressive and anxiety disorder in two CMHCs located in the capital city of Tehran, Iran. The results of this study indicated that age, being a client of particular clinics, and telephone follow-up were related to adherence to treatment (18). Non-adherence to antidepressants is more prevalent in primary care clinics compared to psychiatric clinics (10). However, there is robust evidence that collaborative care interventions are effective in enhancing adherence to treatment in depression (19, 20).
Iran has well-established networks for primary care that provide services to patients across the lifespan. Since 2010, Iran has established a collaborative care program to improve primary care practitioners’ capacity to provide adult mental health care in some areas. The main objective of the program is to enhance the detection and treatment of common mental disorders in primary care. In the collaborative care model, general practitioners (GPs) receive training using evidence-based guidelines. Then, they will detect and treat mental disorders by themselves among their clients and refer those with severe or hard to treat mental disorders to a psychiatrist. A case manager assists the GPs for following the patients’ treatment. GPs will also document their practice in an electronic health system while a psychiatrist oversees their performance.
2. Objectives
Even in the enhanced care systems such as collaborative care, the rate of non-adherence to treatment is high. The aim of this study is to investigate factors associated with adherence to follow-up in patients diagnosed with a depressive disorder in the collaborative care program in Tehran between May 2017 to October 2017. The community mental health center’s (CMHC) collaborative care were chosen to investigate the non-adherence issue due to the limitations of reliable outpatient data in Iran.
3. Methods
3.1. Design and Field of Study
Following a retrospective cross-sectional design, the current study was done in three CMHCs affiliated to the Tehran University of medical sciences. It is worth noting that the centers were located in Tehran’s southern neighborhoods. One CMHC (center A) was collaborating with public primary care clinics, while the other two were collaborating with private practice GPs (centers B and C had 12 GPs).
3.2. Conceptual Framework
Andersen’s model is a widely used theoretical framework for assessing factors related to health services utilization (21). In this model, factors are categorized into three groups (22): (a) predisposing factors, including social structures such as occupation, beliefs like attitude, and demographic factors such as age and gender; (b) enabling factors that consist of individual factors like income, social and contextual factors such as health system characteristics, and other factors such as genetic and psychological factors; and (c) need factors including perceived needs and evaluated needs. To assess the patients’ barriers to adherence and follow-up visits, a structured telephone interview was developed and conducted based on the Andersen model of health services utilization (21).
3.3. Participants and Sampling
The electronic health information database of the CMHCs contains data on patients’ information from the GP offices, including demographic variables, diagnosis, treatment plan, and follow-up, as well as the practitioners’ records.
Inclusion criteria consisted of being 18 to 65 years old, diagnosis of a current major depressive disorder or dysthymia according to GP’s clinical impression, and giving oral informed consent for the telephone interview. Exclusion criteria were the presence of an intellectual disability, comorbid psychotic disorder, hearing loss, or inability to speak Farsi.
3.4. Data Collection
The patient’s demographic characteristics, diagnosis, and follow-up attendance at GP offices were obtained from the CMHCs’ database. After 3 months (± 1 week) of the diagnosis of depression by the GP and initiation of the treatment, the patients were contacted, and the interview was carried out to measure the related factors. The patients were called 3 times before considering them as unreachable. In the initial part of the telephone interview, the participants were asked whether they knew about their diagnosis or the reason they were taking psychiatric medications. The full interview was conducted only for patients who knew they had depression or mentioned having a mental health problem because the rest of the interview was about patients’ attitudes, stigma, perceived mental health, and dropout follow-up. Six clinical psychologists who worked in the CMHCs carried out all interviews after participating in one training and at least two supervision sessions. One of the researchers (A.M.) supervised the interviews and conducted a complimentary interview if necessary. The telephone interview took between 30 to 60 minutes.
3.5. Definition of the Adherence to Follow-up
The adherence to follow-up was defined as having at least one visit during three months after the first visit by the GP, obtained from the database and confirmed by the patient interview.
3.6. Data Analysis
Statistical analyses were administered by SPSS version 24 (23) using frequency and cross tab run for all variables with chi-square analyses. Binary logistic regression was used to assess the association between the adherence to follow-up and the other variables. A multivariate logistic regression analysis was conducted for variables with a P < 0.2 in binary logistic regression to obtain predictive factors to the adherence to follow-up, and a P < 0.05 indicated statistical significance.
4. Results
4.1. Sample Characteristics
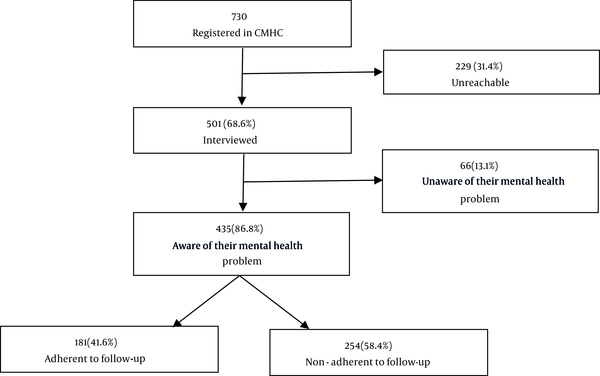
A total of 730 patients with depressive disorders from three CMHCs were approached, of which 501 were interviewed. Figure 1 shows the diagram of participants’ recruitment and interviews. Most patients were from CMHC A (63.6%). About 33.6% of subjects were between 26 and 35 years old, 81.1% were female, slightly less than half (49.4%) had more than high school education, 76.0% were married, and 74% were housewives.
The flow diagram of participants’ recruitment in the study
There were significant differences across the following categories of patients: unreachable patients, patients who were unaware of their mental health problem, and patients who were aware of their mental health problem. Most unreachable patients were male (P = 0.002), and divorced (P = 0.000). Female (85.3%) and married (81.9%) patients and those taking benzodiazepines (27.4%) were more likely to be aware of their mental health problems (P < 0.05). Also, “perceived physical and mental health status in the past month before the first visit” was lower in this group (P < 0.05). On the other hand, patients who were unaware of their mental health problem and attributed their symptoms to a medical illness were more male and single (P < 0.05).
Patients in center A thought that genetics was the least important cause of their illness (P = 0.00). Center A had the lowest employment rate, the lowest education level (P = 0.00), the highest reported financial strain (P = 0.00), the smallest living space (P = 0.02), the shortest duration of illness (P = 0.01), the most percentage of female (P = 0.00) and married patients (P = 0.00), the highest rate of awareness of their depressive disorder (P = 0.00), and the majority of its clients were housewife (P = 0.00). Center B had the highest rate of education level (P = 0.00), the lowest reported financial strain (P = 0.00), the highest rate of duration of illness more than 6 months (P = 0.01), the most percentage of single patients (P = 0.00), and the lowest rate of awareness of their illness (P = 0.00).
Analyses of factors associated with adherence to follow-up were performed on 435 patients who were aware of their mental health problems. Adherence to follow-up rate was 41.6%. Most patients who were adherent to follow-up believed taking medication (80.0%) and going to the health centers (87.6%) were helpful. About 93.8% of them reported that in their first visit they felt medications were needed. Although 61% reported the need for psychological counseling, only 36% of them had been referred to a counselor. Most of the adherent patients were satisfied with the services they received (91.7%). Center B had the highest satisfaction rate (97.1% vs. 88.9% center C and 90.8% center A).
Among patients who were non-adherent to follow-up visits, 19.6 % visited a counselor, 8.5% visited a psychiatrist, 3.2% visited a neurologist on their own, and 7.2% continued taking their medication.
4.2. Adherence to Follow-up
The results of comparative bivariate logistic regression analysis of characteristics of patients who were either adherent or non-adherent to follow-up, are presented in Tables 1 - 3.
Bivariate Logistic Regression Analysis of Predisposing Factors for Overall, Adherent, and Non-adherent Groups to Follow-up a, b
| Predisposing Factors | Total Sample (N = 435) | Adherent (n = 181 [41.6%]) | Non-adherent (n = 254 [58.4%]) | Ρ-Value | OR |
|---|---|---|---|---|---|
| Demographic | |||||
| Age of patient | |||||
| 18 - 25 | 30 (6.9) | 10 (33.3) | 20 (66.7) | Ref | Ref |
| 26 - 35 | 137 (31.5) | 61 (44.5) | 76 (55.5) | 0.264 | 1.605 |
| 36 - 45 | 124 (28.5) | 44 (35.5) | 80 (64.5) | 0.825 | 1.100 |
| 46 - 65 | 129 (29.7) | 59 (45.7) | 70 (54.3) | 0.220 | 1.686 |
| > 65 | 15 (3.4) | 7 (46.7) | 8 (53.3) | 0.387 | 1.750 |
| Gender * | |||||
| Male | 64 (14.7) | 34 (53.1) | 30 (46.9) | Ref | Ref |
| Female | 371 (85.3) | 147 (39.6) | 224 (60.4) | 0.045 | 0.579 |
| Marital status | |||||
| Married | 354 (81.9) | 149 (42.1) | 205 (57.9) | Ref | Ref |
| Single | 32 (7.4) | 13 (40.6) | 19 (59.4) | 0.879 | 0.941 |
| Divorced | 23 (5.3) | 7 (30.4) | 16 (69.6) | 0.279 | 0.602 |
| Widow | 23 (5.3) | 11 (47.8) | 12 (52.2) | 0.585 | 1.261 |
| Social Structure | |||||
| Occupational status | |||||
| Housewife | 326 (76.0) | 126 (38.7) | 200 (61.3) | 0.994 | 0.993 |
| Employed | 64 (14.9) | 32 (50.0) | 32 (50.0) | 0.142 | 1.490 |
| Not working | 39 (9.1) | 21 (53.8) | 18 (46.2) | Ref | Ref |
| Education * | |||||
| High school or more | 218 (50.5) | 102 (46.8) | 116 (53.2) | 0.023 | 1.564 |
| Living arrangement | |||||
| Living alone | 18 (5.2) | 7 (38.9) | 11 (61.1) | Ref | Ref |
| With partner/children | 45 (13.1) | 15 (33.3) | 30 (66.7) | 0.221 | 0.786 |
| With parents | 268 (77.9) | 112 (41.8) | 156 (58.2) | 0.689 | 1.128 |
| Other | 13 (3.8) | 6 (46.2) | 7 (53.8) | 0.885 | 1.347 |
| Number of family members (mean ± SD) | 3.61 ± 1.360 | 3.60 ± 1.316 | 3.61 ± 1.393 | 0.967 | 0.997 |
| Source of recommendation for physician selection | |||||
| No one | 181 (42.5) | 86 (47.5) | 95 (52.5) | 0.263 | 1.281 |
| Health system | 146 (34.3) | 51 (34.9) | 95 (65.1) | 0.345 | 0.759 |
| Other | 99 (23.2) | 41 (41.4) | 58 (58.6) | Ref | Ref |
| Attitude | |||||
| Family psychiatric history | |||||
| No | 245 (57.0) | 88 (35.9) | 157 (64.1) | Ref | Ref |
| Yes | |||||
| No prior treatment | 62 (14.4) | 30 (48.4) | 32 (51.6) | 0.085 | 1.638 |
| Prior treatment | |||||
| Response to treatment * | 93 (21.6) | 52 (55.9) | 41 (44.1) | 0.001 | 2.216 |
| Lack of response | 30 (7.0) | 8 (26.7) | 22 (73.3) | 0.295 | 0.635 |
| Positive past psychiatric history | 159 (37.5) | 72 (45.3) | 87 (54.7) | 0.286 | 1.241 |
| Positive past experience with psychiatric treatment | 71 (63.4) | 37 (52.1) | 34 (47.9) | 0.278 | 1.536 |
| Mental Health Literacy/Awareness | |||||
| Do you know the name of your illness? | |||||
| Doesn’t know/medical illness | 7 (1.6) | 3 (42.9) | 4 (57.1) | Ref | Ref |
| Psychiatric illness | 186 (42.9) | 74 (39.8) | 112 (60.2) | 0.897 | 0.881 |
| Depression | 241 (55.5) | 104 (43.2) | 137 (56.8) | 0.751 | 1.012 |
| Source of health-related information | |||||
| Internet or books | 128 (30.0) | 61 (47.7) | 67 (52.3) | 0.062 | 1.491 |
| Friends | 21 (4.9) | 8 (38.1) | 13 (61.9) | 0.793 | 0.886 |
| Relatives | 38 (8.9) | 10 (26.3) | 28 (73.7) | 0.061 | 0.488 |
| Doctor * | 222 (52.1) | 108 (48.6) | 114 (51.4) | 0.001 | 1.981 |
| TV | 10 (2.4) | 4 (40.0) | 6 (60.0) | 0.951 | 0.961 |
| Other * | 60 (14.1) | 17 (28.3) | 43 (71.7) | 0.036 | 0.526 |
| Cause of the depression | |||||
| Genetic | 24 (5.7) | 13 (54.2) | 11 (45.8) | Ref | Ref |
| Interpersonal conflict | 72 (17.0) | 28 (38.9) | 44 (61.1) | 0.193 | 0.538 |
| Financial problem | 32 (7.6) | 13 (40.6) | 19 (59.4) | 0.316 | 0.579 |
| Other | 295 (69.7) | 120 (40.7) | 175 (59.3) | 0.202 | 0.580 |
| Do you know what type of medication you are taking? (like antidepressant or pain relievers) | 316 (74.0) | 140 (44.3) | 176 (55.7) | 0.093 | 1.469 |
Bivariate Logistic Regression Analysis of Enabling Factors for Overall, Adherent and Non-adherent Groups to Follow-up a, b
| Enabling Factors | Total Sample (N = 435) | Adherent (n = 181 [41.6%]) | Non-adherent (n = 254 [58.4%]) | Ρ-Value | OR |
|---|---|---|---|---|---|
| Social Support/Stigma (All Is About Psychiatric Illness or Treatment) | |||||
| Does anyone know about your illness? * | |||||
| No | 108 (25.5) | 35 (32.4) | 73 (67.6) | 0.022 | 0.584 |
| Do people in your social network support you for taking the medication? * | 277 (68.7) | 136 (49.1) | 141 (50.9) | 0.001 | 2.152 |
| Do people in your social network support you for a follow-up? * | 284 (70.5) | 139 (48.9) | 145 (51.1) | 0.001 | 2.125 |
| What was the others’ opinion about your treatment? (mean ± SD) * | 2.53 ± 1.390 | 2.79 ± 1.313 | 2.34 ± 1.418 | 0.001 | 1.273 |
| How important are their opinions? (mean ± SD) | 2.00 ± 1.413 | 2.02 ± 1.453 | 1.98 ± 1.385 | 0.735 | 1.024 |
| Duration of illness more than 6 months | 146 (35.5) | 68 (46.6) | 78 (53.4) | 0.130 | 1.371 |
| Mental Health Centers | |||||
| Mental health center | |||||
| A | 315 (72.4) | 120 (38.1) | 195 (61.9) | Ref | Ref |
| B * | 61 (14.0) | 34 (55.7) | 27 (44.3) | 0.011 | 2.046 |
| C | 59 (13.6) | 27 (45.8) | 32 (54.2) | 0.270 | 1.371 |
| Financial Situation | |||||
| Financial strain | |||||
| No | 140 (32.4) | 57 (40.7) | 83 (59.3) | Ref | Ref |
| Some | 153 (35.4) | 68 (44.4) | 85 (55.6) | 0.499 | 1.165 |
| Yes | 139 (32.2) | 55 (39.6) | 84 (60.4) | 0.865 | 0.953 |
| Residence status | |||||
| Tenant | 323 (49.3) | 88 (41.5) | 124 (58.5) | 0.948 | 0.986 |
| Own | 215 (50) | 90 (41.9) | 125 (58.1) | Ref | Ref |
| Another person’s home | 3 (0.7) | 1 (33.3) | 2 (66.7) | 0.768 | 0.694 |
| Living space (m2, mean ± SD) | 66.61 ± 24.542 | 66.34 ± 25.57 | 66.81 ± 23.821 | 0.854 | 0.999 |
| Insurance status | |||||
| Insured | 319 (73.7) | 131 (41.1) | 188 (58.9) | 0.847 | 0.958 |
Bivariate Logistic Regression Analysis of Need Factors for Overall, Adherent, and Non-adherent Groups to Follow-up a, b
| Need Factors | Total Sample (N = 435) | Adherent (n = 181 [41.6%]) | Non-adherent (n = 254 [58.4%]) | Ρ-Value | OR |
|---|---|---|---|---|---|
| Chief complain | |||||
| Somatic symptom | 49 (11.3) | 27 (55.1) | 22 (44.9) | Ref | Ref |
| Depression symptom | 181 (41.7) | 75 (41.4) | 106 (58.6) | 0.069 | 0.556 |
| Psychiatric symptom* | 172 (39.6) | 69 (40.1) | 103 (59.9) | 0.048 | 0.526 |
| Other cc* | 32 (7.4) | 9 (28.1) | 23 (71.9) | 0.015 | 0.307 |
| Psychiatric comorbidity | 71 (16.3) | 32 (45.1) | 39 (54.9) | 0.518 | 1.184 |
| Medical comorbidity | |||||
| IHD | 5 (1.1) | 5 (100.0) | 0 | 0.999 | 2331423921 |
| HLP | 4 (0.9) | 2 (50.0) | 2 (50.0) | 0.734 | 1.408 |
| Hypothyroidism | 2 (0.5) | 1 (50.0) | 1 (50.0) | 0.810 | 1.406 |
| HTN | 7 (1.6) | 3 (42.9) | 4 (57.1) | 0.408 | 1.891 |
| Type of medication | |||||
| SSRIs * | 353 (85.1) | 158 (44.8) | 195 (55.2) | 0.003 | 2.539 |
| B- blocker | 39 (9.0) | 17 (43.6) | 22 (56.4) | 0.922 | 1.000 |
| TCAs | 19 (4.5) | 6 (31.6) | 13 (68.4) | 0.371 | 0.637 |
| Antipsychotic | 3 (0.7) | 3 (100) | 0 | 0.999 | 2314569219 |
| BZD | 115 (27.4) | 49 (42.6) | 66 (57.4) | 0.782 | 1.063 |
| Emergency symptoms (suicidality, aggression) | 42 (9.8) | 21 (50.0) | 21 (50.0) | 0.274 | 1.428 |
| Perceived physical health status in the past one month before the first visit (mean ± SD) | 1.57 ± 1.125 | 1.53 ± 1.116 | 1.60 ± 1.134 | 0.573 | 0.952 |
| Perceived mental health status in the past one month before the first visit (mean ± SD) | 1.02 ± 0.955 | 0.94 ± 0.917 | 1.08 ± 0.979 | 0.161 | 0.865 |
| How much you were concerned about depression? (mean ± SD) | 2.83 ± 1.117 | 2.82 ± 1.084 | 2.84 ± 1.142 | 0.888 | 0.988 |
| Referral to psychiatrist (indicator of severity) * | 68 (15.7) | 38 (55.9) | 30 (44.1) | 0.009 | 2.012 |
| Outcome | |||||
| Patient’s reasons for non-adherence/ dissatisfaction to medications | |||||
| Recovery | 67 (16.1) | 0 | 67 (100.0) | 0.997 | 0.000 |
| Cost * | 64 (15.2) | 43 (67.2) | 21 (32.8) | 0.000 | 3.506 |
| Medication’s adverse effect | 99 (23.5) | 35 (35.4) | 64 (64.6) | 0.168 | 0.720 |
| Ineffective treatment | 57 (13.4) | 27 (45.8) | 31 (54.4) | 0.240 | 1.295 |
| Other’s advice | 13 (3.1) | 2 (15.4) | 11 (84.6) | 0.072 | 0.248 |
| Negative attitude towards medications’ efficacy | 18 (4.3) | 0 | 18 (100.0) | 0.998 | 0.000 |
| Lack of confidence in the physician’s competence | 26 (6.2) | 15 (57.7) | 11 (42.3) | 0.085 | 2.024 |
| Stigma | 11 (2.6) | 1 (9.1) | 10 (90.0) | 0.059 | 0.137 |
| Fears about dependency * | 34 (8.1) | 2 (5.6) | 32 (94.1) | 0.001 | 0.078 |
| Long distance to medical center * | 10 (2.4) | 9 (90.0) | 1 (10.0) | 0.014 | 13.337 |
| Disease symptoms | 1 (0.2) | 0 | 1 (100) | 0.844 | 1.000 |
| Other causes | 64 (15.2) | 21 (32.8) | 43 (67.2) | 0.129 | 0.647 |
Non-adherence was significantly higher among females and patients who stated nobody knew about their illness. Patients who reported a history of effective treatment of a mental health problem in their family members, those with high school or more education, patients who reported receiving positive opinions from others about their treatment, and those who mentioned that their source of information for health-related issues is the physician or medical staff, were more likely to be adherent to follow-up. Patients who had the support of their social network for taking the medications and follow-up had a higher rate of adherence. Also, being a client of CMHC B was associated with higher follow-up visits. Furthermore, the adherence rate was significantly higher among those who took SSRIs or were referred to a psychiatrist.
Dissatisfaction with the cost of prescribed medications and distance to health centers were higher among patients who had adherence to follow-up (P = 0.05). Fear of dependency on the medications was significantly higher in non-adherent patients (P = 0.05).
4.3. Predictors of Adherence to Follow-up
A multivariate approach was used to determine factors that can best predict adherence to follow-up. Table 4 shows the results of the multivariate logistic regression model. Patients with high school or higher levels of education were almost 1.7 times more likely to be adherent (P = 0.05). Patients who visited GP offices affiliated to CMHC B were 2.94 times more likely to follow-up their visits (P = 0.01). Furthermore, having a family member with a history of effective treatment (P = 0.04), taking SSRIs (P = 0.00), and referral to a psychiatrist (P = 0.00) predicted more adherence to follow-up.
| Variables | Ρ-Value | Adjusted OR |
|---|---|---|
| Predisposing Factors | ||
| Gender | ||
| Female | 0.442 | 0.629 |
| Occupational status | ||
| Housewife | 0.548 | 0.692 |
| Employed * | 0.046 | 0.313 |
| Not working | Ref | Ref |
| Education | ||
| High school or more | 0.057 | 1.712 |
| Family psychiatric history | ||
| No | Ref | Ref |
| Yes | ||
| No prior treatment | 0.189 | 1.678 |
| Prior treatment | ||
| Response to treatment * | 0.044 | 1.908 |
| Lack of response | 0.189 | 0.449 |
| Cause of the depression | ||
| Genetic | Ref | Ref |
| Interpersonal conflict | 0.733 | 1.247 |
| Financial problem | 0.894 | 1.104 |
| Other | 0.636 | 1.314 |
| Does anyone know about your illness? | ||
| No | 0.909 | 1.041 |
| What was the others’ opinion about your treatment? (mean ± SD) | 0.130 | 1.231 |
| Source of health-related information | ||
| Internet or books | 0.650 | 1.218 |
| Friends | ||
| Relatives | 0.216 | 0.498 |
| Doctor | 0.123 | 1.848 |
| TV | ||
| Other | 0.717 | 0.833 |
| Do you know what type of medication you are taking? | 0.820 | 1.078 |
| Enabling Factors | ||
| Do people in your social network support you for taking the medication? | 0.399 | 1.855 |
| Do people in your social network support you for a follow-up? | 0.945 | 1.055 |
| Duration of illness | ||
| More than 6 months | 0.764 | 1.090 |
| Center name | ||
| A | Ref | Ref |
| B * | 0.015 | 2.940 |
| C | 0.908 | 1.048 |
| Need Factor | ||
| Referral to psychiatrist (indicator of severity) * | 0.010 | 3.246 |
| Type of medication | ||
| SSRIs * | 0.002 | 4.707 |
| B- blocker | ||
| TCAs | ||
| Antipsychotic | ||
| BZD | ||
| Chief complain | ||
| Somatic symptom | Ref | Ref |
| Depression symptom * | 0.042 | 0.386 |
| Psychiatric symptom | 0.131 | 0.490 |
| Other | 0.299 | 0.504 |
| Perceived mental health status in the past one month before the first visit (mean ± SD) | 0.068 | 0.761 |
Patients who initially visited the GP with a chief complaint of typical depressive symptoms (P = 0.04), those who were employed (P = 0.046), and patients who experienced a higher level of perceived mental health status prior to the first visit (P = 0.06) were less likely to be adherent to follow-up.
5. Discussion
This study examined adherence to follow-up in patients diagnosed with a depressive disorder by primary-care physicians in a collaborative care program in Tehran’s southern neighborhoods. The follow-up rate was found as 41.6%; however, there is no national reference point to compare the rates. Moreover, differences in health systems and methodological variations have made comparisons more difficult, particularly between different countries. It has been estimated that 13.7 % of people with depressive disorders in low- and middle-income countries (LMICs) receive treatment (7). Considering the low socioeconomic status of the studied neighborhoods (24, 25), it seems that collaborative care components, including continuous education of GPs, presence of a standard guideline, active telephone follow-up, and the referral system, played a significant role in improving the adherence to follow-up (19, 21, 26).
This study demonstrated that patients who had been visited in center B were 2.9 times more likely to be adherent to follow-up. In addition, center B had the highest satisfaction level of patients, the highest percentage of married patients, the lowest reported financial strain, and patients with high school education or more. Both centers B and C were collaborating with private sector GPs and are located in similar neighborhoods in terms of socioeconomic status. On the other hand, center A had the highest drop-out rate. Center A collaborates with public primary care clinics where the physicians’ turnover rate is high. Compared to other centers, the lowest employment rate, the lowest level of education, and the highest rate of reported financial strain were observed in patients of the collaborative care affiliated to center A. It should be emphasized that the working protocols and clinical guidelines of the three centers were similar. Although part of the difference between the centers can be attributed to social and demographic differences of their populations and is concordant with other studies (21, 27), it is believed that the higher rates of adherence in center B are partly attributable to the performance of their case managers (18, 28). Several studies reported that the quality of the patient-physician relationship, having a fixed physician, and healthcare provider characteristics are influential factors in treatment adherence (11, 29-32).
Positive experience with psychiatric treatment in family members was associated with 1.98 increase in the adherence rate. This factor was considered as an indicator of the patients’ attitude toward mental health services. A positive attitude is associated with higher mental service utilization (21). Kim and Lee and Prokofyeva et al. reported positive psychiatric family history was related to higher service utilization (33, 34).
The association between higher education and adherence to follow-up is consistent with previous studies (27, 35, 36). In contrast to other studies, this study shows that employed patients had a significantly greater risk of dropping out than housewives and unemployed patients (36, 37). However, some studies, such as Gabilondo et al., reported higher service utilization among unemployed depressed patients in Spain (38). In the present study, we assessed patients who referred to the CMHCs that are active during usual office hours. We think one of the reasons for dropouts of employed patients could be the difficulty of making appointments during working hours. Also, stigma in the workplace can be another reason for higher dropout in employed patients.
As expected, referral to a psychiatrist was a predictor of adherence to follow-up. Referral to the psychiatrist at first visit was used as an indicator of illness severity and perceived need. This is parallel with previous studies that indicate more severe depression, and treating by a psychiatrist was associated with higher service use (39-41).
Taking selective serotonin reuptake inhibitors (SSRIs) was significantly associated with higher follow-up rate. In some studies, taking SSRIs, especially new antidepressants such as escitalopram and sertraline, was associated with higher therapeutic adherence (42). This study found no relations between the severity of depression and prescribing SSRIs or between taking SSRIs and reported side effects.
Patients with a chief complaint of typical depressive symptoms had a significantly higher dropout rate. This finding is inconsistent with many published studies that indicated complaining of depressive symptoms, as perceived need, is a predictive factor for higher service use (5, 9, 41, 43). This difference can be attributed to low socioeconomic status of studies areas, likely with more stigma (9) and a negative attitude toward psychiatric disorders. Though, one study showed that higher insight does not necessarily increase adherence in patients with depressive disorders (44).
5.1. Strengths and Limitations
Since limited research on health service utilization in common mental disorders has been conducted in LMICs (37), the result of this study makes a good contribution to the body of knowledge in this field. Moreover, this study examined a wide range of variables based on Andersen’s model. In addition, the study benefitted from multiple sources of information (the registry as well as the interview). Hence, this study could determine whether the patients had discontinued all forms of treatments or only had dropped out of the target primary care clinics.
The main limitation of the study is its generalizability to other populations and different health systems. The study design was planned to investigate adherence to follow-up in a collaborative care program, while the majority of depressed patients use a variety of healthcare systems in Iran. Additionally, the population in the southern neighborhoods of Tehran is not typical of Tehran or other cities. Another limitation is the potential recall bias of some information due to the cross-sectional nature of the study. Short follow-up duration is also a limitation of this study. Finally, this study was not able to fully investigate socio-contextual factors related to health service utilization and adherence to follow-up. To address these problems, future population-based studies are recommended.
5.2. Conclusions
This study examined several predisposing, enabling, and need factors that may influence adherence to follow-up in depressed patients. To design and enhance interventions for delivering quality care to depressed patients, a better understanding of factors related to adherence and service utilization is necessary. As previous studies have shown, collaborative care programs increase the overall follow-up rate in the target populations (19). This study showed that being visited in a particular center, having a family history of positive experience with mental health treatment, being referred to a psychiatrist, and taking SSRIs were predictive factors for adherence to follow-up. The findings of this study indicated a positive attitude towards mental health services, and higher perceived need were related to higher follow-up rate. In contrast to the majority of studies, perceived need was not significantly associated with follow-up rate in our study. Also, this research showed that employment is associated with increased risk of dropout. The present findings might help to improve the quality and performance of the collaborative care programs in the CMHCs. For example, more emphasis on communication skills training for physicians and the staff might result in more engagement of patients.
Acknowledgements
References
-
1.
World Health Organization. Depression and other common mental disorders: global health estimates. Geneva: World Health Organization; 2017. Report No.: WHO/MSD/MER/2017.2.
-
2.
Sharifi V, Amin-Esmaeili M, Hajebi A, Motevalian A, Radgoodarzi R, Hefazi M, et al. Twelve-month prevalence and correlates of psychiatric disorders in Iran: the Iranian Mental Health Survey, 2011. Arch Iran Med. 2015;18(2):76-84. [PubMed ID: 25644794].
-
3.
Fernandez A, Haro JM, Martinez-Alonso M, Demyttenaere K, Brugha TS, Autonell J, et al. Treatment adequacy for anxiety and depressive disorders in six European countries. Br J Psychiatry. 2007;190:172-3. [PubMed ID: 17267936]. https://doi.org/10.1192/bjp.bp.106.023507.
-
4.
Boerema AM, Kleiboer A, Beekman AT, van Zoonen K, Dijkshoorn H, Cuijpers P. Determinants of help-seeking behavior in depression: a cross-sectional study. BMC Psychiatry. 2016;16:78. [PubMed ID: 27009062]. [PubMed Central ID: PMC4806501]. https://doi.org/10.1186/s12888-016-0790-0.
-
5.
Graham A, Hasking P, Brooker J, Clarke D, Meadows G. Mental health service use among those with depression: an exploration using Andersen's Behavioral Model of Health Service Use. J Affect Disord. 2017;208:170-6. [PubMed ID: 27788380]. https://doi.org/10.1016/j.jad.2016.08.074.
-
6.
Simon GE, Fleck M, Lucas R, Bushnell DM, Lido Group. Prevalence and predictors of depression treatment in an international primary care study. Am J Psychiatry. 2004;161(9):1626-34. [PubMed ID: 15337653]. https://doi.org/10.1176/appi.ajp.161.9.1626.
-
7.
Evans-Lacko S, Aguilar-Gaxiola S, Al-Hamzawi A, Alonso J, Benjet C, Bruffaerts R, et al. Socio-economic variations in the mental health treatment gap for people with anxiety, mood, and substance use disorders: results from the WHO World Mental Health (WMH) surveys. Psychol Med. 2018;48(9):1560-71. [PubMed ID: 29173244]. [PubMed Central ID: PMC6878971]. https://doi.org/10.1017/S0033291717003336.
-
8.
Phelan JC, Yang LH, Cruz-Rojas R. Effects of attributing serious mental illnesses to genetic causes on orientations to treatment. Psychiatr Serv. 2006;57(3):382-7. [PubMed ID: 16524997]. https://doi.org/10.1176/appi.ps.57.3.382.
-
9.
Andrade LH, Alonso J, Mneimneh Z, Wells JE, Al-Hamzawi A, Borges G, et al. Barriers to mental health treatment: Results from the WHO World Mental Health surveys. Psychol Med. 2014;44(6):1303-17. [PubMed ID: 23931656]. [PubMed Central ID: PMC4100460]. https://doi.org/10.1017/S0033291713001943.
-
10.
Sirey JA, Banerjee S, Marino P, Bruce ML, Halkett A, Turnwald M, et al. Adherence to depression treatment in primary care: A randomized clinical trial. JAMA Psychiatry. 2017;74(11):1129-35. [PubMed ID: 28973066]. [PubMed Central ID: PMC5710215]. https://doi.org/10.1001/jamapsychiatry.2017.3047.
-
11.
Pampallona S, Bollini P, Tibaldi G, Kupelnick B, Munizza C. Patient adherence in the treatment of depression. Br J Psychiatry. 2002;180:104-9. [PubMed ID: 11823317]. https://doi.org/10.1192/bjp.180.2.104.
-
12.
Prukkanone B, Vos T, Burgess P, Chaiyakunapruk N, Bertram M. Adherence to antidepressant therapy for major depressive patients in a psychiatric hospital in Thailand. BMC Psychiatry. 2010;10:64. [PubMed ID: 20727215]. [PubMed Central ID: PMC2936351]. https://doi.org/10.1186/1471-244X-10-64.
-
13.
Novick D, Montgomery W, Moneta V, Peng X, Brugnoli R, Haro JM. Antidepressant medication treatment patterns in Asian patients with major depressive disorder. Patient Prefer Adher. 2015;9:421-8. [PubMed ID: 25792815]. [PubMed Central ID: PMC4362981]. https://doi.org/10.2147/PPA.S68432.
-
14.
Brown C, Battista DR, Bruehlman R, Sereika SS, Thase ME, Dunbar-Jacob J. Beliefs about antidepressant medications in primary care patients: relationship to self-reported adherence. Med Care. 2005;43(12):1203-7. [PubMed ID: 16299431]. https://doi.org/10.1097/01.mlr.0000185733.30697.f6.
-
15.
Velligan DI, Sajatovic M, Hatch A, Kramata P, Docherty JP. Why do psychiatric patients stop antipsychotic medication? A systematic review of reasons for nonadherence to medication in patients with serious mental illness. Patient Prefer Adherence. 2017;11:449-68. [PubMed ID: 28424542]. [PubMed Central ID: PMC5344423]. https://doi.org/10.2147/PPA.S124658.
-
16.
Khazaie H, Rezaie L, de Jong DM. Dropping out of outpatient psychiatric treatment: a preliminary report of a 2-year follow-up of 1500 psychiatric outpatients in Kermanshah, Iran. Gen Hosp Psychiatry. 2013;35(3):314-9. [PubMed ID: 23265950]. https://doi.org/10.1016/j.genhosppsych.2012.10.008.
-
17.
Ministry of Health and Medical Education. Iran national mental health survey (IranNMHS). Tehran, Iran: Bureau of Mental and Social Health and Substance Abuse; 2011.
-
18.
Abolhassani F, Sharifi V, Moazami GL, Mousavinia S, Jafarineia M, Amin E. Factors associated with drop-out from treatment in patients with anxiety and depressive disorders. Hakim Health Sys Res. 2014;17(3).
-
19.
Hochhausen L, Le HN, Perry DF. Community-based mental health service utilization among low-income Latina immigrants. Community Ment Health J. 2011;47(1):14-23. [PubMed ID: 19821029]. https://doi.org/10.1007/s10597-009-9253-0.
-
20.
Vergouwen AC, Bakker A, Katon WJ, Verheij TJ, Koerselman F. Improving adherence to antidepressants: A systematic review of interventions. J Clin Psychiatry. 2003;64(12):1415-20. [PubMed ID: 14728101]. https://doi.org/10.4088/jcp.v64n1203.
-
21.
von Lengerke T, Gohl D, Babitsch B. Re-revisiting the behavioral model of health care utilization by andersen: A review on theoretical advances and perspectives. Health Care Utilization in Germany. 2014. p. 11-28. https://doi.org/10.1007/978-1-4614-9191-0_2.
-
22.
Andersen RM. Revisiting the behavioral model and access to medical care: does it matter? J Health Soc Behav. 1995;36(1):1-10. [PubMed ID: 7738325].
-
23.
IBM Corp. IBM SPSS statistics for windows, version 24.0. Armonk, NY: IBM Corp; Released 2016. Available from: https://community.ibm.com/community/user/datascience/blogs/douglas-stauber/2016/03/15/whats-new-in-ibm-spss-statistics-24.
-
24.
Nabalamba A, Millar WJ. Going to the doctor. Health Rep. 2007;18(1):23-35. [PubMed ID: 17441441].
-
25.
Ani C, Bazargan M, Bazargan-Hejazi S, Andersen RM, Hindman DW, Baker RS. Correlates of self-diagnosis of chronic medical and mental health conditions in under-served African American and Latino populations. Ethn Dis. 2008;18(2 Suppl 2):S2-105-11. [PubMed ID: 18646330].
-
26.
Gilbody S, Bower P, Fletcher J, Richards D, Sutton AJ. Collaborative care for depression: A cumulative meta-analysis and review of longer-term outcomes. Arch Intern Med. 2006;166(21):2314-21. [PubMed ID: 17130383]. https://doi.org/10.1001/archinte.166.21.2314.
-
27.
Rivero-Santana A, Perestelo-Perez L, Perez-Ramos J, Serrano-Aguilar P, De Las Cuevas C. Sociodemographic and clinical predictors of compliance with antidepressants for depressive disorders: Systematic review of observational studies. PATIENT PREFER ADHER. 2013;7:151-69. [PubMed ID: 23487319]. [PubMed Central ID: PMC3592507]. https://doi.org/10.2147/PPA.S39382.
-
28.
Heise BA, van Servellen G. The nurse's role in primary care antidepressant medication adherence. J Psychosoc Nurs Ment Health Serv. 2014;52(4):48-57. [PubMed ID: 24305910]. https://doi.org/10.3928/02793695-20131126-08.
-
29.
Reneses B, Munoz E, Lopez-Ibor JJ. Factors predicting drop-out in community mental health centres. World Psychiatry. 2009;8(3):173-7. [PubMed ID: 19812755]. [PubMed Central ID: PMC2755282]. https://doi.org/10.1002/j.2051-5545.2009.tb00246.x.
-
30.
Heidari E, Eslami S, Abolhassani F, Sharifi V, Taherzadeh Z, Daneshvar T. Association between physicians' adherence to a pharmacotherapy guideline and continuity of care for patients with depression and/or anxiety disorder. Arch Iran Med. 2017;20(5):308-13. [PubMed ID: 28510467].
-
31.
Bultman DC, Svarstad BL. Effects of physician communication style on client medication beliefs and adherence with antidepressant treatment. Patient Educ Couns. 2000;40(2):173-85. https://doi.org/10.1016/s0738-3991(99)00083-x.
-
32.
Boyas JF, Negi NJ, Valera P. Factors associated to health care service use among latino day laborers. Am J Mens Health. 2017;11(4):1028-38. [PubMed ID: 28625117]. [PubMed Central ID: PMC5675338]. https://doi.org/10.1177/1557988317694297.
-
33.
Kim HK, Lee M. Factors associated with health services utilization between the years 2010 and 2012 in Korea: using Andersen's Behavioral model. Osong Public Health Res Perspect. 2016;7(1):18-25. [PubMed ID: 26981338]. [PubMed Central ID: PMC4776261]. https://doi.org/10.1016/j.phrp.2015.11.007.
-
34.
Prokofyeva E, Martins SS, Younes N, Surkan PJ, Melchior M. The role of family history in mental health service utilization for major depression. J Affect Disord. 2013;151(2):461-6. [PubMed ID: 23856284]. https://doi.org/10.1016/j.jad.2013.06.025.
-
35.
Volkert J, Andreas S, Harter M, Dehoust MC, Sehner S, Suling A, et al. Predisposing, enabling, and need factors of service utilization in the elderly with mental health problems. Int Psychogeriatr. 2018;30(7):1027-37. [PubMed ID: 29198254]. https://doi.org/10.1017/S1041610217002526.
-
36.
Lee LH, Lee S. Association between employment and mental health service use among justice-involved individuals. Community Ment Health J. 2018;54(5):634-40. [PubMed ID: 29129007]. https://doi.org/10.1007/s10597-017-0186-8.
-
37.
Roberts T, Miguel Esponda G, Krupchanka D, Shidhaye R, Patel V, Rathod S. Factors associated with health service utilisation for common mental disorders: a systematic review. BMC Psychiatry. 2018;18(1):262. [PubMed ID: 30134869]. [PubMed Central ID: PMC6104009]. https://doi.org/10.1186/s12888-018-1837-1.
-
38.
Gabilondo A, Rojas-Farreras S, Rodriguez A, Fernandez A, Pinto-Meza A, Vilagut G, et al. Use of primary and specialized mental health care for a major depressive episode in Spain by ESEMeD respondents. Psychiatr Serv. 2011;62(2):152-61. [PubMed ID: 21285093]. https://doi.org/10.1176/ps.62.2.pss6202_0152.
-
39.
Boenisch S, Kocalevent RD, Matschinger H, Mergl R, Wimmer-Brunauer C, Tauscher M, et al. Who receives depression-specific treatment? A secondary data-based analysis of outpatient care received by over 780,000 statutory health-insured individuals diagnosed with depression. Soc Psychiatry Psychiatr Epidemiol. 2012;47(3):475-86. [PubMed ID: 21350809]. https://doi.org/10.1007/s00127-011-0355-y.
-
40.
Tylee A. Depression in Europe: Experience from the DEPRES II survey. Eur Neuropsychopharmacol. 2000;10:S445-8. https://doi.org/10.1016/s0924-977x(00)00112-7.
-
41.
Sareen J, Cox BJ, Afifi TO, Yu BN, Stein MB. Mental health service use in a nationally representative Canadian survey. Can J Psychiatry. 2005;50(12):753-61. [PubMed ID: 16408523]. https://doi.org/10.1177/070674370505001204.
-
42.
Akincigil A, Bowblis JR, Levin C, Walkup JT, Jan S, Crystal S. Adherence to antidepressant treatment among privately insured patients diagnosed with depression. Med Care. 2007;45(4):363-9. [PubMed ID: 17496721]. [PubMed Central ID: PMC2882940]. https://doi.org/10.1097/01.mlr.0000254574.23418.f6.
-
43.
Fleury MJ, Ngui AN, Bamvita JM, Grenier G, Caron J. Predictors of healthcare service utilization for mental health reasons. Int J Environ Res Public Health. 2014;11(10):10559-86. [PubMed ID: 25321874]. [PubMed Central ID: PMC4210995]. https://doi.org/10.3390/ijerph111010559.
-
44.
Lee MS, Lee HY, Kang SG, Yang J, Ahn H, Rhee M, et al. Variables influencing antidepressant medication adherence for treating outpatients with depressive disorders. J Affect Disord. 2010;123(1-3):216-21. [PubMed ID: 19914719]. https://doi.org/10.1016/j.jad.2009.10.002.