Abstract
Background:
The migraine headache is one of the common chronic pains. Recent psychopathological approaches emphasized more on acceptance than the control of pain. Psychological inflexibility in pain scale (PIPS) is a tool to assess pain acceptance.Objectives:
The current study aimed at evaluating the psychometric properties of PIPS.Methods:
The study sample comprised of 250 individuals with migraine headache. They were selected from patients admitted to neurological ward of Shahid Beheshti Hospital and private neurology clinics in Kashan, Iran in summer 2015. After preparation of the PIPS (translation and back-translation), participants completed the PIPS and chronic pain acceptance questionnaire (CPAQ). The factor structure and correlation of PIPS with CPAQ were examined.Results:
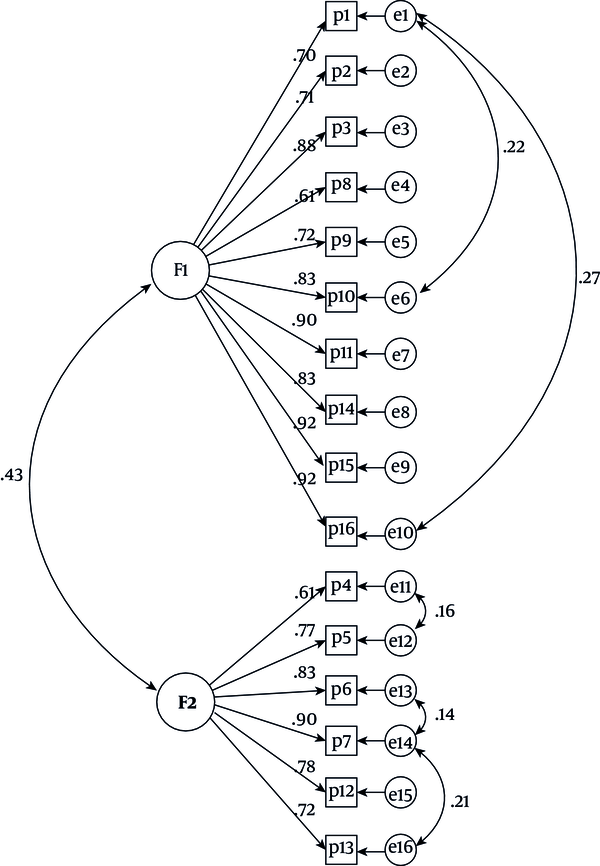
The results of exploratory factor analysis (EFA) showed two factors of pain avoidance (10 items) and cognitive fusion factor (six items) for this scale. The confirmatory factor analysis (CFA) confirmed the obtained model in comparison with the original model (group factor analysis (GFA), CFA, and the Tucker-Lewis index (TLI) ≥ 0.90; the root mean square error of approximation (RMSEA) 90% confidence interval (CI) = 0.03 - 0.06). Also, the convergent validity of this scale was confirmed with CPAQ (r =.66, P < 0.001). The reliability of the scale by internal consistency and test-retest method was good.Conclusions:
The Persian version of PIPS has appropriate psychometric features in Iranian society and it can be used to measure this characteristic.Keywords
Psychological Inflexibility in Pain Scale Validity Reliability Migraine Headache
1. Background
Chronic pain is a pain manifested continuously for at least three months during the past six months (1). The prevalence of chronic pain in general adult population in Iran is reported 25.5% (2). The chronic pain often interferes with the person’s capability of doing various activities of life. Based on International Association for the Study of Pain (3), 33% - 50% of individuals with chronic pain have disability to perform their daily activities (4). One of the common chronic pains is migraine headache. It was reported that 12.8% of patients referred to the neurology clinic had migraine (5). The prevalence of migraine headache was 6% in males and 20% in females in the Western countries and 8.4% in males and 12.5% in females in Iran (6). Migraine headaches have undesirable effects on all the individuals’ life aspects such as social performance and family life (7). According to the World Health Organization (WHO) the headache is among the 10 debilitating states for males and females (8) and is considered as a common cause for early retirement, losing working hours, and burdensome socioeconomic consequences in many countries (9). The studies on such patients generally show high rate of disability, along with psychological disorders such as chronic fatigue, depression, and anxiety (10). Feelings of helplessness with psychological problems are associated with many chronic problems (11).
On the other hand, when people are not willing to be exposed to their own negative psychological experiences such as pain, fear, and anxiety, they have an ineffective emotional life. Usually, two psychological processes might manifest in such conditions: experiential avoidance (EA) and cognitive fusion (CF). The EA is a process in which the person attempts to change the quality of experiences or avoid his own personal experiences. CF occurs when negative thoughts and emotions are excessive or inappropriate and affect a person’s valuable activity (12). When these two processes dominate the person’s behavior and experiences, psychological inflexibility occurs (13). From the perspective of acceptance and commitment therapy (ACT), the psychological inflexibility is a source for the pain in many people. In a sample of patients with fibromyalgia, decreasing psychological flexibility had correlation with pain disability, quality of life, self-efficiency, depression, and anxiety (13). In contrast, psychological flexibility is the ability to attend in the present moment and doing a value based activity. Furthermore, by allowing the values to guide individuals, they can create a more sense of meaning and purposeful in themselves, and experience a sense of vitality (14). It is reported that ACT with emphasis on psychological flexibility can reduce the headache intensity and headache disability in chronic daily headaches (15).
According to the importance of psychological flexibility in pain, its evaluation is important. One of the scales that measure psychological flexibility in pain disorders is the psychological inflexibility in pain scale (PIPS). The acquired information of this scale can guide the physicians; therefore, they can devise their therapeutic interventions in a way that is consistent with patient’s problems (13). This tool is applied in many countries. For example, Wicksell et al. (16), studied the factor structure of this scale in a Swedish patient with chronic pain. The results of the study confirmed the bifactor structure of this scale (avoidance: eight items; thought fusion: four items) that removed the four items of original model (items 3, 6, 10, and 16). They reported a significant correlation between scale total with anxiety (r = 0.50) and depression (r = 0.60, P < 0.001). Rodero et al. (13) studied the convergent validity of Spanish version of PIPS with pain acceptance scale in patients with fibromyalgia. The internal consistency was reported 0.97 and Cronbach’s alpha was 0.90. This version was related to anxiety (r = 0.54), pain catastrophizing (r = 0.62), and pain acceptance (r = -0.72). Also, another study showed the correlation between PIPS and mindfulness in patients with chronic pain (17). The confirmatory factor analysis (CFA) of German version of this scale in 182 patients with chronic back pain confirmed the main bifactor structure. Internal consistency of avoidance scale was 0.91 and cognitive fusion of the scale was 0.26. Based on these results, the avoidance subscale was introduced as the appropriate scale, but it was not the case with the cognitive fusion subscale (18). Also, in the study by Trompetter et al. (17), showed the problems with the cognitive fusion subscale. However, despite the frequent use of this scale in other countries, no study examined the psychometric features of this scale in Iran.
2. Objectives
The current descriptive study aimed at evaluating the psychometric features of PIPS in patients with migraine.
3. Materials and Methods
After getting permission from the scale devisor, the scale was translated from English to Persian by three psychology professors. Then, the scale was examined by the authors. They were familiar with the psychological construct assessed by this scale.
Then, two bilingual linguistic experts, who had no specific knowledge regarding the questionnaire, carried out back-translations (forward and backward method). Any differences between the translations were resolved by consensus. In the next step, the translated text was compared with the original text of scale and confounding factors were removed. Then, after selecting the samples and gaining their permission, the scales were completed by them. In order to assess the test-retest reliability, 50 individuals of the sample were evaluated again after four weeks. The data were analyzed with SPSS version 22. For the CFA, IBM-22 Amos software was used.
The current study was approved by the Research Deputy of Islamic Azad University, Najafabad Branch, Iran (No.152020701932050).
3.1. Participants
Statistical population included all patients admitted to neurology ward of Kashan Shahid Beheshti Hospital and private neurology clinics in Kashan, Iran in summer 2015. In order to perform factor analysis on the final tool, for each item in scale, 5 - 10 samples were required (19). Therefore, considering the number of items in this scale (16 items) the sample size was 160 subjects, which by calculating dropouts, 250 individuals were selected as samples by simple sampling method. Inclusion criteria were: age 18 - 50 years, the patients’ consent, migraine diagnosis by a neurologist, and minimum middle school education. And exclusion criteria were: severe psychological disorder (psychosis or acute bipolar disorder), addiction, and brain injury. All patients that met the criteria and completed informed consent form responded to PIPS and chronic pain acceptance questionnaire (CPAQ).
3.2. Interview
Diagnostic interview for accurate diagnosis of migraine was conducted by a neurologist using a structured interview based on the International Headache Society (HIS) criteria (20).
3.2.1. Psychological Inflexibility in Pain Scale
This scale that is developed by Wicksell et al. (21), is one of the most applicable scales in this context. This scale is comprised of 38 items and was formulated to measure avoidance, cognitive fusion, values, and acceptance. In the factor analysis by the Wicksell et al. (21), its bifactor structure, which includes avoidance (10 items) and acceptance (six items), was confirmed. The pain avoidance subscale measures certain behaviors related to pain avoidance and distress, and cognitive fusion subscale assesses the frequency of patient’s experienced thoughts that can lead to avoidance behaviors if turned into action. This scale is scored based on a seven-point Likert scale, from never agree (1) to always agree (7), and higher scores indicate more inflexibility. The PIPS psychometric properties were examined in various countries such as Spain (13), Sweden (16), and Germany (18). These studies confirmed two factors (avoidance and fusion) for this scale. The internal consistency of the PIPS total was reported 0.87. The Cronbach’s α for avoidance scale was 0.89 and for fusion was 0.66 (13).
3.2.2. Chronic Pain Acceptance Questionnaire
The Persian version of this tool, similar to its original version, assesses chronic pain acceptance in two forms: activity engagement (pursuit of life activities regardless of pain) (11 phrases) and pain willingness (recognition that avoidance and control are often unworkable methods of adapting to chronic pain) (nine phrases). The responder should complete each item based on a seven-option Likert scale. The method of calculating total score of acceptance is that initially, the scale phrases of activity engagement were scored from 0 to 6 and pain satisfaction scale phrases were scored conversely, and then, the resulting scores of two subscales are added together. In this scale, the total scores range from 0 to 120 and higher scores indicate more pain acceptance. Cronbach alpha coefficient of the Persian version of the scale was reported 0.71, which confirmed the convergent validity of the scale with pain self-efficiency scale and its divergent validity with physical disability, depression, anxiety, pain intensity, and catastrophizing (4).
4. Results
In the current study, 173 subjects (69.2%) were female and the rest were male and 125 were married. The age of participants ranged 18 to 50 years (mean = 33.2, standard deviation (SD) = 6.65). According to Table 1, most participants were 25 to 34 years old (52%).
Distribution of the Study Participants Based on Age and Gender
| State | Valuesa |
|---|---|
| Age | |
| Mean ± SD | 33.2 ± 6.65 |
| 18 - 26 | 25 (10) |
| 26 - 34 | 130 (52) |
| 34 - 42 | 64 (25.6) |
| 42 - 50 | 31 (12) |
| Gender | |
| Female | 173 (69.2) |
| Male | 77 (30.8) |
4.1. Construct Validity
In order to examine the construct validity, exploratory factor analysis (EFA), using Varimax rotation method, was applied. The acquired statistical indexes were suitable for factor analysis (Kaiser-Meyer-Olkin (KMO) = 0.86; Bartlett χ2 = 2269.17; P ≤ 0.001). The results showed the existence of two factors, and these two subscales together specified 74% of the variance.
Results of the Exploratory Factor Analysis of the PIPS
| Items | Factors | |
|---|---|---|
| 1 | 2 | |
| 1. I would do almost anything to get rid of my pain. | 0.84 | |
| 2. I don’t do things that are important to me to avoid feeling pain. | 0.50 | |
| 3. When I am in pain, I stay away from other people. | 0.89 | |
| 4. It is important that I learn how to control my pain. | 0.87 | |
| 5. It is important to understand what causes my pain. | 0.81 | |
| 6. I feel angry about my pain. | 0.92 | |
| 7. I say things like ”I don’t have any energy”, ”I am not well enough”, ”I don’t have time”, ”I don’t dare”, ”I have too much pain”, ”I feel too bad”, or ”I don’t feel like it”. | 0.83 | |
| 8. I avoid doing things when there is a risk it will hurt or make things worse. | 0.86 | |
| 9. I avoid scheduling activities because of my pain. | 0.89 | |
| 10. I put a lot of effort into fighting my pain. | 0.94 | |
| 11. It’s not me that controls my life, it’s my pain. | 0.90 | |
| 12. I need to understand what is wrong in order to move on. | 0.67 | |
| 13. Because of my pain, I no longer plan for the future. | 0.86 | |
| 14. I postpone things on account of my pain. | 0.95 | |
| 15. I cancel planned activities when I am in pain. | 0.76 | |
| 16. I interrupt activities if it starts to hurt or becomes worse. | 0.78 | |
| Eigenvalue | 8.78 | 3.19 |
| %Variance | 54.90 | 19.96 |
According to Table 2, the first factor included questions 1, 2, 3, 8, 9, 10, 11, 14, and 15 with 8.78 eigenvalue, which given the item content, was named pain avoidance scale. The questions 4, 5, 6, 7, 12, and 13 were loaded in the second factor with 3.19 eigenvalue of this factor, considering the content of its items, was called cognitive fusion scale. The results of the current study were different from those of the previous studies: (1) Questions 1 and 3 were loaded in the pain avoidance factor in the current study, while it was loaded in the cognitive fusion factor in previous studies; (2) The questions 7 and 13 were loaded in the cognitive fusion factor in the current study, while in previous studies; it was loaded in the pain avoidance factor. The CFA showed that the obtained model had better fitness than original model (group factor index (GFA), the adjusted goodness of fit index (AGFI), CFA, and the Tucker-Lewis index (TLI) ≥ 0.90; the root mean square error of approximation (RMSEA) ≤ 0.05). The goodness of fit indexes for the original and the current model is reported in Table 3.
CFA Results of Original and Obtained Models of PIPS
| Fitness Index Models | χ2/df | GFI | AGFI | TLI | CFI | RMSEA (90% CI) |
|---|---|---|---|---|---|---|
| Original model | 2.76 | 0.92 | 0.89 | 0.86 | 0.89 | 0.09 (0.08 - 0.12) |
| Current model | 1.75 | 0.95 | 0.90 | 0.92 | 0.95 | 0.05 (0.03 - 0.06) |
Results of structural equation modeling analysis of two-factor model PIPS
4.2. Convergent Reliability
In order to measure the convergent reliability of the PIPS, the correlation of this scale and extracted subscales were studied with the CPAQ. Accordingly, PIPS total (r = 0.66, P < 0.001), avoidance scale (r = 0.86, P < 0.001), and cognitive fusion scale (r = 0.66, P < 0.001) demonstrated significant correlation with CPAQ (P < 0.001).
| Reliability Coefficient Scale | Cronbach Alpha | Retest |
|---|---|---|
| Total scale | 0.94 | 0.65* |
| Subscale 1 | 0.95 | 0.55* |
| Subscale 2 | 0.86 | 0.60* |
4.3. Reliability
In order to study the reliability of PIPS, internal consistency (Cronbach’s alpha) and test-retest reliability with four-week interval were calculated. The results showed that internal consistency by Cronbach’s alpha was 0.94 for scale total, 0.95 for pain avoidance, and 0.85 for cognitive fusion scales. The test-retest reliability for total scale was 0.65, and for first and second factors was 0.55 and 0.60, respectively (P < 0.001, Table 3).
5. Discussion
The study aimed at examining factor structure and psychometric features of PIPS in patients with migraine headache. The results of EFA indicated two factors for this scale that included pain avoidance with 10 questions and cognitive fusion factor with six questions. This finding was consistent with those of previous studies. Although, the number of items of each factor (pain avoidance = 10 items and thought fusion = six items) was consistent with those of previous studies, in the current study, items 7 and 13 from pain avoidance factor were placed in cognitive fusion factor, and in contrast, items 1 and 10, which were placed in cognitive fusion factor in previous studies, were loaded in pain avoidance factor. One possible reason for this change can be cultural differences. It seems that the 1st (I would do almost anything to get rid of my pain) and the 2nd (I put a lot of effort into fighting my pain.) items bring the pain avoidance behaviors to Iranian migraine patients’ minds rather than the frequency of thoughts associated with an event. Therefore, these items were placed in pain avoidance scale.
Also, it seems that items 7 (I say things like ”I don’t have any energy”, ”I am not well enough”, ”I don’t have time”, ”I don’t dare”, ”I have too much pain”, ”I feel too bad” or ”I don’t feel like it”) and 13 (“Because of my pain, I no longer plan for the future”) were inferred as a person’s extreme thoughts and emotions, which affect his performance. Therefore, these items were loaded in cognitive fusion subscale rather than being placed in pain avoidance factor (unlike previous studies). The other reason for this difference might be the difference in the study samples. For example, in the study by Rodero et al. (13), the sample study were Spanish patients with fibromyalgia, and in the study by Barke et al. (18), the sample included German patients with descent chronic low back pain.
The other sections of the study examined the convergent validity and reliability of this scale. The results showed that pain avoidance, cognitive fusion scale, and also the scale total score had high correlation with pain acceptance scale. This finding was consistent with those of previous studies (13, 18), and confirmed the convergent validity of this scale. Furthermore, these results showed that the internal consistency of scale total and pain avoidance subscales and cognitive fusion scale were high (> 0.85), and the scale had a good test-retest reliability.
5.1. Conclusions
In short, it can be said that the Persian version of PIPS had appropriate psychometric features in Iranian patients with migraine, and it can be used to measure this characteristic.
Acknowledgements
References
-
1.
Noble M, Tregear SJ, Treadwell JR, Schoelles K. Long-term opioid therapy for chronic noncancer pain: a systematic review and meta-analysis of efficacy and safety. J Pain Symptom Manage. 2008;35(2):214-28. [PubMed ID: 18178367]. https://doi.org/10.1016/j.jpainsymman.2007.03.015.
-
2.
Mohammadzadeh F, Faghihzadeh S, Baghestani AR, Asadi Lari M, Vaez Mahdavi MR, Arab Kheradmand J, et al. [Epidemiology of chronic pain in tehran small area estimation of its prevalence in tehran neighborhoods by bayesian approach (Urban HEART-2 study)]. Iran J Epidemiol. 2013;9(1):19-31. Persian.
-
3.
International Association for the Study for Pain. Unrelieved pain is a major global healthcare problem. 2003. Available from: http://www.iasp-pain.org/AM/Template.cfm? Section=Press_Release& Template=/CM/ContentDisplay.cfm&ContentID=2908/.
-
4.
Mesgarian F, Asghari Moghadam MA, Shairii MR, Broumand A, Maroufi N, Ebrahimi Takamjani I, et al. The relation between acceptance of pain and reduced pain intensity and disability among chronic pain patients. J Res Behav Sci. 2013;10(3):194-203.
-
5.
Ahmadpanah M, Kakekhani H, Ghaderzadeh P. [Investigation of prevalence and clinical characteristics of migraine patients referred to the neurology department of Sina Hospital, 2010]. Pajouhan Sci J. 2014;12(4):1-6. Persian.
-
6.
Ayatollahi SM, Khosravi A. Prevalence of migraine and tension-type headache in primary-school children in Shiraz. East Mediterr Health J. 2006;12(6):809-17. [PubMed ID: 17333827].
-
7.
Solomon GD, Dahlof GH. Impact of headache on the individual sufferer. In: Olesen J, Tfelt-Hansen P, Welch KMA, editors. The Headaches. Philadelphia: Lippicott Wilkins; 2000.
-
8.
Stovner L, Hagen K, Jensen R, Katsarava Z, Lipton R, Scher A, et al. The global burden of headache: a documentation of headache prevalence and disability worldwide. Cephalalgia. 2007;27(3):193-210. [PubMed ID: 17381554]. https://doi.org/10.1111/j.1468-2982.2007.01288.x.
-
9.
Etri M, Adib-Hajbaghery M. Effects of acupressure on pain and vital signs of patients after small abdominal surgeries: A clinical trial. Nurs Midwifery Stud. 2012;1(2):67-71. https://doi.org/10.5812/nms.9079.
-
10.
Rhudy JL, Williams AE, McCabe KM, Nguyen MA, Rambo P. Affective modulation of nociception at spinal and supraspinal levels. Psychophysiology. 2005;42(5):579-87. [PubMed ID: 16176380]. https://doi.org/10.1111/j.1469-8986.2005.00313.x.
-
11.
Zargar F, Foruzandeh E, Omidi A, Mohammadi A. Psychological health and marital adjustment in Iranian employed veterans and veterans receiving disability pension. Iran Red Crescent Med J. 2014;16(7). e10219. [PubMed ID: 25237560]. [PubMed Central ID: PMC4166079]. https://doi.org/10.5812/ircmj.10219.
-
12.
Hayes SC, Luoma JB, Bond FW, Masuda A, Lillis J. Acceptance and commitment therapy: model, processes and outcomes. Behav Res Ther. 2006;44(1):1-25. [PubMed ID: 16300724]. https://doi.org/10.1016/j.brat.2005.06.006.
-
13.
Rodero B, Pereira JP, Perez-Yus MC, Casanueva B, Serrano-Blanco A, Rodrigues da Cunha Ribeiro MJ, et al. Validation of a Spanish version of the psychological inflexibility in pain scale (PIPS) and an evaluation of its relation with acceptance of pain and mindfulness in sample of persons with fibromyalgia. Health Qual Life Outcomes. 2013;11:62. [PubMed ID: 23594367]. [PubMed Central ID: PMC3635918]. https://doi.org/10.1186/1477-7525-11-62.
-
14.
Harris R, Hayes S. ACT made simple: An easy-to-read primer on acceptance and commitment therapy (The New Harbinger Made Simple Series). New Harbinger Publications; 2009.
-
15.
Khazraee H, Omidi A, Daneshvar Kakhki R, Zanjani Z, Sehat M. Effectiveness of acceptance and commitment therapy in cognitive emotion regulation strategies, headache-related disability, and headache intensity in patients with chronic daily headache. Iran Red Crescent Med J. 2018;In Press(In Press). https://doi.org/10.5812/ircmj.57151.
-
16.
Wicksell RK, Lekander M, Sorjonen K, Olsson GL. The Psychological Inflexibility in Pain Scale (PIPS)--statistical properties and model fit of an instrument to assess change processes in pain related disability. Eur J Pain. 2010;14(7):771 e1-14. [PubMed ID: 20106685]. https://doi.org/10.1016/j.ejpain.2009.11.015.
-
17.
Trompetter HR, Bohlmeijer ET, van Baalen B, Kleen M, Köke A, Reneman M, et al. The psychological inflexibility in pain scale (PIPS): Exploration of psychometric properties in a heterogeneous chronic pain sample. Eur J Psychol Assess. 2014;30(4):289-95. https://doi.org/10.1027/1015-5759/a000191.
-
18.
Barke A, Riecke J, Rief W, Glombiewski JA. The Psychological Inflexibility in Pain Scale (PIPS) - validation, factor structure and comparison to the Chronic Pain Acceptance Questionnaire (CPAQ) and other validated measures in German chronic back pain patients. BMC Musculoskelet Disord. 2015;16:171. [PubMed ID: 26215038]. [PubMed Central ID: PMC4517641]. https://doi.org/10.1186/s12891-015-0641-z.
-
19.
Polit DF, Beck CT. Nursing research: Principles and methods. Lippincott Williams and Wilkins; 2004.
-
20.
Headache Classification Committee of the International Headache S. The international classification of headache disorders, 3rd edition (beta version). Cephalalgia. 2013;33(9):629-808. [PubMed ID: 23771276]. https://doi.org/10.1177/0333102413485658.
-
21.
Wicksell RK, Renofalt J, Olsson GL, Bond FW, Melin L. Avoidance and cognitive fusion--central components in pain related disability? Development and preliminary validation of the Psychological Inflexibility in Pain Scale (PIPS). Eur J Pain. 2008;12(4):491-500. [PubMed ID: 17884643]. https://doi.org/10.1016/j.ejpain.2007.08.003.