1. Background
Asthma is a chronic inflammatory disease of the airways of the lung, affect more than 300 million people in the world (1). It is a common chronic disease which is remarkably pathogenic. The prevalence of ever asthma has been reported from 2.7% to 3.5% but wheezing in the past 12 months’ were 7.6% and 10.7% in children aged 6-7 and 13-14 years, respectively (2). In a study conducted in the North of Iran, the prevalence of asthma and wheezing has been recorded as 12% to 30% in elementary and guidance schools (3-5). Intelligence quotient (IQ) in children with moderate asthma is similar to healthy children but this disorder has a significant financial burden on family and country (6, 7). A child with asthma maybe hospitalized several times that this issue can be stressful for both parents and children due to disrupting the way of life and normal functions. When parents feel competent and mighty, they will be able to provide support for their sick children. Parents often due to the lack of awareness about the origin of the sickness, how to perform medical procedures, economic consequences of the child disease, the imposed pain on the child during the illness, uncertainty about the future of the disease, and the risk of contagion experience feelings of anger, anxiety and guilt. These parents show their anxiety with inappropriate behavior, restlessness, irritability and isolation (8). A chronic course of asthma induces morbidity and mortality. Consequently, it creates a significant impact on children's anxiety and thus aggravated asthma (9). Calam et al. showed providing advices to the families about the management of children's behavior have been very useful, especially when parents have not any experience about the asthma disease (10, 11).
Ghaempanah et al. showed that depression among mothers of children with asthma is more common. Furthermore, improving the level of asthma control did not influence on improving mothers' maternal health (12).
In a study conducted by Silver et al., showed that asthma caregivers were more anxious, but the severity of asthma symptoms with depression, anger and cognitive imbalance did not relate with general distress of the caregivers (13).
In a survey that was done by Zhou T et al., showed that the families with low socio-economic level, low performance of caregivers is related to their high levels of anxiety and depression (14). Brown et al. showed increase the prevalence of asthma and deaths from among caregivers of children with Asthma with psychological symptoms. Frequency of hospitalizations due to asthma related with total scores of questionnaire, as well subcategories of depression, anxiety and somatic symptoms (15).
In the present study, we decided to evaluate the relationship between anxiety severities of caregivers of children with their disease severity.
2. Objectives
Due to the high prevalence of anxiety and depression in Iranian people especially in parents of children with chronic diseases and also, because of the high prevalence of asthma, the present study was designed to evaluate the relationship between the parental anxiety intensity and the children's asthma severity.
3. Materials and Methods
This study is a cross-sectional study with 134 patients according to the previous studies (9, 11, 12) and based on consideration of error of less than half a percent and a power of 80%. Selection of our patient was continuous sampling. Children (5-15 years old) with allergic asthma which confirmed by allergist and clinical immunologist referring to educational allergy clinic in Sari during the fall and winter in 92. The researcher explained the aim of the study for participants and their parents have completed the informed consent form. Children who had other diseases besides asthma were excluded from the study.
Beck questionnaire was used to assess parental anxiety. This questionnaire included 21 items that cover most common symptoms of anxiety. The subjects respond the amount of their resentment in the last week by putting crosses in the column before. Method of scoring answers Never [0], mild, medium [2] and severe [3]. Thus the range of scores was from 0 to 63 and it can be classified based on points [0-7] minimal, [8-15] mild, [16-25] average, and [25-63] severe (16).
Reliability and validity of the questionnaire were evaluated and approved at different age and sex in Iran (17). To assess the severity of asthma in children questionnaire of Global Initiative for Asthma (GINA) was used (18). This questionnaire evaluated the frequency of attacks of asthma and asthma severity (during a month in the current year), Severity (mild, moderate and severe), severity of attacks (mild, moderate and severe), the need for medication FEV1/FVC(forced expiratory volume/forced vital capacity) (during the day), number of hospitalizations or going to the emergency department (during the current year), the number of missed school days due to exacerbation of the illness (within three months).
Demographic characteristics of parents were expressed with descriptive statistics. The relationship between parental anxiety and severity of asthma in children assessed by Kendall Tau and Gamma analyzer was used. Data were analyzed by using SPSS 16.
4. Results
One hundred and thirty four people participated in this study. The average age of participants was 36.17 years old that 90% of them mothers and 10% of them were the fathers of children with asthma. The average age of the children was 40.2 ± 7.9 months. Ten percent of children have experienced asthma attack once, about 72% two times or three times, 16.5% four times, and less than 1 percent five times during the past year. Severity attacks of 23.88% of children were mild and 76.12 % of them were moderate. 2.14% of children need for one-time use of the drug, 67.9 % of them twice, 15.7 % three times and 2.2 % four times use of the drug. 2.67% of children did not mention the history of hospitalization due to asthma attacks during the past year. 17.9% of children one time and 14.9% two times mentioned the history of hospitalization due to asthma attacks.
22.4% of children reported missing the school onetime and 9.7% missed the school two times during the past three months due to exacerbation of asthma attacks, and 67.9% of did not miss the school during the last one month due to exacerbation of asthma attacks. FEV1/FVC was in the normal range (> 80%) in 5.4%. In 47% of children the ratio was between 80% to 85% (mild asthma), and in 48.5% of children the ratio was between 60% to 80% (moderate asthma).
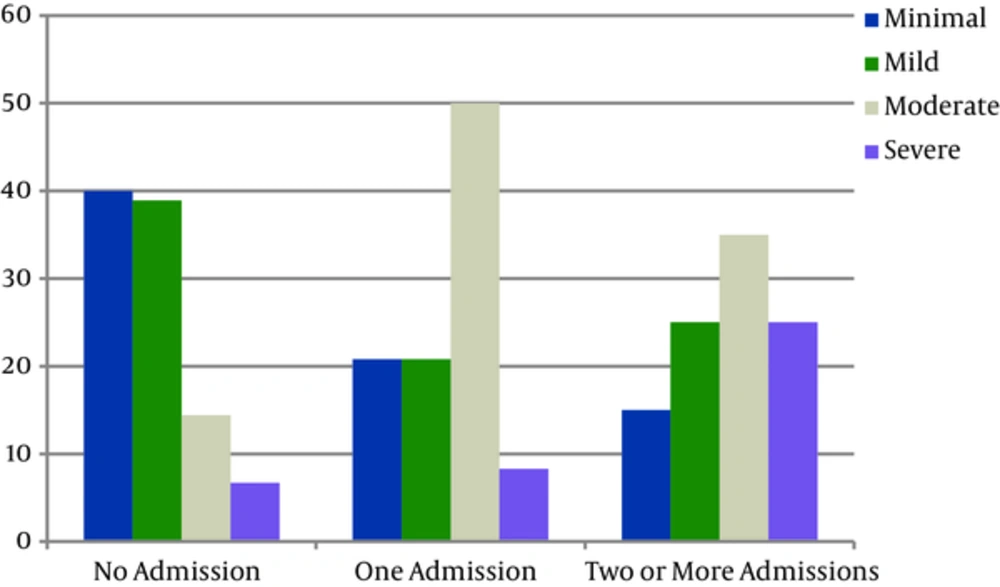
Beck Anxiety Inventory score of parents 32.8% was less than 7 (minimal anxiety), and scores of 33.6%, 23.9% and 9.7% respectively were 8 to 15, 16 to 25 and greater than 26 respectively. Kendall Tau B and Gamma test showed that there is a significant relationship between the number of admissions (P < 0.0001) and the number of attacks (P < 0.0001) with parental anxiety (Figure 1).
Kendall Tau and Gamma test showed a significant correlation between FEV/FVC and the Beck test scores of parents (P > 0.0001). The Beck test scores and other measures of asthma showed a significant relationship between the severity of asthma including the times of using salbutamol (P > 0.0001), school absences (P = 0.02), and attack intensity (P > 0.0001).
| Variables | No. (%) | |
|---|---|---|
| Mean age of the children | 9.07 ± 2.40 | |
| Asthma attack, N | 1 | 14 (4.10) |
| 2 | 61 (5.45) | |
| 3 | 36 (9.26) | |
| 4 | 22 (4.16) | |
| 5 | 1 (07.) | |
| Medication, dose/day | 1 | 19 (2.14) |
| 2 | 91(9.67) | |
| 3 | 21 (7.15) | |
| 4 | 3 (2.2) | |
| Hospitalization, N | 0 | 90 (2.67) |
| 1 | 24 (9.17) | |
| 2 | 20 (9.14) | |
| Missing the school, d | 0 | 91 (9.67) |
| 1 | 30 (4.22) | |
| 2 | 13 (7.9) | |
| Severity of attacks | Slight | 32 (88.23) |
| Moderate | 102 (12.76) | |
| FEV/FEC | 85 < | 6 (5.4) |
| 85 - 80 | 63 (47) | |
| 80 - 75 | 65 (5.48) | |
| Parents, % | 134 | |
| Mothers | 90 | |
| Fathers | 10 | |
| Age of parents (mean), y | 36.17 ± 5.16 |
5. Discussion
The results of this study showed that 33.6% of parents of children with asthma had moderate to severe anxiety. In a study that was done by Ghaempanahv et al., mothers of children with asthma reported symptoms of depression more than normal levels of society (P < 0.001) (12). In this study, there was a significant relationship between parental anxiety scores and measures of asthma severity (Including the number of attacks per month in the last year, intensity of the attacks, the need of using the drug, FEV1/FVC, the number of admissions during the last year and the number of school absences during the last 3 months) was observed in children. The findings of study of Silver et al. showed that caregivers who their children in terms of severity of asthma symptoms were classified with moderate-severe, were more anxious than other caregivers (13).The result of this study suggested that there is a relation between parental anxiety and admissions of children with asthma. This finding is in line with the study of Brown et al. (15).In their study used Brief Questionnaire which contains sub-categories somatic, anxiety and depression. Frequency of hospitalizations due to asthma attacks during the last 12 months was significantly higher than children whose careers had lower scores in Brief Questionnaire.
Their study results showed that the frequency of hospitalizations due to asthma was associated with total scores of questionnaire and with subcategories of depression, anxiety and somatic symptoms. Parental anxiety may be due to child care responsibilities or may be a duty of care for children with asthma (15). Cross-sectional and longitudinal studies indicate a relationship between maternal anxiety and asthma. Although it’s effective mechanism and their relationship is not recognized correctly. Epidemiological studies suggest that anxiety during pregnancy and after giving birth predict the development of childhood asthma. The proposed mechanism is changes in gene expression that regulate immune responses and the hypothalamic-pituitary-adrenal axis. On the other hand, maternal anxiety and asthma kids may not have the cause-effect relationship. For example, the relationship between asthma and anxiety may be due to the environmental stressors (Shared environment) in the family or the family creates stress in children (11).
The possibility of having a child with asthma is higher in mothers who have experienced anxiety and depression during pregnancy and after childbirth or other times. There is also evidence of reverse causality relationship. This means that, caring of children with eczema and asthma with higher levels of depression, anxiety, sleep deprivation and reduced quality of life of parents of children with asthma (10).
Sometimes, it is necessary a child to be hospitalized several times during the course of chronic diseases and this can be stressful for their parents. Parents as the most important people in the child support system can transmit Stress and anxiety to their children (4-6).
In our study, there was a significant relationship between the parental anxiety and number of attacks, attack intensity, need to use the drug, FEV1/FVC, absence from school, the hospital admissions of their children.
This study had some limitations that are as follows; being a cross-sectional study, and we cannot speak with certainty about the causality relationship between asthma and anxiety. The second was the lack of a control group in this study and also we did not mention psychiatric history of parents.
The results of this study show a high prevalence of anxiety in parents of children with asthma and its relation with the severity of asthma. Therefore, it is suggested specialists to better control asthma do some interventions to control the anxiety of parents of children with asthma at a lower level. It is also suggested that in future studies the effect of parental anxiety treatment through the interventions such as behavior therapy, pharmacotherapy on the severity of asthma be evaluated.