Abstract
Keywords
Lipomatosis Ileum Ileocecal Valve Multidetector Computed Tomography
1. Introduction
Lipomatosis of the gastrointestinal tract is a rare condition with a small number of cases. The term lipomatosis describes focal proliferation of normal fat in the soft tissue including the mediastinum, kidneys, pelvis, or the intestine (1). Intestinal lipomatosis is the infiltration of the submucosa by mature fat tissue without tumor formation (2). We are able to obtain higher quality images with the development of radiological imaging technologies. Pathologic conditions can be diagnosed and learned better with coronal and sagittal reformatted images of multidetector computed tomography (MDCT), a product of this technology. Here we report lipomatosis of the terminal ileum and ileocecal valve diagnosed with MDCT.
2. Case report
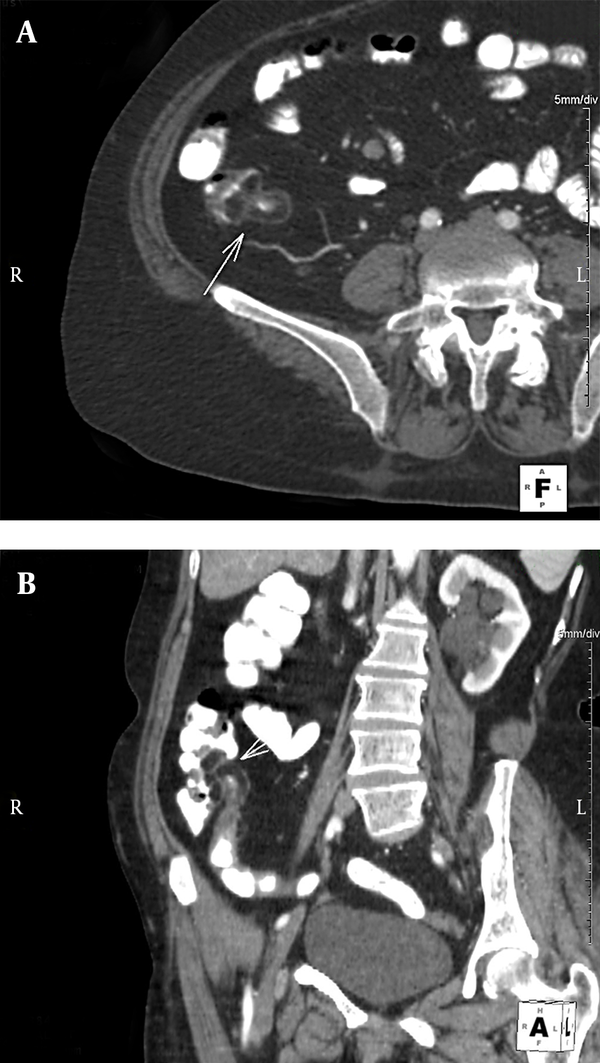
A 70-year-old woman presented with abdominal pain to the general surgery room. Clinical examination was unremarkable. Laboratory blood analysis revealed normal blood profile. Colonoscopy was normal in suboptimal conditions because of endoluminal gaita. Hepatosteatosis, gallbladder stones and bilateral renal cysts were detected on ultrasound examination. Abdominal computed tomography (CT) examinaton was performed with 64-row CT unit (Aquilion 64, Toshiba Medical Systems, Tokyo, Japan). It revealed intramural fatty infiltration of the terminal ileum and ileocecal valve (Figure 1). The density of the lesions was between -70 and -90 Hounsfield units (HU). Luminal narrowing at these sites was the secondary finding, but the contrast passage was present. A few number of millimetric diverticules were also present in the descending and sigmoid colon.
A 70-year-old woman with lipomatosis of terminal ileum and ileocecal valve. Intravenous contrast enhanced MDCT scans: A) Axial reformatted image; B) Coronal oblique reformatted image. They show diffuse intramural fatty infiltration in the terminal ileum and ileocecal valve (arrows). Note parapelvic cysts in the left kidney in Figure.B.
3. Discussion
Abnormal fatty tissue deposits in the intestine can be seen in the forms of single or multiple lipomas or diffuse adipose tissue infiltration of the submucosa without tumor formation. The latter one is called lipomatosis (2). Lack of encapsulation differentiates it from lipoma (3). The fatty tissue proliferation and deposition is usually limited to the submucosal layer, but it may extend to the serosa and mesenteric fat. The cause of the fat deposition is not known (2).
Intestinal lipomatosis shows no sex predominance, and it occurs usually after the fourth decade of life (1, 3, 4). Colon is the most common site (%65-75) and ileum is the second most common site in terms of lipoma (5). No predilection site has been mentioned for lipomatosis in the literature. The majority of cases are asymptomatic. When they reach bigger sizes, the symptoms usually start (6). The most common manifestations are nonspecific abdominal pain, constipation, diarrhea and bleeding (3, 6, 7). Abdominal pain was the only symptom in our patient, there was no gastrointestinal bleeding. Obstruction, intussusceptions and massive hemorrhage are rare findings (6).
The ileocecal area may be affected by many pathologic conditions such as benign and malignant tumors, inflammatory processes (appendicitis, diverticulitis, Crohn disease), and infectious diseases. So, the differential diagnosis is important in the lesions detected in this area. MDCT is the best imaging modality considered to evaluate the ileocecal area (8). Intestinal lipomatosis is shown as well-defined homogeneous intramural hypodense areas with an attenuation between -80 and -120 HU (1, 5). It can be differentiated from true lipoma, which appears as an asymmetric mass, whereas lipomatosis manifests as symmetric enlargement (5, 8). Thumb-printing of fluid-containing bowels is seen in coronal magnetic resonance images. The same sign can also be seen in intestinal ischemia, but intestinal wall thickness is normal in lipomatosis (1). No treatment is required since it is usually asymptomatic (7). When it reaches big sizes and obstruction develops, surgical procedures may be necessary for treatment. Derotation is performed in the presence of intussusception (1).
Coronal and sagittal reformatted images are added and larger areas with thinner sections can be examined with MDCT. It is the preferred diagnostic method for a rare, benign condition, such as intestinal lipomatosis, because it can differentiate fat tissue from other tissues.
References
-
1.
Komagata T, Takebayashi S, Hirasawa K, Fukawa T, Arai M. Extensive lipomatosis of the small bowel and mesentery: CT and MRI findings. Radiat Med. 2007;25(9):480-3. [PubMed ID: 18026907]. https://doi.org/10.1007/s11604-007-0162-2.
-
2.
Shenoy R, Rodrigues G, Gopashetty M, Kannaiyan L, Rao S. Segmental jejunal lipomatosis--a rare cause of intestinal obstruction. Yonsei Med J. 2003;44(2):359-61. [PubMed ID: 12728483].
-
3.
Bhupalan AJ, Forbes A, Lloyd-Davies E, Wignall B, Murray-Lyon IM. Lipomatosis of the ileocaecal valve simulating Crohn's disease. Postgrad Med J. 1992;68(800):455-6. [PubMed ID: 1437927].
-
4.
Suarez Moreno RM, Hernandez Ramirez DA, Madrazo Navarro M, Salazar Lozano CR, Martinez Gen R. Multiple intestinal lipomatosis. Case report. Cir Cir. 2010;78(2):163-5. [PubMed ID: 20478119].
-
5.
Thompson WM. Imaging and findings of lipomas of the gastrointestinal tract. AJR Am J Roentgenol. 2005;184(4):1163-71. [PubMed ID: 15788588]. https://doi.org/10.2214/ajr.184.4.01841163.
-
6.
Vasiliadis K, Katsamakas M, Nikolaidou A, Christoforidis E, Tsalis K, Tsalikidis A. Submucosal lipoma of the ascending colon as a source of massive lower gastro-intestinal bleeding: a case report. Acta Chir Belg. 2008;108(3):356-9. [PubMed ID: 18710116].
-
7.
Ormson MJ, Stephens DH, Carlson HC. CT recognition of intestinal lipomatosis. AJR Am J Roentgenol. 1985;144(2):313-4. [PubMed ID: 3871276]. https://doi.org/10.2214/ajr.144.2.313.
-
8.
Hoeffel C, Crema MD, Belkacem A, Azizi L, Lewin M, Arrive L, et al. Multi-detector row CT: spectrum of diseases involving the ileocecal area. Radiographics. 2006;26(5):1373-90. [PubMed ID: 16973770]. https://doi.org/10.1148/rg.265045191.
reply