Abstract
Keywords
1. Introduction
Lipomas are the most common benign tumors of the soft tissues. They are generally distributed in the subcutaneous areas of the body, but they may develop in all organs throughout the body. In the thoracic cavity, lipomas are rarely encountered. A pleural origin of lipoma is extremely rare (1). The incidence of pleural lipomas is not yet fully known. However, Jensen reported three cases of intrathoracic lipoma from a series of 3,502 cases of thoracic tumors (2) and Jaile reported five cases of intrathoracic lipoma from a series of 1800 patients who were undergoing thoracic exeresis (1). The hourglass-shaped thoracic lipomas are very rarely found (3-5). In his study, Ono identified 22 hourglass type lipomas from 114 cases of intrathoracic lipomas (6).
2. Case Presentation
We present the case of a 77-year-old Caucasian woman, non-smoker, who had signs and symptoms of acute tracheo-bronchitis (fever and cough with muco-purulent expectoration for a few days).
The clinical examination indicated a 6 cm-diameter anterior upper-left thoracic mass, painless, soft, non-adherent to the skin, with normal superjacent tissues. The patient observed a slowly progressive growth of it in the last 30 years. She did not have any major complaints related to the tumor. The patient’s body mass index was 31.25 kg/mp.
Laboratory examination showed leukocytosis with neutrophilia and elevated levels of C-reactive protein.
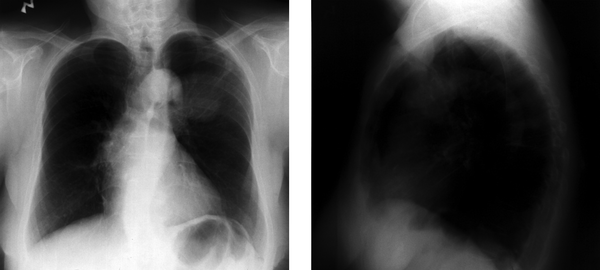
On the chest radiography (X-ray), a round opacity was observed in the left lung, projected on the topography of the anterior segment of the upper lobe (Figure 1).
Chest X-ray of a 77-year-old non-smoker Caucasian woman. She was admitted to the hospital with signs and symptoms of acute tracheo-bronchitis. Chest X ray showed a round opacity projected on the topography of the anterior segment of the upper lobe of the left lung. The patient had no complaints related to the tumor. According to the patient, the tumor appeared 30 years ago and was slow in growth.
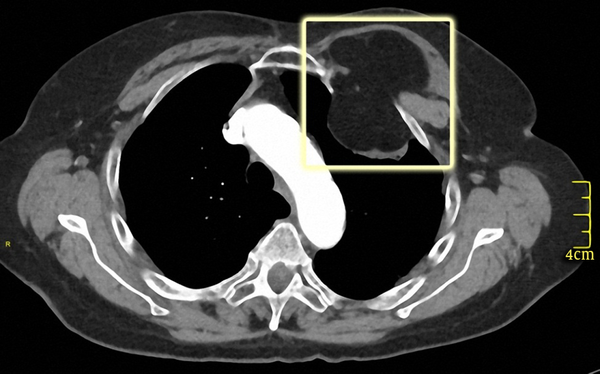
A computed tomography (CT) examination revealed an hourglass-shaped well-defined formation under the left clavicula, with fatty densities (-110 UH) and fine septa inside. The overall dimensions were 73 × 55 × 55 mm [anterior-posterior (AP)-transverse (T)-cranial-caudal (CC)]. Intravenous contrast medium injection provided no contrast enhancement. The formation extended into the chest, exerting a mass effect on lung parenchyma, with a perilesional atelectasis area. Intrathoracic dimensions were 47 × 47 × 41 mm (AP-T-CC). No rib erosion or destructive bone changes were observed (Figures 2 and 3). These findings were consistent with typical lipoma of the extrapleural fat.
CT images (axial view) demonstrating the hourglass-shaped mass of fatty density (-110 UH), homogeneous, without contrast enhancement (arterial phase)
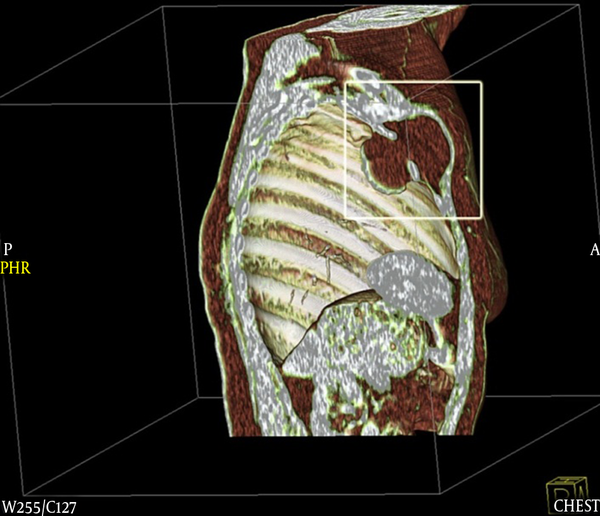
Three dimensional (3D) reconstruction of CT images, showing the passage of the tumor through the first intercostal space
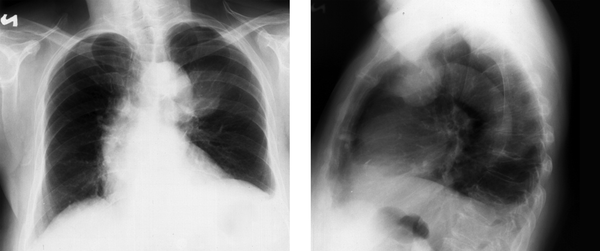
At the time, the patient refused any invasive approach. No biopsy or surgical excision was performed. After one year, a new chest X-ray was performed. No changes were observed (Figure 4). No significant anomalies were reported clinically and biologically. The patient still refused any intervention on the thoracic tumor.
Chest X-ray at 1-year follow-up demonstrates absence of any changes.
3. Discussion
Lipomas are common benign tumors of mesenchymal origin, slow-growing, well-defined and encapsulated (7). More than half of lipomas are distributed ubiquitously in the subcutaneous areas of the body, but they may develop in virtually all organs throughout the body.
A variety of lipoma exists. The vast majority are classic lipomas and consist only of mature adipose tissue. Some of them contain scattered fibrous connective tissue septa. The superficial classic lipomas are better circumscribed and smaller than the deeper lesions. The deep lipomas are far rarer. Because of the usual detection at a late stage of development, they tend to be larger then superficial ones. They are usually encountered in the chest wall, hand and feet. The variable shape is determined by the space they occupy, because they are forced to mold themselves around the surrounding tissues (8). Extremely rare, classic lipomas can arise on the surfaces of bone (parosteal lipoma) (9).
Rarer types of lipoma contain fat and nonadipose elements in varying proportions. Some of them have similar characteristics to malignant tumors of the soft tissue and pose real problems in diagnosis. Well-differentiated liposarcomas resemble lipomas on both CT and magnetic resonance imaging (MRI) (10, 11). These tumors do not metastasize. Instead, they locally recur after surgical removal and they may undergo dedifferentiation into a more aggressive and potentially metastasizing form of sarcoma (8, 12). Therefore, a thorough pathological examination is imperative. Sometimes a malignant component is difficult to exclude even on biopsy specimens (9, 13).
A lipomatous malignancy does not usually grow in the subcutaneous region; therefore, a deep-seated lipoma, including an intrathoracic lipoma, must be carefully differentiated from malignancies such as liposarcomas or metastatic lesions.
Lipomas are rarely encountered in the thoracic cavity and may originate from the diaphragm, mediastinum, bronchus, lung or thoracic wall (14, 15). A pleural origin of lipoma is extremely rare. It originates in the adipocytes of the visceral, parietal, thoracic or mediastinal pleura (1) and in rare occasions, it can infiltrate the intercostal space. An hourglass development through the intercostal space is possible, however the intrathoracic and extrathoracic dumbbell-shaped lipoma is a very rare finding (9).
Keeley and Vana (16) and Williams and Parsons (17) divided intrathoracic lipomas into two classes: (a) hourglass or dumbbell-shaped lipomas that pass through the thoracic inlet or intercostal space and (b) purely intrathoracic lipomas (9).
In our case, the hourglass-shaped lipoma originated from the left parietal pleura and passed outside the thorax through the first intercostal space. Intrathoracic, it exerts mass effect on the lung parenchyma, with the constitution of perilesional small atelectatic areas. The extrathoracic part of the lipoma exerts mass effect on the muscles. There is no CT evidence of rib erosion or local invasion.
Our patient was asymptomatic like most patients (except a small and painless bump on the anterior upper-left thoracic wall), but since lipomas are able to grow to a large size, non-specific symptoms due to compression may develop, depending on sites and sizes of the tumor mass. Compression symptoms are intermittent cough, mild chest pain, dyspnea, dysphagia or thoracic tightness sensation.
Between simple lipomas and well-differentiated liposarcomas there are major differences concerning treatment, prognosis and long-term follow-up, so it is mandatory to properly distinguish before surgery. Local or marginal excision is used to treat simple lipomas, while wide local excision is necessary for well-differentiated liposarcomas due to the high probability of local recurrence. A long-term follow-up is also required for well-differentiated liposarcomas because they may dedifferentiate after 5 to 10 years from the initial surgery (18, 19).
On the chest radiography, intrathoracic lipomas look like nodules or masses with rounded and smooth appearance. Unfortunately, conventional radiography cannot be used alone as an imaging method to separate benign from malignant pleural processes, nor to distinguish between pleural processes and parenchymal ones (9).
The modern diagnosis of intrathoracic lipomas is based on CT and MRI. These imaging methods allow the precise localization of the tumor and give information regarding the shape, homogeneous fat content, lack of vascularization and the relationship with nearby structures.
Classic lipomas consist only of mature adipose tissue, therefore they have CT imaging signal characteristics similar to those of subcutaneous fat. One can often identify a thin capsule and less than 2 mm thick septa. Simple lipomas may also contain muscle fibres, blood vessels and necrotic or inflammatory areas (12), making diagnosis more difficult because they mimic findings associated with well-differentiated liposarcomas. The CT diagnostic criteria for lipoma are: well-defined mass of homogeneous fat (-50 to -150 HU), absence of enhancement by an intravenous injected contrast medium, obtuse angles with the chest wall, displacement of the adjacent pulmonary parenchyma and blood vessels. The typical characteristics of a malignant tumor include: invasive growth, infiltration of surrounding structures rather than displacement, inhomogeneous enhanced by an intravenous injected contrast medium, attenuation values greater than -50 HU, poor delineation of the lesion and the occurrence of metastases (12). In our case, the CT images are unequivocal characteristic for lipoma.
In previously reported literature, dimensions of peripheral lipomas range between 10 mm and 130 mm (20). In our case, the overall dimension was 73 × 55 × 55 mm, with intrathoracic dimensions of 47 × 47 × 41 mm.
MRI is the modality of choice for imaging lipomas, especially when atypical features suggest liposarcoma. The MRI characteristics of the lipoma are: homogeneous fatty mass, no or few thin septa, no or mild linear enhancement, and no or minimal areas of high T2 signal (12). Persistent areas of high T2 signal are worrisome. In our case, we considered that CT characteristics are eloquent enough not to require further investigation by MRI.
The therapeutic approach has not yet reached a unanimous consensus. Because lipomas are benign tumors, a non-surgical approach may be reasonable as long as the imaging examinations reveal no lesion growth. In elderly and frail patients, if the pleural lipomas are small and asymptomatic, the clinical and radiological follow-up may be a good therapeutic option (9). The indication for surgery is a matter of debate (1). In the past, surgery was not usually indicated, except when the tumor was large and caused compression symptoms. Today most authors advocate surgical removal of the intrathoracic lipomas because the possibility of underdiagnosed liposarcoma. In our case, considering the benign CT appearance of the tumor and taking into account the patient's option, we proceed by imaging follow-up.
In conclusion, Intrathoracic lipomas are not a common pathology, much less the intrathoracic and extrathoracic hourglass type. The history of our patient, the imaging investigations (serial chest X-ray, and CT scan) support the benign and lipomatous nature of the tumor. In our case, the small size of the lipoma compared to the long duration of its evolution and the absence of any signs and symptoms of intra-thoracic compression was detected. So, a non-surgical approach could be safely adopted in this case. The taken therapeutic approach complies with the patient’s options while fitting in the current generally accepted recommendations.
The etiologic diagnosis of a lung opacity triggers a chain of complex investigations. The result is sometimes surprising. In our case, the opacity has proven to be a dumbbell-shaped lipoma.
Acknowledgements
References
-
1.
Jayle C, Hajj-Chahine J, Allain G, Milin S, Soubiron L, Corbi P. Pleural lipoma: a non-surgical lesion? Interact Cardiovasc Thorac Surg. 2012;14(6):735-8. [PubMed ID: 22371386]. https://doi.org/10.1093/icvts/ivs052.
-
2.
Jensen MS, Petersen AH. Bronchial Lipoma:Three Cases and Review of the Literature. Scand J Thorac Cardiovasc Surg. 2009;4(2):131-4. https://doi.org/10.3109/14017437009134253.
-
3.
Shimoyama T, Kimura B. Hourglass Transmural Lipoma; Report of a Case. Kyobu Geka Japanese J Thorac Surg. 2016;69(10):885-7.
-
4.
Matsuoka T, Fukamitsu G, Onoda M, Uesugi N, Kawano K, Kato T. Hourglass transmural lipoma; report of a case. Kyobu Geka Japanese J Thorac Surg. 2011;64(2):165-8.
-
5.
Givigliano F, La Rocca A, La Manna C, Busiello L, Longo F, Scognamiglio F, et al. Minimally invasive combined approach for an hourglass-shaped mass at the thoracic inlet. J Thorac Cardiovasc Surg. 2007;134(2):528-9. [PubMed ID: 17662811]. https://doi.org/10.1016/j.jtcvs.2007.03.019.
-
6.
Ono M, Tsuda K, Sasagawa N, Satoh M, Ikeda K, Sudoh K. An hourglass type intrathoracic lipoma--a case report of surgical treatment. Zasshi J Nihon Kyobu Geka Gakkai. 1993;41(9):1556-61.
-
7.
Cakmak H, Bayram FC. A giant intrathoracic and extrathoracic dumbbell-shaped lipoma. Eur J Cardiothorac Surg. 2010;37(3):735. [PubMed ID: 19818640]. https://doi.org/10.1016/j.ejcts.2009.09.016.
-
8.
Munk PL, Lee MJ, Janzen DL, Connell DG, Logan PM, Poon PY, et al. Lipoma and liposarcoma: evaluation using CT and MR imaging. AJR Am J Roentgenol. 1997;169(2):589-94. [PubMed ID: 9242783]. https://doi.org/10.2214/ajr.169.2.9242783.
-
9.
Zidane A, Atoini F, Arsalane A, Traibi A, Hammoumi M, Ouariachi F, et al. Parietal pleura lipoma: a rare intrathoracic tumor. Gen Thorac Cardiovasc Surg. 2011;59(5):363-6. [PubMed ID: 21547634]. https://doi.org/10.1007/s11748-010-0650-7.
-
10.
Kransdorf MJ, Moser RJ, Meis JM, Meyer CA. Fat-containing soft-tissue masses of the extremities. Radiographics. 1991;11(1):81-106. [PubMed ID: 1996399]. https://doi.org/10.1148/radiographics.11.1.1996399.
-
11.
Jelinek JS, Kransdorf MJ, Shmookler BM, Aboulafia AJ, Malawer MM. Liposarcoma of the extremities: MR and CT findings in the histologic subtypes. Radiology. 1993;186(2):455-9. [PubMed ID: 8421750]. https://doi.org/10.1148/radiology.186.2.8421750.
-
12.
Gaskin CM, Helms CA. Lipomas, lipoma variants, and well-differentiated liposarcomas (atypical lipomas): results of MRI evaluations of 126 consecutive fatty masses. AJR Am J Roentgenol. 2004;182(3):733-9. [PubMed ID: 14975977]. https://doi.org/10.2214/ajr.182.3.1820733.
-
13.
Sakurai H, Kaji M, Yamazaki K, Suemasu K. Intrathoracic lipomas: their clinicopathological behaviors are not as straightforward as expected. Ann Thorac Surg. 2008;86(1):261-5. [PubMed ID: 18573434]. https://doi.org/10.1016/j.athoracsur.2008.03.052.
-
14.
Politis J, Funahashi A, Gehlsen JA, DeCock D, Stengel BF, Choi H. Intrathoracic lipomas. Report of three cases and review of the literature with emphasis on endobronchial lipoma. J Thorac Cardiovasc Surg. 1979;77(4):550-6. [PubMed ID: 423588].
-
15.
Sen S, Discigil B, Badak I, Gurcun U. Lipoma of the diaphragm: a rare presentation. Ann Thorac Surg. 2007;83(6):2203-5. [PubMed ID: 17532428]. https://doi.org/10.1016/j.athoracsur.2007.01.040.
-
16.
Keeley JL, Vana AJ. Lipomas of the mediastinum; 1940 to 1955. Surg Gynecol Obstet. 1956;103(4):313-22. [PubMed ID: 13360666].
-
17.
Williams WT, Parsons WH. Intrathoracic lipomas. J Thorac Surg. 1957;33(6):785-90. [PubMed ID: 13429696].
-
18.
Weiss SW, Rao VK. Well-differentiated liposarcoma (atypical lipoma) of deep soft tissue of the extremities, retroperitoneum, and miscellaneous sites. A follow-up study of 92 cases with analysis of the incidence of "dedifferentiation". Am J Surg Pathol. 1992;16(11):1051-8. [PubMed ID: 1471725].
-
19.
Lucas DR, Nascimento AG, Sanjay BK, Rock MG. Well-differentiated liposarcoma. The Mayo Clinic experience with 58 cases. Am J Clin Pathol. 1994;102(5):677-83. [PubMed ID: 7942636].
-
20.
Hirata T, Reshad K, Itoi K, Muro K, Akiyama J. Lipomas of the peripheral lung--a case report and review of the literature. Thorac Cardiovasc Surg. 1989;37(6):385-7. [PubMed ID: 2694442]. https://doi.org/10.1055/s-2007-1020360.
reply