1. Introduction
Giant cell tumor accounts for 5% - 10% of all primary bone neoplasms. It can be locally aggressive or even metastase to distant organs such as the lungs as the most common site (1). However, its metastasis does not mean poor prognosis and metastatectomy is a way to cure these patients (1).
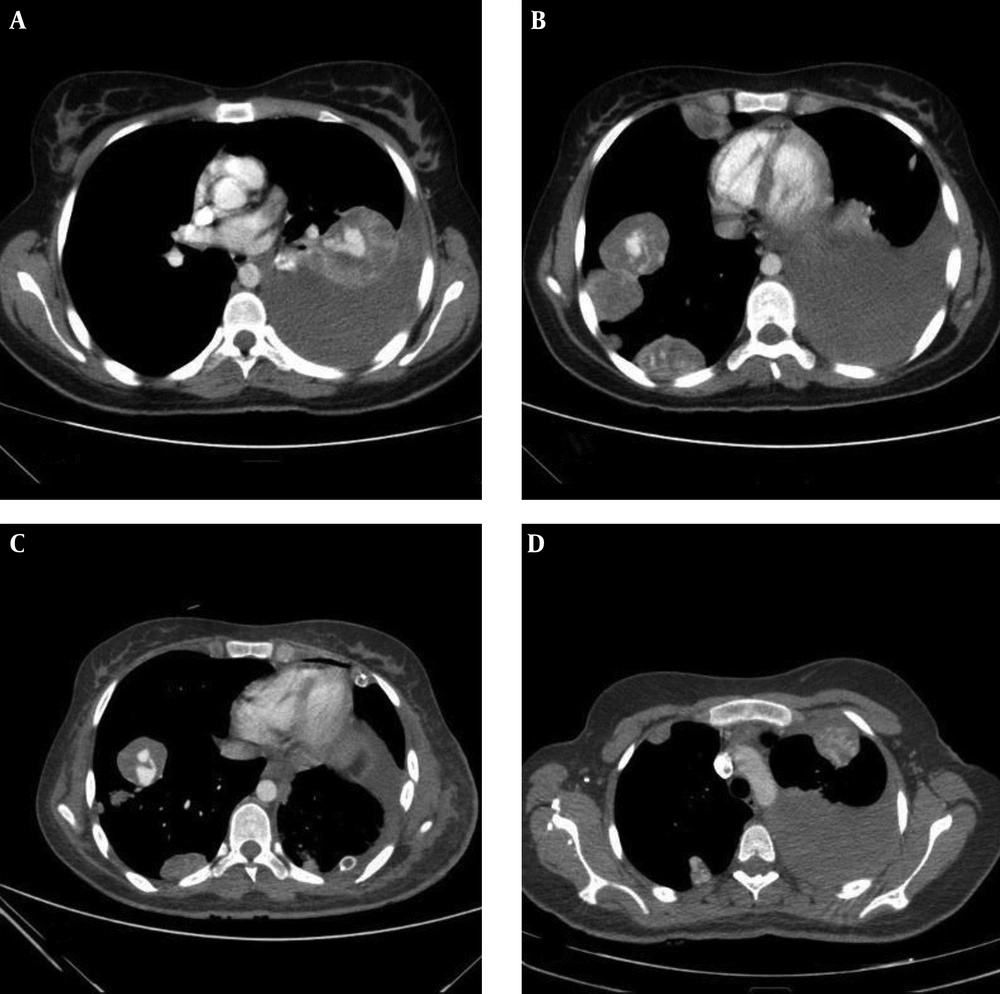
In our presented case, computed tomography scan (CT scan) showed varicose vessels within multiple lung metastases a rare radiologic feature. To the best of our knowledge, only one case of such manifestation has been reported (2).
2. Case Presentation
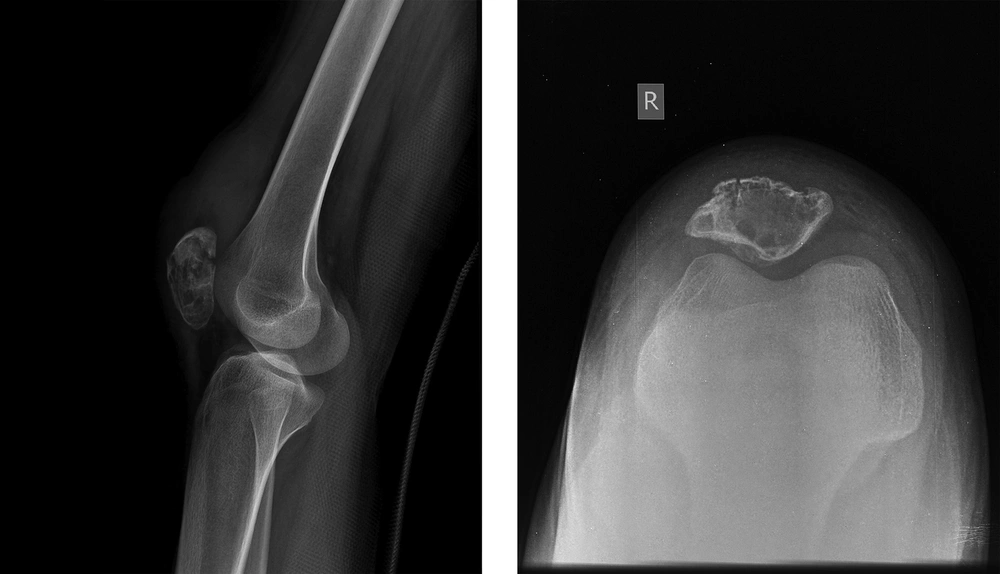
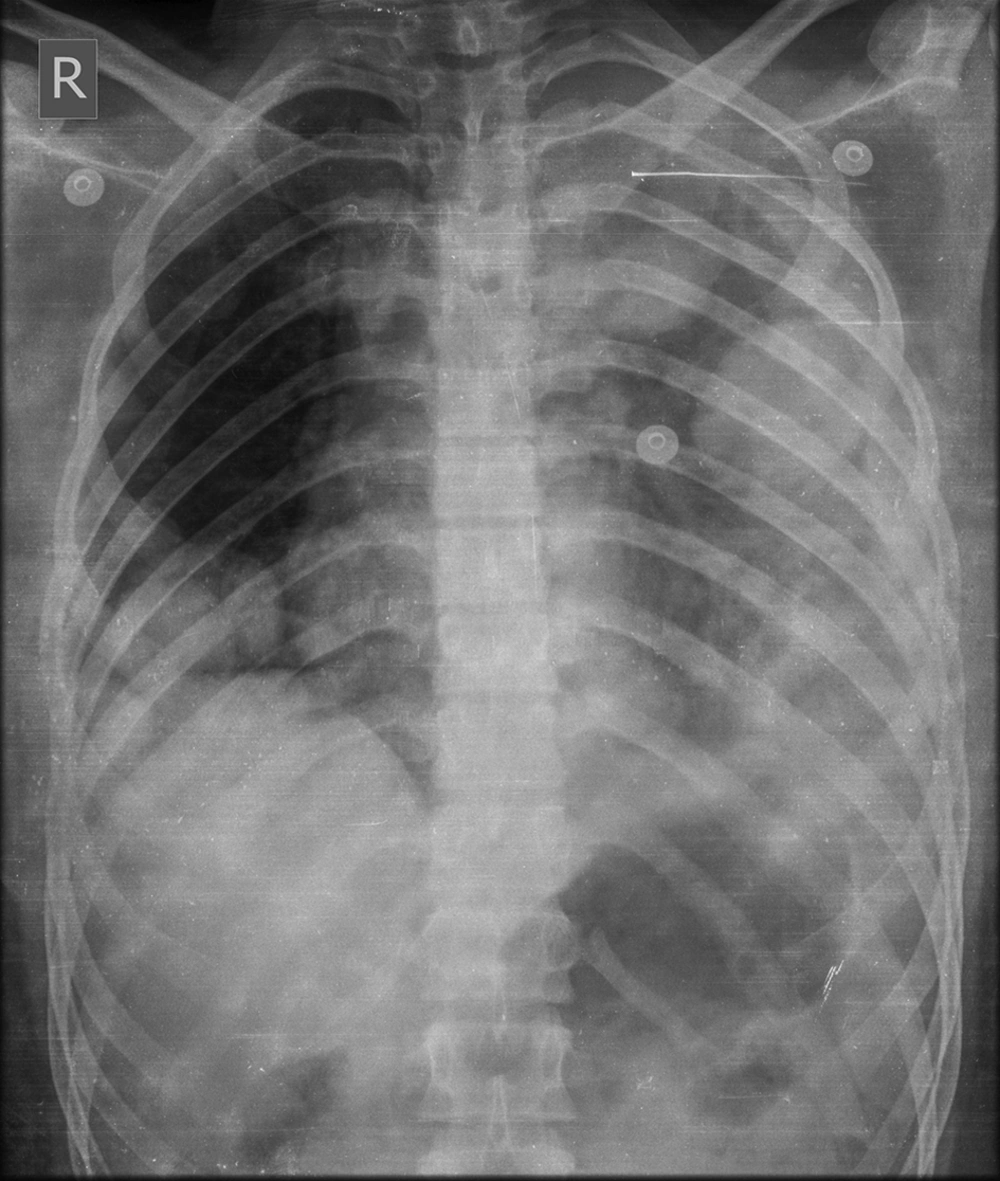
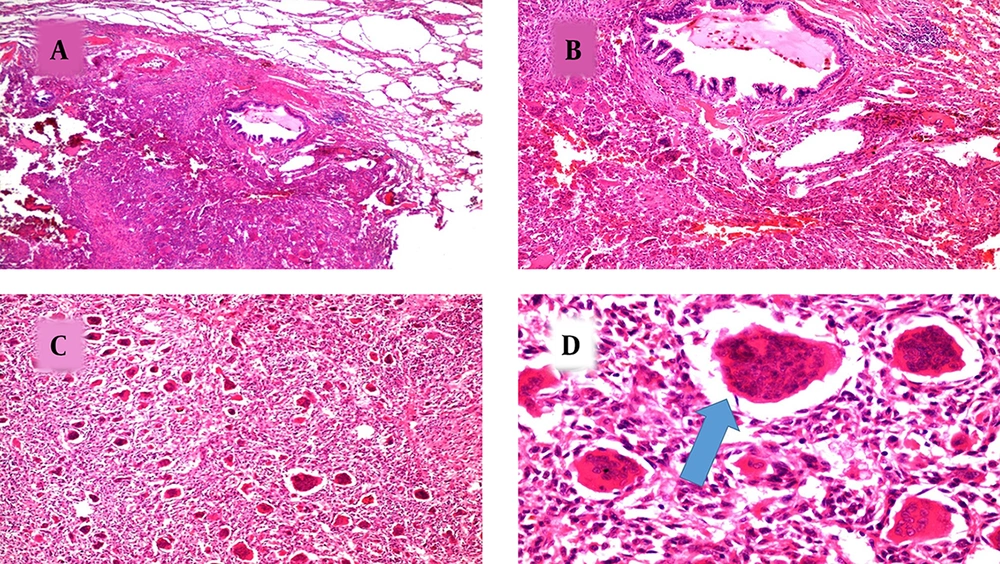
A 19-year-old female was diagnosed with giant cell tumor of the patella two years ago after severe right knee pain. She had no fever or weight loss. Her family history was negative for bone tumors. Physical examination was unremarkable except for tenderness over the right patella. Her initial X-ray of the right knee showed a lytic lesion with a narrow zone of transition and non-sclerotic border in the right patella. The overlying cortex was thinned but not eroded and no mineral calcification was found. There was also evidence of pathologic fracture within it (Figure 1). Surgical resection was performed. Histopathological examination confirmed giant cell tumor of the patella (Figure 2). She was on her routine follow up until one month prior to admission when she developed progressive dyspnea. Initial chest x-ray showed multiple varying size opacities in both lung fields with left sided pleural effusion (Figure 3).
A 19-year-old female with a history of giant cell tumor of the patella. Lateral and patellar views of knee X-ray demonstrate a lytic lesion with narrow zone of transition and non-sclerotic border in the right patella. The overlying cortex is thinned but not eroded and no mineral calcification is found. Evidence of pathologic fracture is also noted.
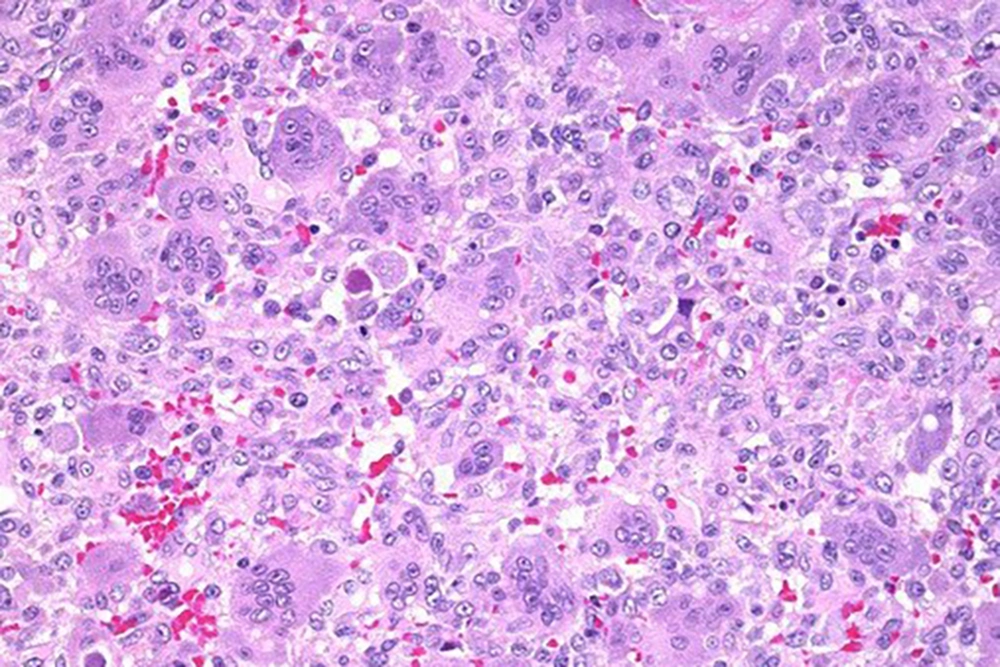
Multiple lung masses were revealed with engorged varicose vessels in contrast enhanced CT scan (Figure 4). Next, biopsy under the guide of CT scan was done, which revealed metastatic giant cell tumor (Figure 5). Knee MRI was performed, which revealed no local recurrence. Finally, she underwent exploratory thoracotomy with pneumolysis and metastatectomy, resection of masses was performed on the left side, and the future plan was to do the same thing on the right side.
Histopathological evaluation of the lung nodule. A and B, Microscopic section shows normal lung parenchyma involved by tumoral process in the lower part of the slide (H & E staining, ×40, ×100). C and D, Sections show evenly distributed giant cells (arrow) in the background of mononuclear cells. (H & E staining, × 100, × 400).
3. Discussion
Giant cell tumor is a benign bone tumor that accounts for 20% of all benign bone tumors. Its female/male ratio is 1.5:1, and most cases are 20 - 40 years old. The most common giant cell tumor (GCT) site is around the knee in the distal femur, proximal of tibia and distal radius (1, 3). Typical GCT is an eccentrically located lytic lesion with non-sclerotic border in long bones with sub articular extension (1). Patella is an unusual location of bone neoplasm. Radiologic features essentially cannot differentiate benign from malignant patellar neoplasm. However, the majority of its neoplasms are benign and giant cell tumor accounts for 33% of all patellar tumors (4). Usual clinical presentation of patellar GCT is knee pain with or without swelling (5).
In spite of GCT benign features, it can be locally aggressive or even metastase to soft tissues, liver, brain, and lung (1). 15% - 25% of patients present with local recurrence after initial treatment (5). Lung metastasis occurs in 1-6% of cases that occur within ten years, with the mean time of 3.5 years after the initial treatment either with or without local recurrence (6).
Lung is the most common site for giant cell tumor metastasis and occurs more probably in patients with a history of local recurrence or radiologically aggressive appearance of primary tumor (7). Both giant cell tumor and its pulmonary metastasis are benign and there is no correlation between the location of giant cell tumor and the risk of lung metastasis (8).
Due to successful treatment of giant cell tumor lung metastasis and the rare occurrence of it, wide surgical resection of primary tumor in order to prevent further metastasis is not recommended (3).
Radiologic features of lung metastasis include solitary or multiple homogeneous lesions. These masses usually have a narrow zone of transition with lung parenchyma and are predominately located in basal segments and periphery regions of the lungs (6). Hence, masses with feeding vessels and varicosity are extremely rare. Varicose vessels within pulmonary masses are also infrequent with only few cases ever been reported with possible mechanism of angiogenic factor created by masses (2, 9). In addition, varicose vessels within these metastases have the same radiologic appearance resembling arteriovenous malformation (AVM) (2). If diagnosed inaccurately, it can affect patient management significantly.
In non-contrast enhanced CT scan, these are homogeneous masses, and contrast enhanced CT scan is essential to show its feeding artery and draining veins (2). As these varicose vessels have the potential risk of bleeding during biopsy or even spontaneously that can lead to hemothorax (2), we recommend contrast enhanced CT scan after detecting lung metastasis in patients with giant cell tumor. Therefore, after treatment close follow up is necessary in order to have a proper diagnosis and management.