1. Background
Hepatitis is a common infectious disease and an important health issue with increasing trend (1). However, there are differences in prevalence rates worldwide and an increasing rate is seen in the majority of regions (2). Some types of hepatitis B and D subtypes that are transmitted from blood transfusion, shared syringe or sexual route may have chronic status, leading to hepatic dysfunction and cirrhosis (3).
Also, hepatitis patients have higher rate of diabetes, ESRD, obesity, and HIV infection leading to further decrease in their quality of life (4). Since hepatitis has high transmission rate, developing some therapeutic and preventive strategies is important (5), especially for those with blood-transfusion, such as hepatitis B, hepatits C, HIV1, HIV2, HTLV1, HTLV2, and syphilis (6, 7).
Tenofovir is a therapeutic approved by FDA for treatment of hepatitis B (8-10).
The most commonly reported side effects due to use of tenofovir disoproxil were dizziness, nausea, back pain, skin rash, itching skin, and diarrhea. Long term use of tenofovir is associated with nephrotoxicity and bone loss (11). However, the efficacy of this drug in Iranian patients has not been assessed.
2. Objectives
The purpose of this study was to determine the effect of tenofovir on DNA and HBe antigen in patients with chronic hepatitis B.
3. Methods
In this interventional open label trial study, 145 consecutive patients with chronic hepatitis B attending a Hepatitis Clinic at Labbafinejad hospital of Tehran, Iran in 2016 and 2017, who received tenofovir 300 mg daily (Tenobiovir 300- BAKHTAR BIOSHIMI CO.) were enrolled with goal-oriented sampling. Exclusion criteria were presence of other liver diseases, co-infection with other types of viral hepatitis, HIV infection, organ transplantation, immune deficiency, drug hyper-sensitivity, and patient dissatisfaction.
Data including age, gender, viral load (DNA), HBe antigen, duration of disease, hepatitis B vaccination history, family history of hepatitis, liver biopsy, risk factors (blood transfusion, having tatoo, having major surjury, history of phlebotomy, being an employee or inmate of prison, unsafe sexual contact, sharing needles and drug injection equipment, having direct contact with blood of an infected person, hemodialysis patients, health care workers and others exposed to blood products and needle stick devices, and donor of blood and organs), diagnosis-duration interval, and adverse effects (renal, gastrointestinal, cutaneous, and neurological) were collected by census manner in 51 patients, who were followed-up to one year using interview and lab results and the data were recorded in a checklist.
Data analysis was performed among 51 subjects by SPSS (version 13.0) software (Statistical Procedures for Social Sciences; Chicago, Illinois, USA). Chi-Square, paired- sample-T, and independent-sample-T tests were used and were considered statistically significant at P values less than 0.05.
4. Results
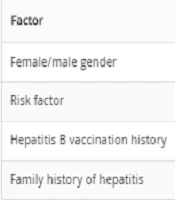
Among 51 patients, the mean age was 47.3 ± 11.9 years. The mean interval between diagnosis and treatment was 4.3 ± 5.6 years. Overall, 44 patients had risk factors for hepatitis B (25 persons (56.81%) had a history of major surgery, nine individuals (20.45%) had history of Phlebotomy, three individuals (6.81%) had history of transfusion, two cases (4.54%) had a tatoo, two cases (4.54%) had a history of sharing needles and drug injection equipment, two (4.54%) were inmate of prisons, and one (2.27%) had unsafe sexual contact. The common diagnostic route was accidental after blood donation. Other demographic data are presented in Table 1.
| Factor | Frequency | Percent |
|---|---|---|
| Female/male gender | 19/32 | 37.3/62.7 |
| Risk factor | 44 | 86.3 |
| Hepatitis B vaccination history | 7 | 13.7 |
| Family history of hepatitis | 20 | 39.2 |
Mean viral load before and after treatment was 31643426.761 ± 1553051.267 IU and 128.08 ± 434.12 IU respectively with a significant difference (P = 0.001); Table 2. The HBe antigen was positive in 7.8% and 2% before and after treatment, respectively, without a significant difference (P = 0.078). There were no adverse effects (renal, gastrointestinal, cutaneous, and neurological). Mean grade and stage were 5.3 and 4.2, respectively, in liver biopsy. Age, gender, hepatitis B vaccination history, family history of hepatitis, liver biopsy, risk factors, and diagnosis-duration interval had no effect on the results.
| Mean ± SD | |
|---|---|
| Viral load before treatment | 31643426.761 ± 1553051.267 |
| Viral load after treatment | 128.0784 ± 434.11956 |
5. Discussion
The purpose of this study was to determine the effect of tenofovir on DNA and HBe antigen in patients with chronic hepatitis B. The authors found that mean viral load before and after treatment was significantly decreased yet the HBe antigen was not different. The researchers found no case with drug-related adverse effects.
Duarte-Rojo and colleagues (12) reported that in Canada during year 2010, the efficacy of tenofovir in patients with chronic hepatitis B was 93%. However, they reported diarrhea and nausea in 11% and 8%, respectively. However, no adverse effects were seen in the current study. Pan et al. (13) showed that in the United States in 2014 the efficacy of tenofovir in patients with chronic hepatitis B was 79% to 83%. Similarly, they reported no adverse effect.
Also, Lovett et al. in Australia during year 2017, reported that efficacy of tenofovir in patients with chronic hepatitis B is 71% with mild and transient adverse effects (14). However, the results of the current study were better. Ahn et al. in South Korea during year 2017 reported that efficacy of tenofovir in patients with chronic hepatitis B is 80.4% with two severe adverse effects in 209 patients (15). Ke et al. (16) in china during year 2014 reported that efficacy of tenofovir in patients with chronic hepatitis B is 80% with mild and transient adverse effects. The current authors reported no adverse effects.
In total, according to the obtained results, it may be concluded that there is good effect for tenofovir on DNA yet not the HBe antigen in patients with chronic hepatitis B. The limitations of the current study were incomplete data that were excluded and also assessment in only one center that decreased the generalization of the results. However, further studies with larger sample sizes and multi-center sampling would develop further evidence with greater reliability and also generalization ability.