1. Background
Delirium is a neuropsychiatric syndrome, which is a common complication at the intensive care unit (ICU), especially found in older patients, and it is a risk factor for morbidity and mortality in this population (1-3). Delirium, which is presented in approximately 20% of hospitalized patients (2), is defined as an acute onset, fluctuating change, in mental status characterized by a reduced awareness of the environment and disturbance of attention, according to the diagnostic and statistical manual of mental disorders IV (DSM-IV) (4). Delirium leads to an increase in the duration of mechanical ventilation, by interfering with weaning, increasing the time of stay at the ICU, and decrease of functional outcomes. It is also associated with disturbance in consciousness, change in cognition, disturbed psychomotor activity, and abnormal sleep-wake cycle (5-9).
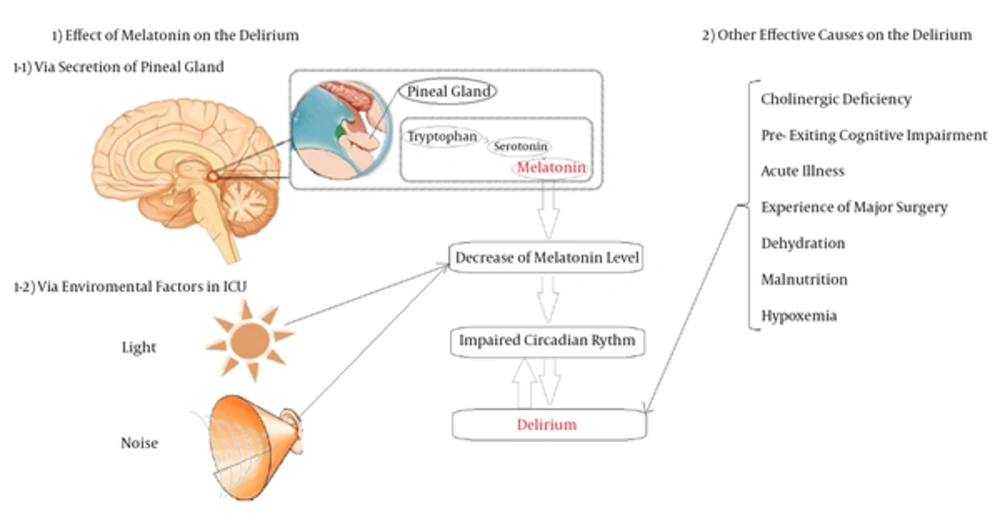
The etiology of delirium remains unclear, yet many risk factors have been associated with delirium, including age, patient’s history, pre-existing cognitive impairment, disruption of the circadian rhythm, acute illness, experience of major surgery, environment, dehydration, malnutrition, hypoxemia, severe concomitant diseases attributing to acid-base imbalance, metabolic disturbances, sensory deprivation, and the administered drugs (1, 5, 10, 11) (Figure 1).
1, Melatonin could affect delirium via two mechanism: 1-1, via secretion of the pineal gland; low levels of tryptophan, serotonin and melatonin are associated with an increased risk of delirium; and 1-2, via environmental factors at the ICU, such as light and noise, that with disturbance of circadian rhythm could lead to delirium. 2, Other effective causes on delirium include cholinergic deficiency, pre-exiting cognitive impairment, acute illness, experience of major surgery, dehydration, malnutrition, and hypoxemia.
Despite wide knowledge about delirium, its pathophysiology is still not fully understood (10). Cerebral metabolism dysfunction is one of its responsible mechanisms (12). Neurotransmission alternation and inflammation are influencing factors in the pathogenesis of delirium. Cholinergic deficiency appears to play a central role in the development of delirium. This hypothesis is supported by the effect of anticholinergic medication in increasing delirium symptoms while administration of acetylcholine esterase inhibitors have shown cognitive improvements (13, 14). Over-activity of the dopaminergic system is another mechanism in delirium pathophysiology (15). The increase in serotonergic activity and a relative deficiency of serotonin may also play an important role in the development of delirium (15-17). On the other hand, low levels of tryptophan may also lead to delirium. This amino acid acts as a precursor of some neurotransmitters, including serotonin and melatonin, therefore, low levels of tryptophan, serotonin, and melatonin are associated with increased risk of delirium (18, 19). Investigators have proposed that delirium may occur via 2 different mechanisms with alterations in tryptophan levels. This alternation may lead to the overproduction of neurotoxic metabolites or diversely in the production of melatonin (20, 21). In other words, the other effective mechanism might be the change in the circadian rhythms of the melatonin hormone, which is produced and secreted by the pineal gland (8, 10, 19).
Melatonin hormone is produced from serotonin by acetylation and methylation reaction in the pineal gland, and serotonin is produced from tryptophan by the hydroxylation reaction (22). Melatonin is the essential hormone for regulation of sleep cycle and it has other biological and physiological functions (23, 24). This process has been described in Figure 1.
Several causes could influence melatonin excretion rhythm, including systemic inflammatory response, hormone interactions, drugs, acuity of illness, mechanical ventilation, and environmental factors (25, 26).
Due to the high incidence of delirium in critically ill patients and a direct relationship between sleep disturbance, which may be caused by abnormal levels of melatonin and loss of circadian rhythms, several studies have been conducted to evaluate the level of melatonin and administration of exogenous melatonin or its agonists in this population (9, 17, 25, 27-31). The intention of this article was to review these conducted studies.
2. Methods
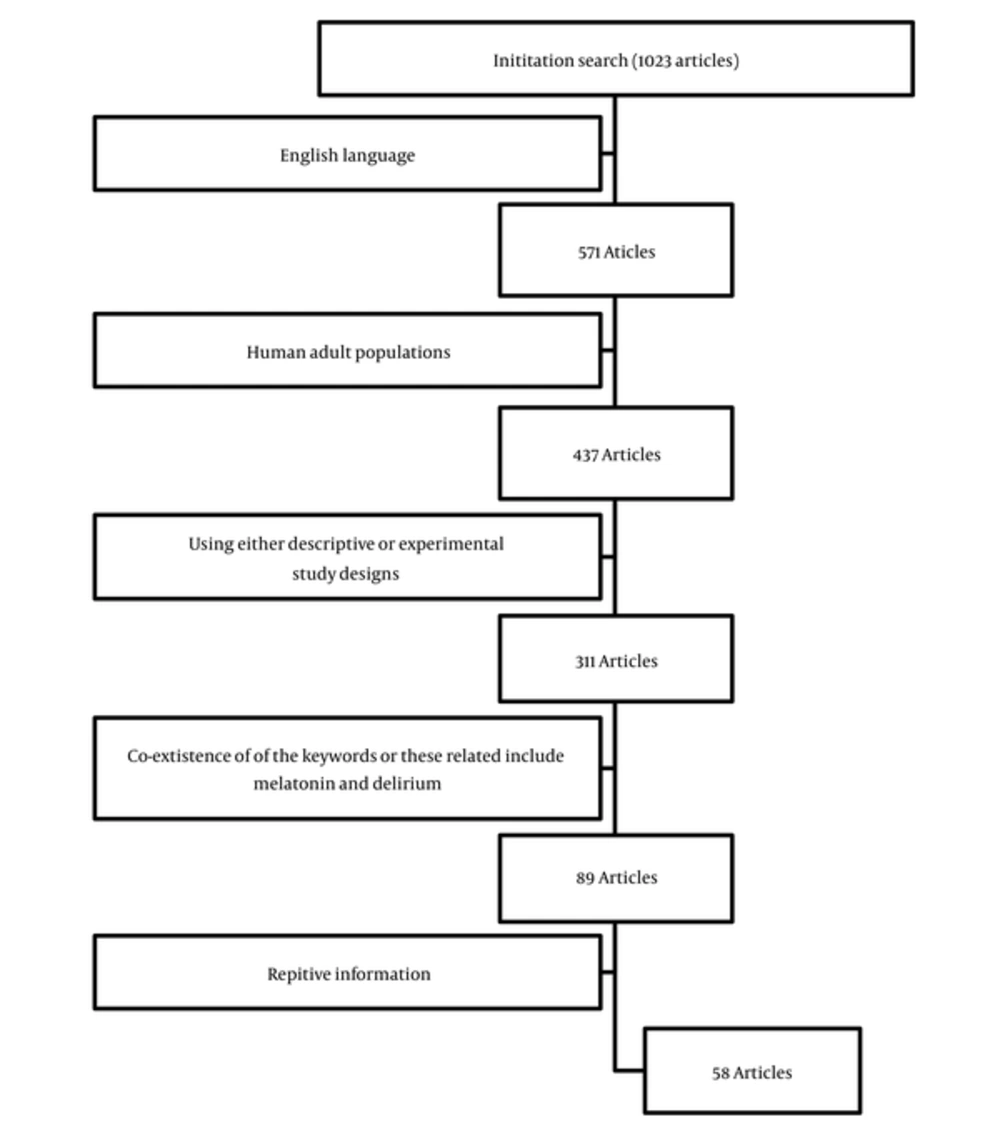
This review was designed to be applied across all types of research and evidence, including melatonin, melatonin agonist, delirium, pathophysiology f delirium, clinical trials of using melatonin at the ICU, effects of melatonin on delirium, and intensive care unit. Available data in Pubmed, Scopus, Medline, EMBASE, the Cochrane central register of controlled trials, and Cochrane databases were reviewed. Delirium is a common complication at the ICU and the current study only included studies on ICU patients that developed delirium.
The search retrieved 1023 articles, which were then filtered for articles using English language and human adult populations (18 years of age) using either descriptive or experimental study designs and using both melatonin and delirium as their key words. Review articles, case reports, and clinical studies were included. Ultimately, after the elimination of repetitive information, 58 articles were identified (Figure 2).
3. Results
3.1. Delirium
Delirium could be classified to 3 subtypes, including hyperactive, hypoactive, and mixed-type, based on the systematic clinical observation of hospitalized patients (32-34). In non-ICU patients, hyperactive delirium is recognized, while it is not observed in older patients (33, 35). In ICU patients, the most common types of delirium are mixed and hypoactive. Furthermore, hypoactive delirium is the major delirium witnessed in older patients (32, 33, 35). Melatonin degrades in the liver, and the metabolite of melatonin, 6-sulfatoxymelatonin (6-SMT), which is secreted in the kidney and could be directly measured (7). Given the known effects of melatonin, it appears that a relationship could exist between melatonin blood levels and/or a biochemical parameters (the urinary 6-SMT) and the subtypes of delirium, describing the low levels of urinary 6-SMT in hyperactive patients and the high levels of 6-SMT in hypoactive patients (7, 22, 25, 27).
Pharmacological and non-pharmacological approaches could be applied to prevent and control delirium in hospitalized patients (5, 36-38).
3.2. Melatonin in Delirium
Low levels of melatonin lead to an increase in the risk of delirium, therefore melatonin with a variety of doses has been used in studies that describe that the administration of melatonin could have beneficial effects, leading to prevention, management and improvement of delirium in critically ill patients with delirium (Table 1).
| Study | Type of Study | Dose of Melatonin, mg | Other Intervention | Duration of Study | Conclusion |
|---|---|---|---|---|---|
| Hanania et al. (29) | Case reports: 2 cases | 2 | - | 3 days | Prevention and management of delirium |
| Sultan (39) | RCT, N = 300 | 5 | The control group, 7.5 mg midazolam, 100 µg clonidine | Preoperative for 2 doses and postoperatively for 3 nights to those with postoperative delirium | A significant decrease in the percentage of post-operative delirium (9.43% vs. 32.65%) |
| Al-Aama et al. (40) | RCT, N = 145 | 0.5 | Placebo | 14 days or until discharge | A lower risk of delirium with melatonin (12.0% vs. 31.0%, P value = 0.014) |
| Lammers et al. (41) | Case reports | 2, twice per day | - | 14 days | Significant improvement in behavior |
| Jonghe et al. (42) | RCT, N= 378 | 3 | Placebo | 5 days | No effect of melatonin on the incidence of delirium, but led to long-lasting episode of delirium (> 2 days) (25.5% v. 46.9%; P = 0.02) |
| Chen et al. (6) | RCT, N = 669 | 0.5 - 5 | Surgical wards | 3 - 5 days | Decreased incidence of delirium |
| Medical wards | 7 - 14 days | ||||
| Clayton-Chubb et al. (43) | RCT, N = 36 | 5 | Placebo | 5 days or until discharge | Led to significant outcome benefits for delirious inpatients |
Hanania et al. (2002) described 2 cases; case 1 was a 53-year-old male with a history of Crohn’s disease, and had a hip pinning procedure and experienced postoperative delirium. His delirium ultimately improved with a daily intake of 2 mg of melatonin for 4 days. Case 2 was a 78-year-old male with a history of coronary artery disease and transient ischemic attacks, who had undergone a hip pinning procedure and experienced confusion, mild agitation, and sleep disturbance after the procedure. He was visited 3 years later for open debridement of an infected knee joint. He received 2 mg of melatonin before the operation and the same amount for 3 nights, postoperatively; therefore, he slept well and remained alert and oriented without confusion (29). Sherif S Sultan (2010) performed a controlled, randomized, double-blind study with 300 patients aged > 65 years old undergoing hip arthroplasty under spinal anesthesia. Patients were categorized to 4 groups, including the control group, 5 mg melatonin, 7.5 mg midazolam, and 100 µg clonidine. They received one dose at sleep time on the night of the operation and another dose 90 minutes pre-operatively. The results revealed a statistically significant decrease in the percentage of post-operative delirium to 9.43% (5 out of 53 patients) in the melatonin group versus 32.65% (16 out of 49 patients) in the control group. Finally, melatonin could decrease after the operation and played a successful role in treating more than half of the patients when administered postoperatively for 3 nights (39). Al-Aama et al. (2010) randomly assigned 145 acutely ill medical inpatients aged 65 years old. In this controlled, randomized, double-blind study, the patients were classified to 2 groups and received either 0.5 mg of melatonin or placebo every night for 14 days or until discharge. The results demonstrated that melatonin was associated with a lower risk of delirium (12.0% vs. 31.0%, P value = 0.014), with an odds ratio (OR) adjusted for dementia and comorbidities of 0.19 (95% confidence intervals (CI): 0.06 - 0.62). These differences remained statistically significant when the patients with prevalent delirium on admission were excluded. Thus, the nightly administration of low-dose melatonin to elderly patients admitted to the acute care unit could be a potential protective agent for delirium (40). Lammers et al. (2013) described a case, who was an 81-year-old male diagnosed with Alzheimer’s disease 4 years prior to the study and delirium one month before admission. Moreover, haloperidol was not effective for him. Subsequently, 2 mg of melatonin was administrated twice per day and improved his sleep quality, significantly ameliorating his behavior (41). Jonghe et al. (2014) conducted a controlled, randomized, double-blind clinical trial of 378 hip surgery patients aged 65 years or older. The patients received 3 mg of melatonin or placebo in the evenings for 5 days, starting within 24 hours after admission. The results did not show any effects for melatonin on the incidence of delirium between the melatonin (55/ out of 186, 29.6%) and placebo (49 out of 192, 25.5%) groups when a smaller proportion of participants in the melatonin group experienced a long-lasting episode of delirium (> 2 days) (42). Chen et al. (2015) carried out controlled clinical, randomized trials of 669 elderly patients. The data indicated that melatonin supplementation induced a significant 75% decrease in the incidence of delirium in elderly patients, who were presented to medical wards; however, no effect on sleep-wake disturbances was observed (6). Clayton-Chubb et al. (2016) undertook placebo-controlled, double-blind, randomized trials of 36 elderly patients with delirium, who were hospitalized (≥ 70 years old). The patients were divided to 2 groups and received either 5 mg of melatonin or placebo per night for 5 nights or until discharge. The results demonstrated that the administration of melatonin to elderly inpatients with delirium could lead to considerable outcome benefits for delirious inpatients (43).
3.3. Melatonin Agonist, Ramelteon, in Delirium
Ramelteon, a melatonin receptor agonist, has a high affinity for the melatonin receptors (44). Previous case reports indicated that the administration of melatonin agonist, Ramelteon, has some beneficial effects leading to prevention and management of delirium without showing any adverse effects (Table 2).
| Study | Type of Study | Dose of Ramelteon, mg | Other Intervention | Duration of the Study | Conclusion |
|---|---|---|---|---|---|
| Kimura et al. (2011) | Case reports: 3 cases | 8 | - | 7 days | A significant improvement in delirium |
| Furuya et al. (2012) | Case reports: 5cases | 8 | - | During 24 h | Management of delirium |
| Tsuda et al. (2013) | Case reports | 8 | 0.5 mg risperidone | 5 days | Improved delirium without over sedation |
| Ohta et al. (2013) | RCT, N = 28 | 8 | Other drug such as brotizolam, zopiclone, and haloperidol | 7 days | A significant improvement in delirium |
| Hatta et al. (2015) | RCT, N = 67 | 8 | Placebo | 7 days | A lower risk of incidence of delirium with ramelteon (12.0% vs. 31.0%, P value = 0.014) |
Kimura et al. (2011) described 3 case reports that were 3 females admitted to the hospital, who illustrated symptoms of delirium during hospitalization and were administrated 8 mg of Ramelteon per day for the treatment of delirium (45). Furuya et al. (2012) described 5 cases, 3 of which had a primary neurological disease such as Alzheimer’s disease. In addition, one of these 5 cases had no previous psychiatric history, but he did have a medical history of asthma, Hashimoto’s disease. He later had steroid-induced psychosis and illustrated symptoms of delirium during hospitalization. At the end, they were all successfully treated by receiving 8 mg of Ramelteon per day (46). Tsuda et al. (2013) described a case, who was a 100-year-old male with severe pneumonia admitted to the ICU. He had a surgical history and no history of neuropsychiatric problems or dementia. After moving to a general ward from the ICU, he was diagnosed as having delirium. Subsequently, he received a single dose of 0.5 mg of risperidone at 18:00 on the sixth day. He showed over-sedation all day for 2 days and had severe psychomotor excitement after 9 days. The administration of 8 mg of Ramelteon improved delirium without having any adverse effects, such as over-sedation (47). Ohta et al. (2013) performed a study on elderly patients with delirium and insomnia after acute stroke. Seven patients were treated with Ramelteon and 21 patients with the other drugs. The results confirmed that all the patients treated with Ramelteon showed significant improvement within a week (48). Hatta et al. (2015) conducted a multi-center, rater-blinded, randomized, placebo-controlled trial of 67 patients aged between 65 and 89 years old, who were recently admitted for serious medical problems to the ICU. The patients received melatonin agonist, Ramelteon, (8 mg/d; 33 patients) or placebo (34 patients) every night for 7 days. The results confirmed that Ramelteon was associated with a lower risk of incidence of delirium (12.0% vs. 31.0%, P value = 0.014). Therefore, described melatonin neurotransmission could have a possible pathogenic role in delirium (49).
4. Discussion
Despite considerable advances in the understanding of the delirium mechanisms and its effects on critically ill patient outcomes, its prevention and management is still a significant issue. According to the association between delirium and irregular patterns of melatonin secretion, which has been described by several studies, irregular melatonin secretion could be one of the mechanisms of delirium (10, 23, 30, 31, 50-52) as well as the presence of sleep deprivation in hospitalized delirious patients at the ICU, as it has been indicated that melatonin and its agonists could be an effective supplement for prevention and management of delirium (38, 53, 54). Furthermore, several studies have reported the marked improvement of delirium in delirious patients without side effects due to the use of melatonin and ramelteon (6, 45, 46). According to the literature, pharmacological methods are not yet recommended for prevention of delirium in critically ill patients, based on reviewed studies, especially because melatonin could improve patients’ sleep; further trials could be performed to evaluate the efficacy of melatonin on prevention of delirium.
4.1. Conclusion
Exogenous melatonin and melatonin agonist, ramelteon, could improve circadian rhythm, therefore, the use of melatonin supplementation leads to prevention, improvement and control of delirium at the ICU.