1. Background
Chronic obstructive pulmonary disease (COPD) is a major noncommunicable respiratory disease with diverse pulmonary and external pulmonary clinical manifestations (1, 2). This disease is one of the leading causes of mortality in the world (3), and about 1% of the adult population suffers from COPD. Meta-analyses performed in 2015 showed a high and growing prevalence of COPD (4), and it is predicted to become the third cause of death and disability in the world by 2020 (5).
Studies have shown that people with COPD have sustained airway inflammation that causes high mucus secretion, airway stenosis, and an increase in inflammatory markers, such as C-reactive protein (CRP), tumor necrosis factor alpha (TNF-α), interleukin-6 (IL-6), IL-8, etc. (5, 6). The relationship between inflammatory cells and cytokines, and the sequence of events that leads to progressive airway obstruction and destruction of the parenchymal lung, remains largely unknown (7). Since inflammation plays an important role in the development of COPD, measuring the level of inflammatory and proinflammatory factors can be effective in the diagnosis and treatment of this disease, and these factors can be used as special therapeutic goals.
Due to differences in the health care system of the nations, economic policies, and drug availability, there are many differences in the treatment methods of COPD patients (8). Montelukast (a leukotriene receptor antagonist) is one of the medications that is well tolerated in patients with asthma (9). Leukotrienes are the important inflammatory mediators of upper and lower airways (10). It has been observed that in patients with asthma, the early administration of montelukast at the onset of viral respiratory infections reduces the symptoms of asthma (11). In a study conducted on 20 COPD patients who were treated with montelukast pills for 12 months, a significant decrease in serum leukotriene B4 and IL-8 levels was observed (6).
IL-18 is a member of the IL-1 family cytokines. The members of this family are able to regulate inflammation. IL-1β and IL-18 have a common production pathway that is dependent on Caspase-1 and can lead to inflammation and cell death (12).
Previous studies on some of the beneficial and anti-inflammatory effects of montelukast have been conducted on COPD animal models. However, the results are unknown or less applicable in human studies due to the known pathogenesis of COPD and the mechanism of action of montelukast and its effectiveness in asthmatic patients. Also, inflammatory factors are cost-effective and accessible as effective factors in the progression of COPD disease.
2. Objectives
Therefore, we decided to evaluate the effect of montelukast administration on serum levels of common inflammatory factors, such as TNF-α, CRP, and IL-18, in COPD patients.
3. Methods
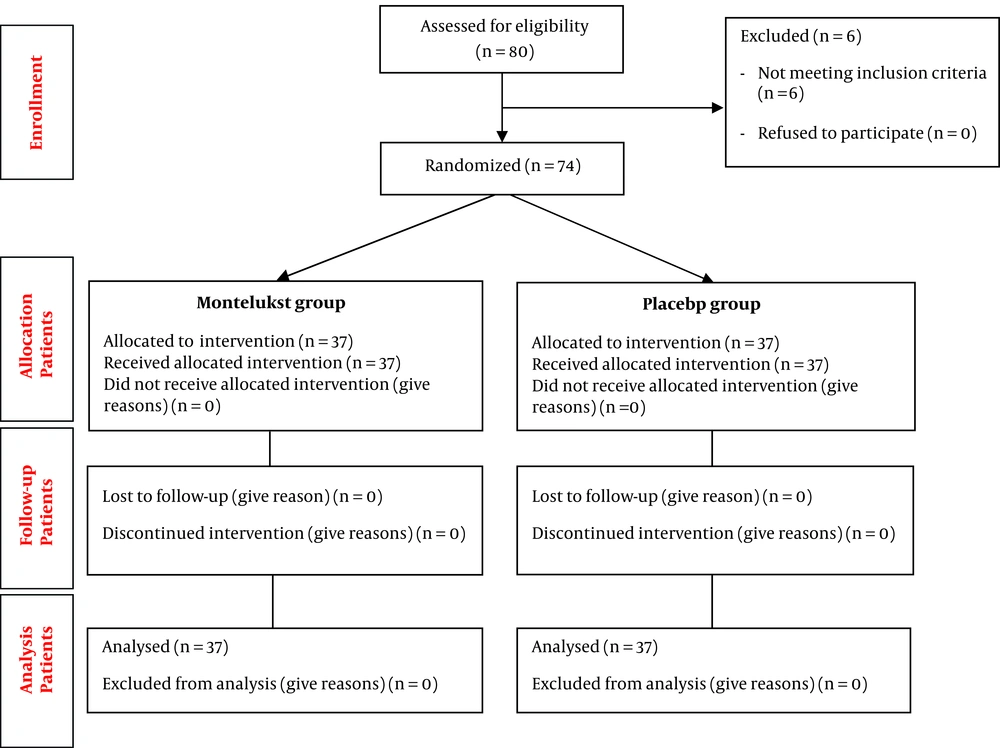
We conducted an interventional study as a double-blind, randomized placebo-controlled clinical trial to evaluate montelukast effects on the serum level of inflammatory factors, including IL-18, TNF-α, and CRP in patients with COPD. Patients were recruited from May 2018 to September 2018 from Shahid Rahimi Hospital in Khorram Abad. The studied subjects were COPD patients aged 40 to 70 years in the II, III, or IV stages of the disease, with stable conditions in the last three months and also had no history of hospitalization, recently corticosteroid use, and inflammatory disease or cardiovascular, rheumatic, pulmonary, and progressive renal diseases. Six out of 80 patients were omitted, as mentioned in the flowchart (Figure 1). Samples were selected using available sampling and assigned to the study groups using the randomized block method. The first and second groups received montelukast (10 mg/d) and placebo for 2 months, respectively. During the study, physicians and patients remained blind, and all patients, regardless of the group, continued their treatment according to the treatment protocol, and concealment of randomization adhered. The patients were closely observed by regular monthly visits and also by making telephone calls for two months.
3.1. Ethical Approval
The research followed the tenets of the Declaration of Helsinki. The Ethics Committee of Lorestan University of Medical Sciences approved this study (LUMS.REC.1396.321). All study protocols were approved by the institutional ethical committee at Lorestan University of Medical Sciences. Accordingly, written informed consent was taken from all participants before any intervention. This trial was registered at the Iranian Registry of Clinical Trials (IRCT20190423043361N1).
3.2. Laboratory Studies
We collected 15 CC of venous whole blood samples from each patient two times, at the beginning and at the end of the study, and the levels of inflammatory factors, such as TNF-α, IL-18, and CRP were measured using Sigma kits. After centrifugation of the samples and measurement of the mentioned parameters, the serum was separated followed by freezing at -20°C for the measurements of IL-18 and TNF- α levels using enzyme-linked immune sorbent assay kits (EASTBIOPHARM; IL-18 and TNF- α ELISA Kits were based on double-antibody sandwich enzyme-linked immunosorbent assay technology) at the beginning and at the end of the study. Also, the CRP level was measured with semi-quantitative CRP latex agglutination kits (Bionik kit was based on direct agglutination on a slide with a black background).
4. Results
Of 76 studied patients, no patient in the montelukast and control groups was excluded from the study due to non-adherence to study protocol or side effects. The montelukast group included 28 (73.7%) men and 10 (26.3%) women. Also, in the placebo group, there were 32 (84.2%) male and 6 (15.8%) female cases. The two groups were homogenous regarding sex (P = 0.399). In mean age of the montelukast and placebo groups was 55.68 ± 8.54 and 54.66 ± 8.99 years, respectively. There was no significant difference between the mean age of the two groups (P = 0.612).
The frequency and percentage of patients according to inflammatory factors (TNF-α, IL-18, and CRP) are listed in Tables 1-3. As shown in Table 1, in the placebo group, the mean of TNF-α increased from 109.01 ± 29.6 in the pre-intervention to 151.69 ± 48.2 in the post-intervention period, which showed a statistically significant difference (P = 0.012). Also, in the group receiving the montelukast, the mean of TNFα increased from 116.09 ± 36.93 before the intervention to 153.19 ± 51.58 after the intervention, which was statistically significant (P < 0.001). Regarding between-group difference (P = 0.95), there was no significant difference in TNF-α changes between both placebo and montelukast groups.
| Group | Before | After | Difference | P Value Within-group | P Value Between-group | |||
|---|---|---|---|---|---|---|---|---|
| Mean ± SDa | Median (IQR) | Mean ± SD | Median (IQR) | Mean ± SD | Median (IQR) | |||
| Placebo | 109.01 ± 29.6 | 106.1 (117.1) | 151.69 ± 48.2 | 133.4 (53.2) | 42.68 ± 53.31 | 27.5 (52.55) | 0.012 | 0.95 |
| Monelukast | 116.09 ± 36.93 | 109.8 (222.7) | 153.19 ± 51.58 | 142.6 (40) | 37.10 ± 30.84 | 34.3 (40.60) | < 0.001 | |
aStandard deviation.
| Group | Before | After | Difference | P Value Within-group | P Value Between-group | |||
|---|---|---|---|---|---|---|---|---|
| Mean ± SD | Median (IQR) | Mean ± SD | Median (IQR) | Mean ± SD | Median (IQR) | |||
| Placebo | 18.97 ± 6.2 | 17.4 (6.2) | 16 ± 4.16 | 14.7 (19.2) | 2.97 ± 6.8 | 2.5 (43.8) | 0.003 | 0.23 |
| Monelukast | 20.25 ± 5.98 | 20 (4.8) | 16.19 ± 4.17 | 15.9 (5.3) | 4.06 ± 4.65 | 3.2 (25.4) | < 0.001 | |
| Group | CRP (Before intervention) | CRP (After intervention) |
|---|---|---|
| Placebo | 3 (7.9%) | 0 |
| Monelukast | 1 (2.6%) | 1 (2.6%) |
As shown in Table 2, the mean IL-18 before the intervention was 18.97 ± 6.2 in the group receiving placebo and significantly decreased after the intervention to 16 ± 4.16 (P = 0.003). Also, the mean IL-18 in the group receiving montelukast before the intervention was 20.25 ± 5.98 and significantly decreased after the intervention to 16.19 ± 4.17 (P < 0.001). Despite a decrease in mean levels of IL-18 after the intervention, because of the decrease in this variable in both placebo and montelukast groups at the end of the study and regarding between-two difference (P = 0.23), this reduction was not statistically significant.
As shown in Table 3, in the placebo group, the number of CRP-positive patients was 3 (7.9%) and 0 before and after the intervention, respectively. Also, in the recipient group of montelukast, one CRP-positive person (2.6%) was found before the intervention, and after the intervention, this number did not change (P > 0.05). These results showed that montelukast has no effect on the CRP level and its reduction in the placebo group was probably due to unknown reasons.
5. Discussion
The results demonstrated that montelukast has different effects on the inflammatory aspects of COPD. The inflammatory process of COPD was evaluated by measuring serum levels of inflammatory markers, such as TNF-α, CRP, and IL-18. At the end of the study, no significant changes were observed in the levels of these markers in both groups.
However, the mechanism of montelukast is to inhibit the interleukin receptor to impair the function of interleukin and inhibit the stimulation of effective cells and the secretion of inflammatory factors. On the other hand, montelukast has been shown to inhibit several pro-inflammatory cytokines in animal models of asthma. Maeba et al. (cited in Basyigit et al.) reported an inhibitory effect of montelukast on the lipopolysaccharide-induced production of IL-1β, IL-6, TNF-α, and MCP-1 from peripheral blood mononuclear cells, while Can et al. (cited in Basyigit et al.) demonstrated a decrease in serum TNF-α levels in pediatric asthmatics after montelukast treatment. TNF-α, as a pro-inflammatory cytokine, can respond to pathologic conditions by many inflammatory cells, such as neutrophils and macrophages (13). It is also elevated in COPD patients and has an important role in the pathogenesis of COPD (14). It has been shown that treatment of COPD is associated with a reduction in TNF- α serum levels. For example, Gueli et al. showed that following a long-term treatment (12 months) with montelukast, TNF-α significantly reduced in patients with stable COPD (6), which is in agreement with the results of Rubinstein et al. (15). Feldman et al. also showed the effect of montelukast on the reduction of the serum level of TNF-α in patients with asthma (16). Lishchuk et al. in 2012 showed that in patients with Churg-Strauss syndrome, after three months of treatment with montelukast, the serum TNF-α level decreased significantly, and the patient's pulmonary symptoms improved (17). However, in our study, despite a significant decrease in this cytokine in the montelukast group (within-group P < 0.001), a comparison of a reduction in both groups after intervention showed that this decrease was not significant (between-group P = 0.95). Although the exact cause of this difference is not clear, the length of the treatment period may not be sufficient to show the maximum effects of the drug. For example, in the retrospective study by Rubinstein et al., the long-term (at least 12 months) montelukast therapy (10 mg every night) was safe and associated with significant improvement in COPD management in elderly patients with moderate to severe COPD (15). Also, due to the presence of different phenotypes and subtypes of the disease, there may be differences in the selected populations in various studies.
IL-18 belongs to the immunoglobulin superfamily and is produced by mononuclear cells (18). This cytokine is involved in the onset and development of COPD, and its level is directly related to the severity of the acute exacerbation of COPD (AECOPD) (19). Imaoka et al. showed that serum levels of IL-18 in COPD patients and smokers were significantly higher than nonsmokers (20). Also, it can trigger neutrophil activation (21). In the study on the effect of montelukast on the expression of IL-18 in hypoxic-ischemic brain damage (HIBD), no significant change was observed using the immunohistochemical staining method. IL-18 expression in the treatment group was lower than the control group, but it was not statistically significant (22). Meng et al. Showed that the use of tiotropium bromide in combination with montelukast had several effects on the treatment of COPD, including a reduction in IL-18 levels (23). In our study, montelukast prescription reduced the level of IL-18 in the montelukast group. However, a non-significant reduction was observed in the placebo group. The anti-inflammatory mechanism of montaukast has been shown to be the inhibitory effect of the most important inflammatory pathways, nuclear factor-kappa B (NF-кB), and downstream pro-inflammatory factors, such as TNF-α and IL-1β (24). Due to the role of montelukast in reducing IL-1β levels in previous studies (25), and the role of inflammasome and caspase-1 in the production of these two cytokines (IL-1β and IL-18) (26), montelukast probably uses a similar mechanism to reduce the level of IL-18. This may explain the partial inhibitory effect of montelukast on the development of smoke-induced inflammation by reducing some inflammatory cytokines, such as IL-18.
In a study to assess the effect of montelukast on the progression of atherosclerosis in affected local domestic rabbits, it was shown that montelukast reduces systemic inflammation and aortic expression of inflammatory markers by measuring TNF-α and hs-CRP levels (27). In the study on the montelukast effect on inflammatory factors (such as TNF- α, hs-CRP, and some inflammatory cytokines) and lung function of children with cough variant asthma, it was observed that montelukast can significantly reduce inflammatory responses (28). In our study, we did not see a decrease in the number of CRP-positive patients in the montelukast group, despite the reduction in CRP in all CRP-positive patients in the placebo group. This difference can be due to the different used methodology in the measurement or other uncertain factors involved in the occurrence of inflammation.