1. Introduction
Sarcoidosis is an inflammatory granulomatous disorder typically affecting young adults, and it is pathologically characterized by presence of non-caseating granulomas in affected tissues, including lungs and lymph nodes (1). Although the precise etiology of sarcoidosis is unknown, the immune system, infectious, and non-infectious agents may contribute to its pathogenesis. It has been suggested that specific human leukocyte antigen (HLA) alleles may increase risk of sarcoidosis (2). There are few reports on association of sarcoidosis and other disorders that may similarly have an immunological basis, including ulcerative colitis (UC).
Ulcerative colitis is a chronic form of inflammatory bowel disease (IBD) that involves mainly the mucosal layer of colon. Although there have been few reported cases of sarcoidosis in association with UC (3), these disorders are not commonly coexisted. Some cases occur following treatment with anti-TNF agents, but there is no clear evidence on this association.
Herein, we report a case of UC, without a prior history of treatment with infliximab, whose disease was in remission for about 20 years, before developing sarcoidosis. Human leukocyte antigen typing of the patient was examined by polymerase chain reaction using sequence-specific primers (PCR-SSP).
2. Case Presentation
The patient was a 48-year-old woman, known case of UC for a period of 20 years, with symptoms of abdominal pain and bloody diarrhea that repeated several times daily. The patient was a teacher with no smoking habit. Her last disease flare was 10 years ago. She had been cured by mesalazine with primary dose of 3 g/day, which was reduced to 1 g/day. After changing the dosage, the patient had no complaints, and the symptoms were controlled. She was on regular follow-up by gastroenterologist, and her UC was in remission. No evidence of colitis was observed in her last colonoscopy done two years ago. She presented to the Adult Pulmonology Clinic with complaints of chronic non-productive cough, episodic night sweats, progressive dyspnea (initially on exertion, then at rest), fatigue, and significant weight loss. Her clinical manifestations began since about 1 year ago and aggravated over time. Regarding her respiratory problem, the symptoms were under control, and she did not suffer from dyspnea and cough anymore. She started taking hydroxychloroquine 200 mg/day and prednisolone 5 mg/day.
At the first visit, the patient’s physical examination showed stable hemodynamics, normal breath sounds, and cardiac auscultation. Also, no significant finding was noted in her abdominal examination. She underwent some laboratory assessments (Table 1) and total colonoscopy, which showed no significant abnormality.
| Variables | Values |
|---|---|
| Hematology | |
| WBC (× 103/μL) | 5.4 |
| RBC (× 103/μL) | 5.15 |
| Hb (g/dL) | 12.2 |
| Hct (%) | 38.2 |
| MCV (fL) | 74.2 |
| MCH (pg) | 23.9 |
| MCHC (g/dL) | 32.2 |
| Platelet (× 103/μL) | 340 |
| RDW-CV (%) | 13.9 |
| Biochemistry | |
| AST (IU) | 16 |
| ALT | 7 |
| ALP (IU) | 198 |
| BUN (mg/dL) | 16.9 |
| Cr (mg/dL) | 1.1 |
| Serology | |
| ESR (mm/h) | 10 |
| CRP | Neg. |
| RF | Neg. |
| Human leukocyte antigen typing by polymerase chain reaction | |
| A* | 01-03 |
| B* | 35-57 |
| C* | 04-06 |
| DRB1* | 07-13 |
| DRB3,4,5 | 3,4 |
| DQ* | 03-06 |
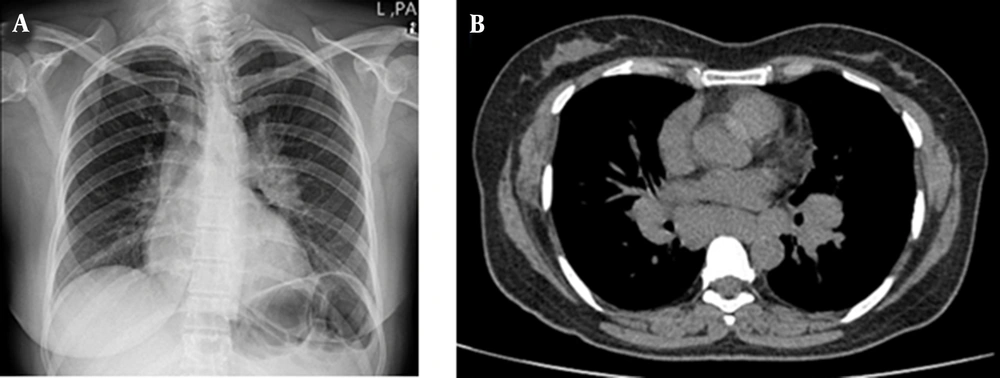
Due to shortness of breath, plain chest radiography was obtained that was suggestive of bilateral hilar lymphadenopathy (LAP) (Figure 1A). Next, contrast-enhanced computed tomography (CT) of the lungs and mediastinum was obtained, that confirmed the aforementioned finding (Figure 1B). Transthoracic echocardiography also showed no significant abnormality.
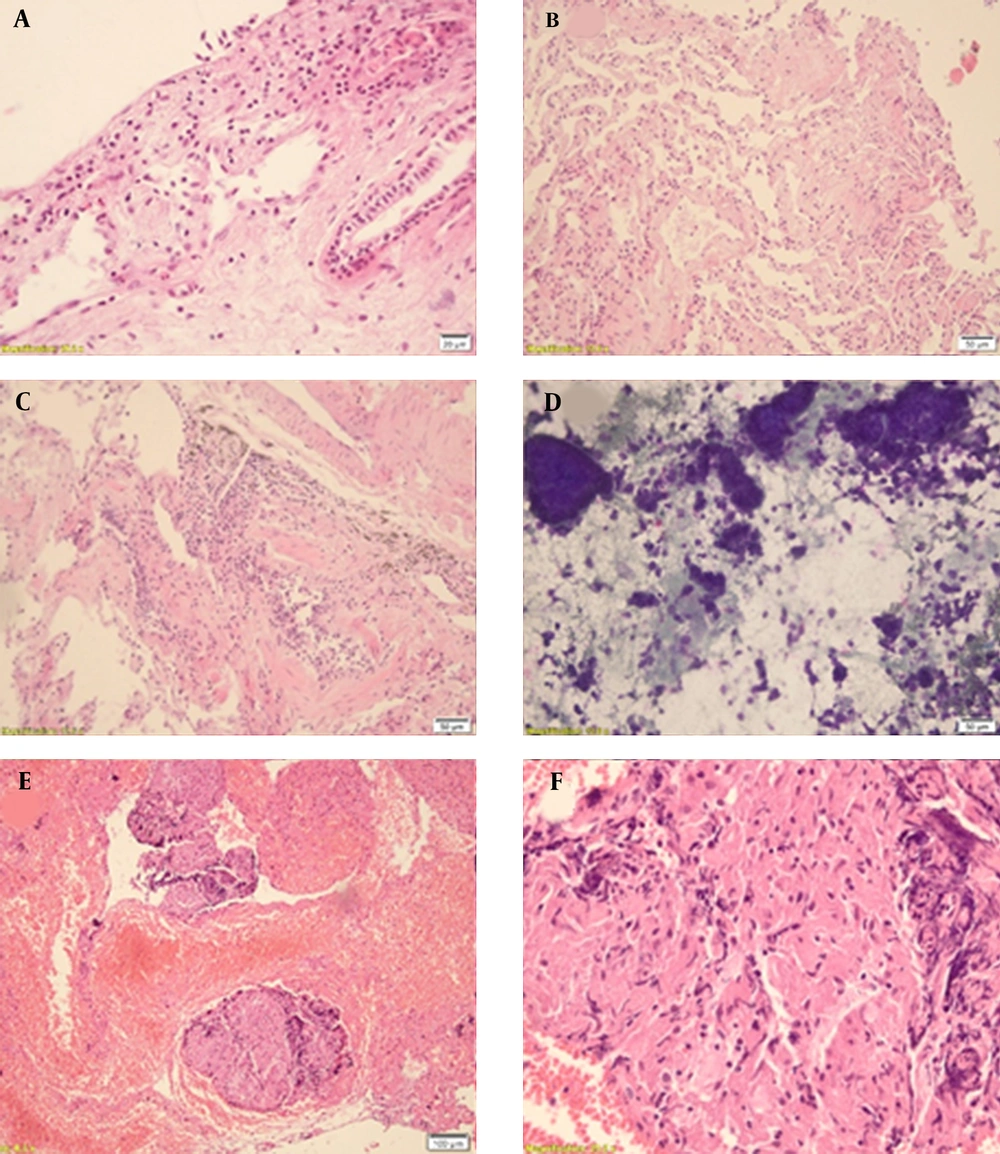
The patient underwent fibrobronchoscopy, bronchoalveolar lavage (BAL), and transbronchial lung biopsy (TBLB) to evaluate the underlying cause of LAP. Our investigations (laboratory and histopathology) showed no evidence of malignancy. However, microscopic review of hilar lymph node tissues revealed non-caseating granulomas representative of sarcoidosis (Figure 2). It is worthy to mention that this patient was on mesalazine (with a total daily dose of 1000 mg) and had no history of anti-TNF (including infliximab) administration.
A, Microscopic slides of transbrochial lung biopsy exhibit bronchial tissue lined by bland-looking columnar surface epithelium, and edematous inflamed stroma; B, Lung parenchyma shows intact alveoli lined by flat epithelium, interstitial fibrosis, and thick fibrous bands in alveolar septae; C, Along with mixed lymphocytic-rich inflammation and antrachotic macrophages; D, Cytology smears of BAL fluid show many lymphocytes, collections of dust macrophages and many degenerated to reactive respiratory-type epithelial cells in a bloody background; E, Peribronchial lymph node biopsy reveals multiple discrete non-caseating granulomas; and F, Composed of epithelioid histiocytes with abundant amount of eosinophilic cytoplasm, rimmed by lymphocytes with crushing artifact evident in higher magnification
3. Discussion
Sarcoidosis is a condition that may coexist with both forms of IBD, UC, and Crohn’s disease (CD), and vice versa; patients with sarcoidosis may complicate with gastrointestinal involvement (4, 5). It has been estimated that prevalence of gastrointestinal involvement in sarcoidosis is about 0.1% - 0.9%, and the stomach (mainly antrum) is the most affected part. Nevertheless, gastrointestinal involvement may be asymptomatic (6).
Inflammatory bowel disease, including UC and CD, can cause extra-intestinal involvement and may affect the lungs causing different forms of pulmonary abnormalities concomitantly (5). Although they may be clinically asymptomatic, it has been estimated that pulmonary function test (PFT) or chest imaging of about 37% - 55% of cases with IBD reveal abnormalities. The value of PFT abnormalities reaches about 90% in patients with active phase of gastrointestinal disease (7). Cases with IBD may suffer from various forms of lung involvement, including tracheal stenosis, bronchitis, bronchiectasis, alveolitis, pulmonary fibrosis, pleural diseases, etc. (4, 5, 7, 8). A decreased forced expiratory volume in first second (FEV1) and diffusion capacity of the lungs for carbon monoxide (DLCO) are among the most common PFT abnormalities associated with IBD. Additionally, medications used for the treatment of IBD, like methotrexate, may cause lung injury (7).
Although some cases with coexistence of sarcoidosis and IBD have been reported (Table 2), no clear evidence has been identified to precisely explain the association between these two diseases so far (9-11). It has been suggested that this coexistence may be related to common genetic and immunological mechanisms, and both diseases may have common allelic regions implicated in their pathogenesis (5, 6). Several studies focused on genes involved in the regulation of the immune responses, in particular the major histocompatibility complex (called HLA in humans). HLA-DRB1, HLA-DQA1, and HLA-B loci have shown the strongest and broadest associations with IBD (12). However, no distinct allele is implicated as the primary disease susceptibility gene in UC. The most consistent associated alleles with UC are the positively associated HLA-DRB1*1502 (subtype of HLA-DR15) and HLA-DRB1*0103, and negatively associated DRB1*0401 alleles (12, 13). HLA-DRB1*12 and HLA-B*52 may also contribute to the development of UC (13, 14).
| References | Year | Age (y)/Sex | Order and Interval of Onset (y) | Human Leukocyte Antigen | Preceding Treatment |
|---|---|---|---|---|---|
| (3) | 1967 | 30/M | UC - SAR (2) | N.C. | Steroid |
| 1969 | 26/M | UC - SAR (2) | N.C. | Steroid, salazopyrin | |
| 1971 | 52/F | SAR - UC (13) | N.C. | - | |
| 1981 | 64/F | Coincidence | N.C. | - | |
| 1986 | 44/F | UC - SAR (20) | Three patients with HLA A1, B8, and DR3+ | Steroid | |
| 31/M | Coincidence | - | |||
| 64/M | SAR - UC (12) | Steroid | |||
| 38/F | SAR - UC (6) | - | |||
| 33/M | SAR - UC (15) | Steroid | |||
| 20/M | UC - SAR (16) | - | |||
| 37/F | SAR - UC (9) | - | |||
| 47/M | UC - SAR (13) | - | |||
| 1987 | 30/M | UC - SAR (13) | B8 | Steroid, sulfasalazine | |
| 1989 | 42/M | UC - SAR (13) | N.C. | - | |
| 1995 | 38/M | UC - SAR (13) | N.C. | Steroid, sulfasalazine | |
| 1996 | 41/M | UC - SAR (6) | N.C. | Tixocortal | |
| 1996 | 58/F | UC - SAR (36) | N.C. | Steroid | |
| 1997 | 22/M | UC - SAR (6) | A27, B52, B54, DR2, DR4 | - | |
| 1999 | 33/F | Coincidence | DR52 | - | |
| 2001 | 38/F | UC - SAR (10) | A2, A28, B27, B44 | Steroid, sulfasalazine | |
| 2003 | 53/M | UC - SAR (3) | N.C. | Steroid, mesalamine | |
| 2005 | 33/F | UC - SAR (10) | N.C. | Steroid | |
| 2013 | 50/M | UC - SAR (8) | N.C. | Steroid, salazopyrin | |
| 2015 | 62/F | UC - SAR (24) | A24, A26, B62, B52, DR14, DR15 | Mesalazine | |
| (24) | 2017 | 30/M | UC - SAR (5) | A24, B62, DR14- A26, B52, DR15 | Infleximab, 5-ASA, azathioprine, steroid |
| Our study | 2022 | 48/F | UC - SAR (20) | A*01, DRB1*13-DQB1*06 haplotype | Mesalazine |
Abbreviation: N.C., not considered.
Likewise, familial clustering of sarcoidosis has been reported previously. Various genes have been suggested to contribute to genetic susceptibility to sarcoidosis, including genes encoding angiotensin converting enzyme, vitamin D receptor, T-cell receptor genes, immunoglobulin genes, and, most relevant, HLA genes (15). It is claimed that HLAs DRB1*08, DRB1*11, DRB1*12, DRB1*14, DR 15 (serotype of HLA DRB1*15), and DR 17 (equivalent to HLA DRB1*03) cause susceptibility to developing sarcoidosis; however, some others, including HLAs DR1 (HLA DRB1*01), DR4 (HLA DRB1*04), and possibly DQ*0202 may play a protective role (9, 16).
Barr et al. showed that HLA A1, B8, and DR3 phenotype occur with a higher frequency in cases with sarcoidosis associated with UC than the patients with either disease alone (17). The present case had HLA-A*01 allele, which may be related to the occurrence of sarcoidosis in association with UC.
DRB1*13-DQB1*06 haplotype is one of the most prominent positive HLA associations of primary sclerosing cholangitis (PSC). The present case, though not complicated by PSC, had the DRB1*13-DQB1*06 haplotype. The frequency of the DRB1*13-DQB1*06 haplotype is about 3.3-7.7% in different Iranian ethnic populations (18). This suggests that this haplotype may play a role in different autoimmune disorders, including sarcoidosis.
Some cases have been shown to harbor both sarcoidosis-related HLA alleles and UC-related alleles (3). However, patients suffering from both diseases without any of the known susceptible HLA genotypes have also been reported (3). These cases, along with our reported case suggest that there might be unknown common susceptible genes outside the MHC class I and II region influencing the onset of both sarcoidosis and UC. Some non-classical HLA genes involved in antigen processing and presentation, namely TAP, LMP, and DM, and alleles of the tumor necrosis factor gene cluster (TNFA, LTA, LTB), seem to contribute (15). The association of IL23R with sarcoidosis has also been identified, and based on genetic results, possible aetiologic similarities between sarcoidosis and IBD were reported (19). Further studies are required to better understand the genetic associations between sarcoidosis and UC. It has also been reported that patients with UC treated with infliximab are susceptible to develop sarcoidosis (20-24).
3.1. Conclusions
Herein, we reported a case that developed sarcoidosis 20 years after the onset of UC symptoms without a prior history of infliximab therapy. Patients with UC who possess HLA-A*01 phenotype may possibly be more susceptible to developing sarcoidosis.