1. Background
The electronic health record (EHR) is a new technology, which is considered as a standard for medical practice in the United States in the 21st century. In the past 15 years, the results of numerous studies have emphasized on the need to move towards EHR and promote information structure-based technologies (1, 2). From the perspective of the world health organization (WHO), an EHR contains all the information about a person’s health, provides electronic access for providers during life, and consists of all the patient’s referrals and received services, including outpatient, inpatient, and emergency services. EHR includes information, such as observations and visits, results of laboratory tests, reports of diagnostic imaging, allergies, received treatments and prescribed drugs, identification information, and legal permissions (3, 4).
To date, great efforts have been made to increase the quality, safety, and efficiency of health services using information technologies, including EHR, computerized physician order entry (CPOE), and decision support systems (DSSs) (5). In many countries, use of computerized information to reduce paper records has become one of the Ministry of Health projects, with advantages such as medical information exchange, standardized medical terms, increased security and privacy, and standardized treatment processes (6).
The advantages of EHR are inadequate for motivating physicians to use them, and there are various reasons for physicians’ resistance, including failure of advertisements, negligence of its capacities, physicians’ limited computer knowledge, and fear of low efficiency, patient dissatisfaction, and unreliable technologies (7). Some of the main advantages of EHRs include increased knowledge about medical errors and attempts to decrease them, increased focus on patients’ recovery, and improved quality of patient care (8). Although there has been significant progress in EHR around the world, it has not been fully implemented around the world during the past 3 decades, and it does not have the required effectiveness yet (9).
Electronic health (E-Health) in Iran was established in medical diagnostic laboratories in 1981. In the 1990’s, activities of the private sectors in the field of medical software started, and public and governmental activities in this area were developed. In the 2000’s, applied information technologies (abbreviated as “TAKFA” in Persian) and health information technologies (abbreviated as “TAKFAB” in Persian) were developed, and strict details and characteristics of E-Health development were determined. Also, health level 7 version 3 (HL7 v.3.0) was considered as the interactive standard. In 2007, the review of 80 types of software in the field of health was initiated, and the electronic health record architecture started to develop, which is now being set up as a national project, known as Iran’s EHR system project (abbreviated as “SEPAS” in Persian). In addition, some local projects, such as health cards and patient record software, are being implemented by different organizations and companies, which should become affiliated to SEPAS in near future (10).
Several studies have been conducted on EHRs in Iran and other countries, including studies performed by Gorzin et al. (2016) on the opportunities and challenges of EHR documentation from the nurses’ perspective (11) and Ahmadi et al. (2015) on the development of a conceptual model for the radiology reporting system (12). Moreover, Asadi et al. (2015) have evaluated Iran’s SEPAS national project based on EHR system coordinates (13), Ghazisaeidi et al. (2014) have assessed readiness for preimplementation of EHR in Iran (14), and Jebraeily et al. (2012) have examined the barriers to EHR implementation in Iran (15).
Furthermore, Palojoki et al. (2016) (16) studied the concerns about EHR-related safety, Jensen and Bossen (2016) evaluated factors affecting physicians’ use of a dedicated overview interface in EHR (17), and Jalota et al. (2015) examined interventions to increase physicians’ efficiency and comfort with an EHR system (18). Risko et al. (2014) also studied the impacts of implementing EHRs on the emergency physicians’ efficiency and patient throughput (19), while Morton (2008) evaluated the factors affecting physicians’ attitudes towards the use and acceptance of EHR, which showed that behavioral and social factors influencing HER planning should be considered (20).
There is little evidence reviewing physicians’ attitudes towards EHRs, and there is a need for conducting further studies. Since one of the key strategies of the healthcare system in Iran is the implementation of EHRs at the national level, this study aimed to investigate the physicians’ attitudes towards the implementation of EHRs in a university-affiliated teaching hospital in Tehran, Iran.
2. Methods
This cross sectional study was conducted in a university-affiliated teaching hospital in Tehran, Iran in the second half of 2016. This hospital was founded in 1875 and has 373 available beds and 169 physicians. In the present study, the attitudes of all 169 physicians working in this hospital towards the implementation of EHR were investigated, using the census sampling method.
The required data were collected using the translated and localized Morton’s standard questionnaire (2008) (20), which consisted of 42 items in 8 dimensions of “management support” (6 items), “physicians’ participation” (5 items), “physicians’ independence” (7 items), “physician-patient relationship” (4 items), “education and training” (5 items), “perceived ease of use” (4 items), “perceived usefulness” (5 items), and “physicians’ attitudes towards HER” (6 items); the physicians’ demographic characteristics were also included. A 5-point Likert scale was used to investigate the physicians’ attitudes towards the implementation of EHRs (1, “strongly disagree” to 5, “strongly agree”).
The international quality of life assessment (IQOLA) was used for the translation, cultural adaptation, and localization of the questionnaire (21). The content validity of the questionnaire was approved through content validity index (CVI) and content validity ratio (CVR). Its construct validity was also confirmed using structural equation modeling (SEM), in which all fitting indices showed acceptable values. The reliability of the questionnaire was also approved (α, 0.78). A 5-point Likert scale was used to investigate the physicians’ attitudes towards the implementation of EHRs (1, “completely disagree” to 5, “completely agree”).
At the beginning of the study, one of the researchers, who was responsible for data collection, visited the studied hospital, made the required coordination with the hospital administrator and directors of different wards, and arranged a short briefing meeting about the study and its objectives. Then, the physicians’ viewpoints were assessed by distributing the questionnaires. The data collection process continued for 2 months, and the questionnaires were distributed and gathered simultaneously by the researchers.
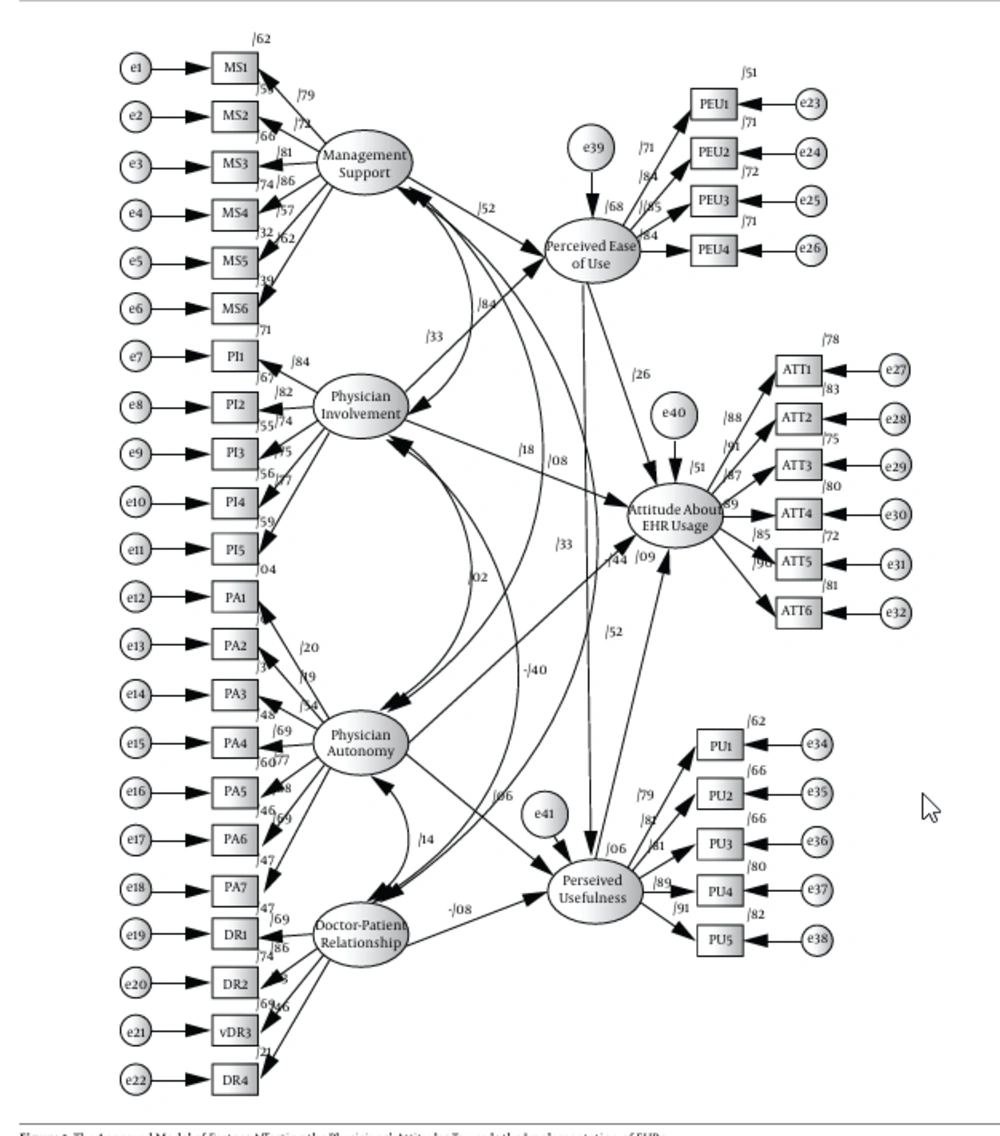
As mentioned above, SEM was used in the present study to analyze the relationships and associations among variables and factors in the conceptual model. SEM is a technique in which interdependent and simultaneous relationships among several variables and factors are studied and tested. In the current study, two main components of SEM were used, including measurement and structural models.
The measurement model determines the contribution of each item to measuring the latent variables using confirmatory factor analysis, while the structural model determines the relationships between the latent variables. The measurement model shows the relationships between the latent variables and their indicators, while the structural model shows multiple relationships among the variables. It should be noted that the conceptual model used in the current study was the Morton’s model, which includes 8 dimensions, as mentioned above.
In the present study, the following fundamental principles were taken into account as the ethical considerations: coordinating with the hospital administrator and directors of the studied wards through an introduction letter, providing the required explanations about the study objectives for the physicians, voluntary participation in the study (the participations could withdraw from the study at any stage), anonymous responses to the questionnaire items, and confidential data analysis.
The collected data were analyzed using IBM SPSS version 23.0 and AMOS version 18.0. P value less than 0.05 was considered statistically significant.
3. Results
The results showed that most of the studied physicians were male (52.1%), less than 30 years (38.5%), married (60.9%), and residents (35.7%). The majority had less than 5 years of work experience (56.8%) (Table 1).
| Variables | No. (%) | |
|---|---|---|
| Gender | Male | 88 (52.1) |
| Female | 81 (47.9) | |
| Age, y | < 30 | 65 (38.5) |
| 30 - 40 | 42 (24.9) | |
| 41 - 50 | 36 (21.3) | |
| > 50 | 26 (15.4) | |
| Marital status | Single | 66 (39.1) |
| Married | 103 (60.9) | |
| Education level | Resident | 62 (35.7) |
| General practitioner | 7 (5.1) | |
| Specialist | 58 (32.8) | |
| Subspecialist | 42 (26.4) | |
| Work experience, y | < 5 | 96 (56.8) |
| 5 - 10 | 31 (18.3) | |
| 11 - 15 | 26 (15.4) | |
| > 15 | 16 (9.5) | |
| Total | 169 (100) |
The results showed that the conceptual model had a good fit and was structurally acceptable (Table 2). Moreover, the results showed that independent variables could predict 51% of variance in the dependent variable of “physicians’ attitudes towards EHR”. In addition, the results of SEM showed that variables of “perceived usefulness” (r, 0.52) and “perceived ease of use” (r, 0.26) had important effects on the physicians’ positive attitudes (P < 0.001). Also, “perceived ease of use” (r, 0.33) had a significant effect on “perceived usefulness” (P < 0.001). It should be noted that the variable of “education and training” was removed from the final conceptual model because of its low standard coefficient and insignificant effect on the physicians’ attitudes. The final conceptual model and the associations among the variables are shown in Figure 1.
| Fitting Indices | Acceptable Values | Results |
|---|---|---|
| χ2 | - | 1791.950 |
| Degree of freedom (df) | - | 614 |
| χ2/df | 3 > x > 1 | 2.91 |
| P Value | < 0.05 | < 0.001 |
| Root mean squared error of approximation (RMSEA) | < 0.08 | 0.073 |
| Incremental fit index (IFI) | > 0.90 | 0.961 |
| Comparative fit index (CFI) | > 0.90 | 0.959 |
4. Discussion
The most important barriers to the implementation of EHRs are people’s attitudinal-behavioral limitations and organizational changes. If system users are familiarized with the features, objectives, benefits, and positive impacts of EHRs (besides data privacy and security standards), and the ability to exchange messages is developed, their resistance to change will reduce and their readiness for EHR implementation will increase. Before implementing EHRs, it is necessary to assess organizational readiness. In fact, lack of organizational readiness can lead to the organization’s inability to successfully implement EHRs (22-25).
Reasons for the low success of EHR implementation in developing countries include limited resources, lack of information technology support, and lack of stakeholders’ awareness. Increasing users’ readiness through developing their awareness and creating positive attitudes can result in reduced disruption during and after EHR implementation (26).
The results of the present study showed that independent variables of “perceived usefulness” and “perceived ease of use” could predict 51% of variance in the dependent variable of “physicians’ attitudes towards EHR”, which was at a moderate level. The results of a study by Morton and Wiedenbeck (2010) (5) on factors of management support, physicians’ involvement, physicians’ independence, adequate training, patient-physician relationship, ease of use, and usefulness showed that the mean score of each factor was about 3, which is consistent with the results of the present study.
In addition, the results of the current study showed that the studied physicians had relatively favorable views about the management and organizational support of the involved organizations. Organizational support is related to the managers’ ability to provide adequate time and resources for implementing and training EHR systems (27). The results of studies by Morton (2008) (20) and Mirabootaleb et al. (2012) confirm the current findings (28).
Furthermore, the present results showed that management support had a positive significant effect on “perceived ease of use” of EHRs, which is similar to the findings reported by Aldosari (2003) (29) and Dansky et al. (1999) (30). In general, management support had the greatest direct effect on “perceived ease of use”. The physicians’ attitudes indicated their expectation of managers to ensure a suitable workplace, provide good training and support, and resolve technical problems when necessary (20).
Users’ involvement in the selection and implementation of a system can speed up and improve the development of users’ acquisition and adoption (31, 32). Involving physicians in the implementation of EHRs can play a major role in the selection of a user-friendly system. In addition, physicians’ participation in education and understanding the clinical processes are very important (33, 34).
In the present study, “physicians’ independence” had a significant positive effect on the “perceived usefulness” of EHRs. Berner et al. (2005) (9) in their study showed that physicians believe that use of decision support systems and systems of prescribing medications can oppose their authority and independence. The results of previous studies have shown that many scientific advances, which have decreased the physicians’ independence, have increased their resistance and opposition (9, 20, 28).
Aldosari (2003) also found a strong negative association between physicians’ independence and their attitudes towards EHR systems. Moreover, they found the significant association of physicians’ independence with perceived ease of use and perceived usefulness (29). Considering the overall mean of patient-physician relationship, it can be concluded that physicians had moderate attitudes and somewhat disagreed with EHRs. Overall, use of this system did not have any negative effects on the physician-patient relationship.
Electronic physician-patient communication can reduce the costs of health plans implemented in physicians’ offices, as well as laboratory services. Overall, 90% of providers and consumers in the United States are satisfied with such communication. However, some complex issues, such as information confidentiality and security, prevent the widespread use of electronic communication between patients and physicians (35).
The users’ “perceived ease of use” of a system can affect their attitudes (36). According to the results of the present study, “perceived ease of use” had a significant positive effect on “perceived usefulness” of EHRs. In addition, “perceived ease of use” had a significant positive effect on the “physicians’ attitudes towards EHR”. In the Morton’s study, the mean score of “perceived ease of use” was 3.65, indicating the relatively positive attitudes of physicians towards the dependent variable.
The poor direct association between “perceived ease of use” and “physicians’ attitudes towards EHR” in the present study was inconsistent with the theory of technology acceptance model (TAM). The mediating effects of “perceived ease of use” of a system cannot be ignored. However, it was the strongest predictor of usefulness in the TAM model (20). Although this association was part of the main study model, other findings, including those reported by Aldosari, showed that this association was poor (29). Chau and Hu (2002) also concluded that the physicians’ skill in the use of new equipments and technical systems was very high and that they were able to understand new things quickly (36).
Moreover, the results of the current study showed that “perceived ease of use” had a significant positive effect on the “physicians’ attitudes towards EHR”. The results of studies by Morton (2008) (37) and Mirabootaleb et al. (2013) (28) confirm the present findings. Moreover, Moody and Donna (2004) (37) found that the majority of physicians were completely satisfied with the EHR system (38).
It can be concluded that the studied physicians had positive attitudes towards EHRs, which is an advantage for implementing an EHR system in the studied hospital. The comparison of the results of the present study and similar research indicated that almost all the barriers in the present study had been also considered in other studies, although the priorities in these studies were somewhat different, which can be due to differences in the attitudes, care delivery mechanisms, and infrastructures of countries where these studies were conducted.
4.1. Conclusions
In conclusion, the results of the current study showed that physicians working in the studied hospital agreed with the implementation of EHRs; in fact, they had the required abilities and readiness to implement EHRs. According to the results, development of standards related to information security and privacy, as well as standards for conveying messages, especially for physicians and users who work directly with the system, can help improve system performance and increase the quality of provided services. In addition, conducting further studies on the barriers to EHR implementation, improvement of related software, and training physicians to use such programs is recommended.