1. Background
Preterm delivery is defined as delivery between the 20th and 37th week of pregnancy that affects 7% to 11% of all pregnancies and continues to be the primary cause of perinatal mortality and morbidity worldwide (1-3). Preterm birth is associated with a high prevalence of severe neurologic deficits and developmental disabilities and is a leading cause of infant and neonatal mortality, respiratory distress syndrome, sepsis, intraventricular hemorrhage, necrotizing enterocolitis, and disorders related to low gestational age at birth (4). The first step to prevent preterm labor (PTL) is early identification of women at risk (5).
A number of effective interventions are available to provide population-based screening for preterm birth (3). Epidemiologic data and digital examination have not been proved to be helpful in identifying risk factors for preterm delivery (1, 6). Measuring cervical length (CL) with ultrasonography has become increasingly acceptable as an early diagnostic procedure in patients at risk for preterm delivery (6), with transvaginal ultrasonography (TVUS) being considered as the gold standard for the CL assessment (6, 7).
Transperineal ultrasonography (TPUS) is superior and alternative method to TVUS because there is no need for inserting the probe into the vagina; moreover, due to its easy application, it is more accessible and acceptable techniques in pregnant women (7, 8). Additionally, TPUS correlates well with TVUS (7). Although some studies have validated the predictive value of CL measurement by TPUS in assessing preterm delivery (9), there is still controversy over the feasibility and reliability of TPUS versus TVUS (10).
2. Objectives
The aim of this study was to investigate the feasibility and reliability of CL measurement by TPUS in the second trimester of pregnancy in comparison with those by TVUS.
3. Patients and Methods
3.1. Study Population
The study was conducted from September 2009 to March 2010 at Hafez and Zeinabieh hospitals, affiliated to Shiraz University of Medical Sciences. The Institutional Review Board (IRB) and the Ethics Committee of Shiraz University of Medical Sciences approved the study protocol.
Women with singleton pregnancy who had an accurate dating by last menstrual period (LMP), confirmed by first trimester sonography, were included in this study. Women with a history of dilatation and curettage, cervical anomalies, early delivery, cervical cerclage, and early termination due to medical or obstetrical indications were excluded from the study. Data regarding age, parity, number of previous abortion, and history of PTL or delivery were obtained through face-to-face interview. A total number of 195 eligible women with gestational age of 18 to 24 weeks gave their written informed consent for CL assessment by TVUS.
3.2. Study Protocol
Labor residents selected all the patients at the time of admission. A thorough history was taken from the participants and a resident performed a complete physical examined including digital vaginal examination. The data including the fetal presentation, cervical dilatation, effacement, and past medical history were recorded in a questionnaire. The patients were registered in the hospital and a unit number was assigned to them.
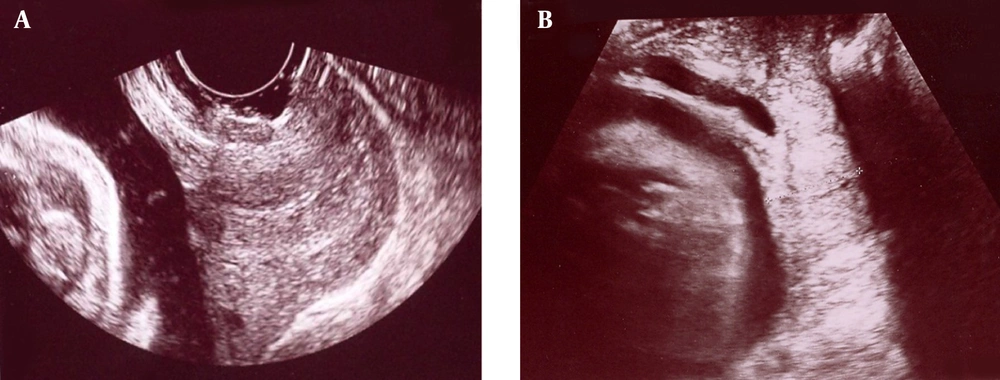
CL measurements by TVUS were performed with a 5 to 7 MHz endovaginal transducer and Voluson 730 ultrasound machine (General Electric’s Inc., Austria) by a single perinatologist (the first author). Women were placed in lithotomy position with empty bladder. Cervical pressure was avoided during transvaginal measurement. The CL was measured on sagittal plane with clear image of the internal and external os and the obvious view of the cervical canal (Figure 1 A). The same machine was used for measuring CL thorough perineum. The ultrasonographic probe was rotated until a clear image of the cervical canal as well as internal and external os were obtained (Figure 1 B); the patients were followed until delivery and the gestational age was recorded.
An analysis was done throughout the study to assess the correlation between CL size and chance of preterm birth. All the patients and their obstetricians were provided with the risk assessment results of the TVUS and TPUS and were asked to reduce the risk of preterm delivery according to the standard guidelines.
3.3. Statistical Analysis
All the data were processed using MedCalc version 11 (MedCalc Software, Mariakerke, Belgium). Regression analysis was used to determine the significance of the association between obtained CLs by TVUS or TPUS. The Bland-Altman plot representing the difference between obtained measurements from TVUS or TPUS and the mean of paired measurements was prepared and the 95% confidence interval (CI) for paired observations was calculated. Receiver operator characteristic (ROC) curves were prepared, enabling the selection of an optimal cutoff point that would minimize both the false-positive and false-negative rates. The developed method by Hanley and McNeil was used to determine whether there was any significant difference between the ROC curves of TVUS and TPUS. Specificity and sensitivity for the tests were also calculated.
4. Results
Preterm delivery after 20 weeks and before 37 weeks of gestation occurred in 16 patients (8.2%) and 179 patients (91.8%) had term delivery at ≥ 37 weeks of gestation. Mean of mothers’ age was 26.6 ± 3.9 years in term and 27.9 ± 4.7 years in preterm deliveries (P = 0.22). Gestational age at the time of measurement was comparable between those with preterm and term deliveries (20.3 ± 1.6 vs. 19.9 ± 1.5 weeks; P = 0.36). Mean of measured CL by TVUS was significantly higher in term pregnancies in comparison to preterm pregnancies (33.5 ± 4.1 vs. 21.8 ± 6.0 mm; P < 0.001). In addition, the measured CL by TPUS was also higher in term pregnancies than in preterm deliveries (34.2 ± 4.6 vs. 22.6 ± 5.0 mm; P < 0.001).
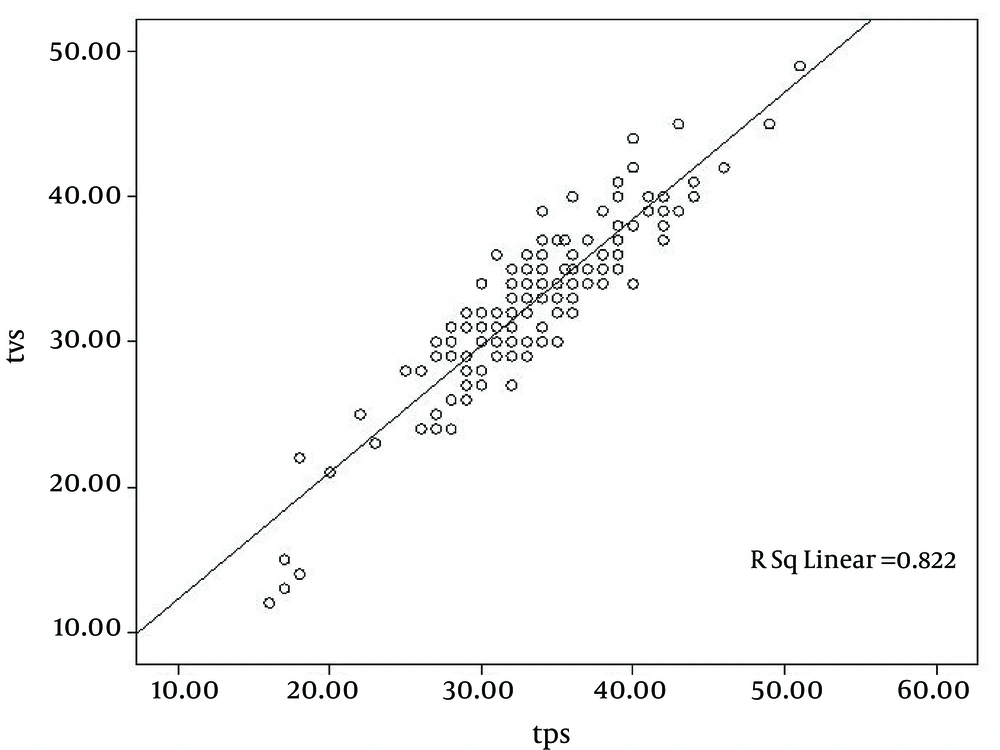
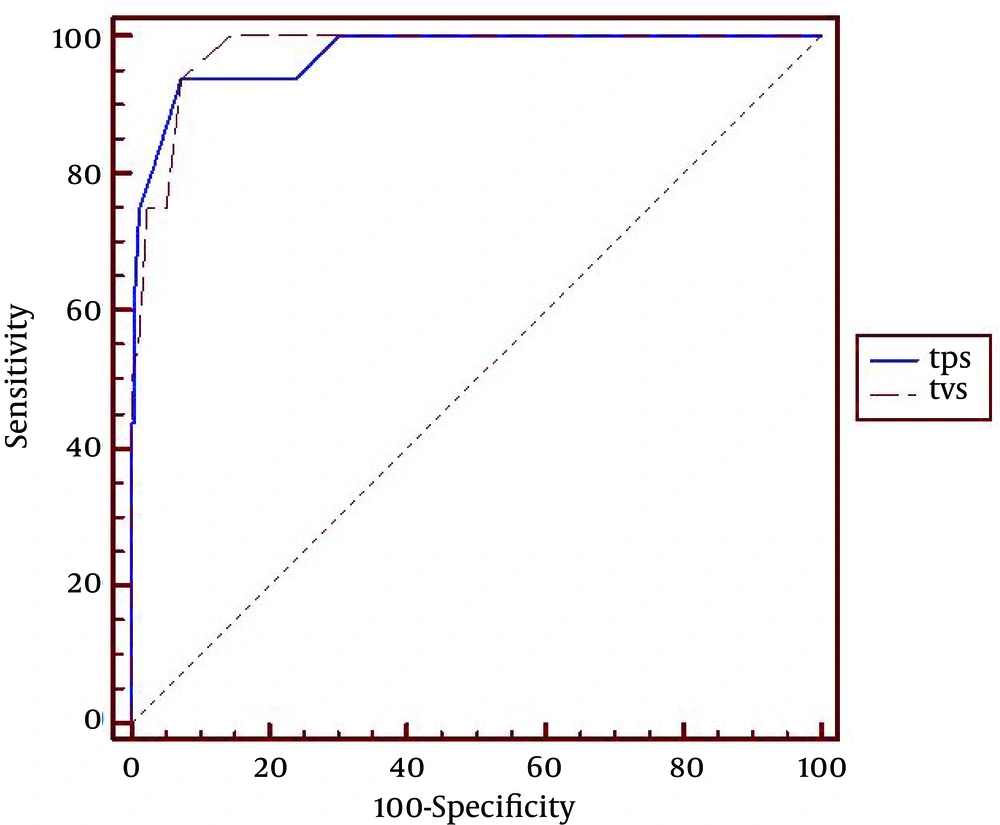
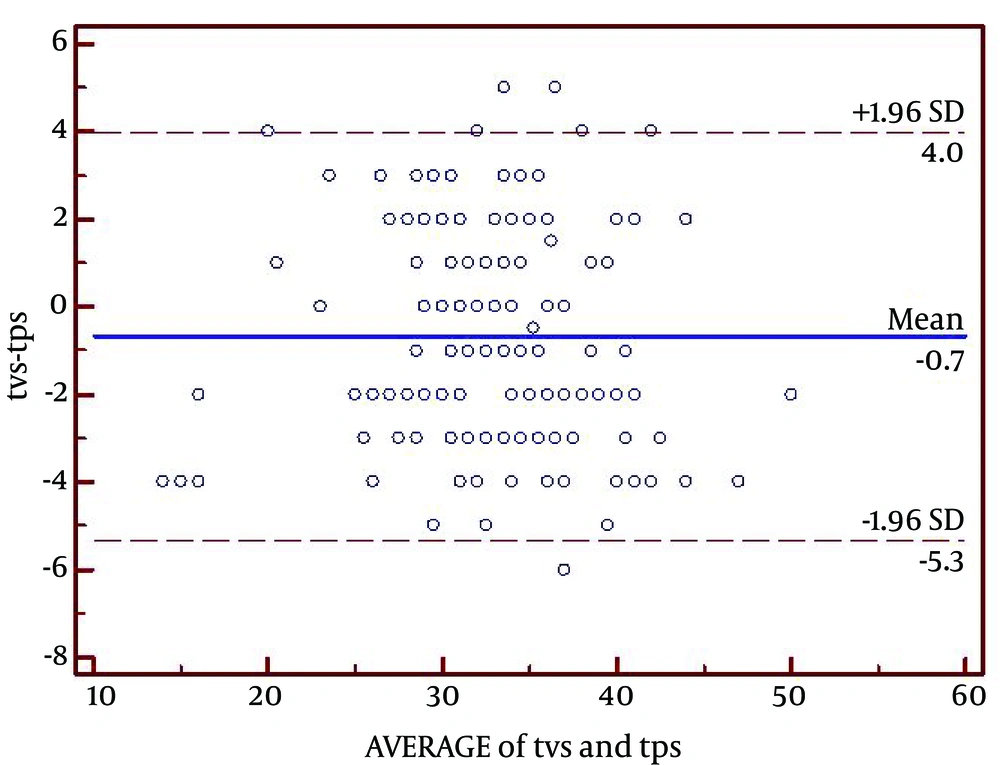
As shown in Figure 2, there was a strong correlation between TPUS and TVUS (r = 0.907; P < 0.001). The area under ROC curve was 0.973 for TPUS with cutoff point of 28 mm, sensitivity of 93.6% and specificity of 92.5% and 0.978 for TVUS with cutoff point of 28 mm, sensitivity of 93.75%, and specificity of 92.74% for predicting preterm delivery (Figure 3). In that regard, there was no significant difference between TPUS and TVUS (P = 0.70). The Bland-Altman plot indicated the difference between the paired means as -0.7 mm (95% CI, -5.3 to 4.0) (Figure 4).
5. Discussion
The rate of preterm delivery has remained stable over the last decade, ranging from 6% to 8% in Europe and Australia and from 9.6% to 11.6% in North America (11). Preterm deliveries are the main cause of neonatal morbidity and mortality (1-3). The understanding of pathogenic mechanisms leading to preterm delivery has improved greatly in the past several years (1). A recent systematic review has shown that medical prophylactic therapies are effective in preventing PTL but may not alleviate neonatal adverse outcomes including respiratory distress syndrome (12, 13). In this context, prostaglandin inhibitors and calcium channel blockers might delay delivery and improve neonatal outcomes. Thus, early identification of women at risk of preterm delivery is an important area for investigation (5).
TVUS has been shown to be an objective, reproducible, and reliable method to assess the cervix and to predict the risk of preterm delivery (6). TPUS has been introduced as an alternative method (7) because of some advantages including no need for inserting the transducer probe into the vagina, no image impairment due to obstruction by fetal parts, no need for an additional transducer, and being favored by most women (7, 8).
Some studies have confirmed feasibility of the TPUS (14) and approved its results to be as valid as that of TVUS (1, 15). Nevertheless, there are some restrictions to utilizing TPUS in clinical practice; for instance, a more experienced sonographer is needed (7). The patients’ preference for one method over the other varies regarding the level of convenience and experienced pain during the procedures (7, 14). In that regard, patient preference should be investigated further.
The TVUS might be associated with increased rate of prenatal infections because of entering the bacteria into upper parts of the vaginal; however, the complications of the TVUS are limited. Bennett et al. (16) reported the complication rates following TVUS in a series of 2670 patients. They reported vaginal hemorrhage in 229 patients (8.6%) while pelvic infections were reported in 18 (0.6%). Out of these 18 patients, 9 (0.3%) developed severe pelvic infection with abscess formation. Interestingly, the most common route of pelvic infection was the direct inoculation of the bacteria through the vaginal by means of the vaginal probe (16).
In our study, preterm delivery occurred at a rate of 8.2%, which was similar to the rate in European countries and Australia and lower than the rate in North America (11). The percentage differences might be due to the sample size, eligibility criteria, or race (17).
Our optimal cutoff value for CL measurements by TVUS to predict preterm delivery was 28 mm (sensitivity, 93.75%; and specificity, 92.74%), which was within the range reported in other studies (15-30 mm) (18). Other investigators had reported different cutoff points in their studies on predicting preterm delivery. reported cutoff points by other investigators include Leung et al. at ≤ 27 mm (sensitivity, 36.8%; and specificity, 96.2%) (19), Gramellini et al. at ≤ 15 mm (sensitivity, 24%; and specificity, 93.9%) (20), Schmitz et al. at ≤ 30 mm (sensitivity, 95%; and specificity, 29%) (21), Vendittelli et al. at < 30 mm (sensitivity, 83.4%; and specificity, 50.1%) (22), Bagga et al. at ≤ 25 mm (sensitivity, 88.3%; and specificity, 60%) (23), and Yazici et al. at 32.5 mm (sensitivity, 72.1%; and specificity, 81.8%) (1). The wide range of CLs cutoff points in various studies might be due to their difference in eligibility criteria. Difference between our cutoff points and other studies might be due to small sample size. Some studies included women with PTL and gestation age ranging from 18 or 20 to 37 weeks (22, 23). Moreover, various studies had different definition of PTL, with gestational age varying from 34 to 37 weeks cutoffs (19, 20, 22, 24). Gramellini et al. reported the optimal cutoff point of ≤ 15 mm for CL to predict preterm delivery with gestational age ≤ 34 weeks at birth (20) in comparison to compared to < 37 weeks in our study.
This might account for different cutoff points in predicting PTL in various studies (19, 20, 22, 24). In our study, correlation between the TVUS and TPUS was very strong (r = 0.907 and P < 0.001). The estimated difference between the paired means was -0.7 mm (95% CI, -5.3 to 4.0 mm). Meijer-Hoogeveen et al., Kurtzman et al., Cicero et al., Yazici et al., and Owen et al. reported a strong correlation between TVUS and TPUS in measuring CL (r = 0.85, r = 0.95, r = 0.944, r = 0.83, and r = 0.38, respectively) (1, 6, 7, 25, 26).
This study had some limitations. First, eight obstetrics and gynecology residents attended the labor ward during the study period as part of their rotations. Different residents and physicians examined the patients at presentation. Thus, interobserver variability was inevitable. Second, the study might be underpowered because of the low incidence of preterm delivery, which might have led to type II error. Along with these limitations, there are several strengths in this study. We included a large study population that increased the power of the statistical analysis. Previous reports had only included a limited number of patients. A trained perinatologist performed all the ultrasonographic examinations, which decreased the interobserver variability to zero and increased the accuracy of all examinations. Therefore, the results of this study should be referred to with high reliability and low variability.
In conclusion, TVUS is the gold standard for measurement of CL. However, our study indicates that it can be substituted for TPUS in limited cases, especially in preterm premature rupture of membranes, where insertion of the device into the vagina should be avoided, or according to patient preference. The accuracy of TPUS is dependent on the experience of the sonographer, which might restrict its application in clinical practice.