Abstract
Background:
Coagulopathy is common after severe trauma or massive bleeding, and many studies have shown the benefits of co-administration of blood and plasma. Efforts are being made to improve the treatment of patients injured by blunt trauma using plasma infusion.Objectives:
This study focused on blood fibrinogen levels in patients with severe trauma and bleeding.Patients and Methods:
Twenty-eight patients who were admitted to the Rajaee (Emtiaz) Trauma Hospital were studied in this cross-sectional survey, which was conducted in August and September of 2013. The patients were male and over 16 years old, with an injury severity score greater than or equal to 16, diastolic blood pressure under 90 mmHg, a minimum 1500 cc of estimated blood loss, and a minimum of 2000 cc crystalloid fluid intake, and patients were not receiving blood or blood products at the time of the traumatic event. Upon patient arrival, blood samples were obtained to measure fibrinogen concentration before starting resuscitation for the patient. Administration of blood and blood products was then performed according to hospital protocol.Results:
Over three months, twenty eight patients were admitted with the above criteria. Among these patients, the fibrinogen levels of eight cases (28.57%) were reported as non-measurable. Fibrinogen levels in 10% of the patients were below the acceptable standard of admission to the center, which means that blood fibrinogen levels were lower than normal in a significant number of patients.Conclusions:
Severe tissue damage and bleeding significantly reduce fibrinogen levels, and the positive effects of administering plasma to severe trauma patients may be due to the fibrinogen that plasma provides. It is therefore important to discover safer ways to administer fibrinogen. We recommend that the amount of administered fibrinogen be controlled, and that a thromboelastography be conducted for all patients on arrival.Keywords
1. Background
Coagulopathy is common after severe trauma or massive bleeding (1). Acute coagulopathy of trauma occurs in patients with shock and results in organ dysfunction, increased transfusion requirements, critical care stays, and mortality. Early diagnosis of a coagulopathic state allows for the care of patients in shock and the management of massive transfusion (2). Although data suggest that a 1:1 ratio of fresh frozen plasma (FFP) to packed red blood cells (RBCs) reduces coagulopathy, this treatment has not been shown to translate into a survival benefit (3). Many studies have shown the benefits of concurrent administration of blood and plasma to blunt trauma victims, and albumin can offer benefits in the diverse clinical settings of these patients. Further trials are warranted to delineate optimal fluid regimens (4). Resuscitation with plasma in the acute phases of coagulopathy leads to mortality reduction, but in sub-acute phases it can lead to unwanted side effects such as increased incidence of transfusion related acute caring injury (TRACI) and other immune responses. In addition, because FFP is a human blood product, the risk of transmitting infectious agents such as HIV, HCV, and HBV could increase (5). Due to the above issues, the identification of fresh plasma is necessary to increase the survival and safety.
With identification, we can prevent contaminated FFP from being used in patients. One of the most important components of FFP that maybe effective in reducing mortality is fibrinogen. Fibrinogen is a coagulation protein that plays an important role in the coagulation pathway and will placed in acute phase reactant protein. Fibrinogen is often used in acute trauma a few hours after the injury. Fibrinogen also plays an essential role in clot formation and stability, and it seems to be the most vulnerable factor during severe injury (6). There are three treatment options for fibrinogen replacement: FFP, cryoprecipitate, and fibrinogen concentrate (FC).
Studies have also shown that low levels of fibrinogen are associated with further complications and less mortality for patients (7). Other studies have shown that administration of fibrinogen could reduce mortality in severe trauma (8) and also reduce the need for transfusion (9).
2. Objectives
The current study sought to demonstrate fibrinogen levels in critically ill patients before resuscitation with blood products.
3. Patients and Methods
Patients admitted to the Rajaee (Emtiaz) Trauma Hospital, the first level trauma center in Shiraz and southern Iran, were examined during a prospective study in August and September of 2013. Patients injured by car accidents who met the following conditions and criteria were studied: patients were male and over 16 years old, with diastolic blood pressure between 70 - 90mmHg, an injury severity score (ISS) of 16 or greater, without loss of consciousness, and with a crystalloid fluid intake of at least 2000 cc. They had not received blood or blood products prior to the incident. Blood samples were taken from patients for the measurement of blood fibrinogen upon admission to the center, before the administration of blood products.
4. Results
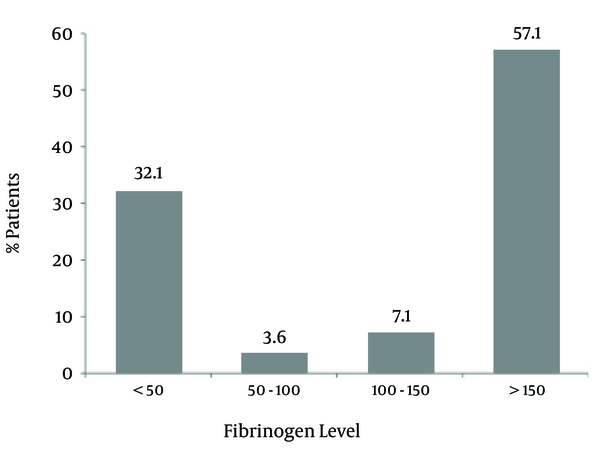
Twenty-eight patients with the aforementioned criteria were admitted to the resuscitation room of the Rajaee (Emtiaz) Hospital in Shiraz, in August and September of 2013. The minimum patient age was 17 years, and the maximum was 62. The average ISS was 18.4, and all patients had suffered fractures of the long bones or pelvis. The minimum ISS was 16, and the maximum was 27 (Table 1). In eight (28.57%) patients, fibrinogen levels were below 50 mg/dl, and in two patients they were between 50 and 100 mg/dl. This means that fibrinogen levels in 10 (35.7%) patients were below the acceptable standard of admission to the center, while these patients were received only two liters of crystalloid (Table 1). Figure 1 shows the fibrinogen levels of the patients who were admitted with major blunt trauma. It shows that fibrinogen levels were 57.1% between 55 - 60 of patients and 32.1 at the age of 30 years old.
Summary of Important Data
| Max | Min | Mean | |
|---|---|---|---|
| Age | 62 | 17 | 28.5 |
| ISS | 27 | 16 | 18.4 |
| Fibrinogen Level | 389 | 0 | 149.3 |
| Pre-hospital crystalloid, L | 4.5 | 2 | 2.3 |
Fibrinogen Levels of Patients Admitted with Major Blunt Trauma
5. Discussion
Coagulopathy in trauma is a result of multiple mechanisms, including substantial blood loss, decreased availability of coagulation factors, and dilution of remaining coagulation protein due to the administration of colloid and crystalloid fluids (10). Additional mechanisms have also been suggested for trauma induced coagulopathy, such as hyperfibrinolysis, hypothermia, and acidosis. Coagulation factors do not decrease homogeneously in severe bleeding, but coagulation factors levels can decrease during severe bleeding, and fibrinogen appears to reach critical levels at an early stage (11-13). Fibrinogen appears to be a derivate of acute phase reaction, and it has a crucial role in the coagulation pathway. It is also one of the compounds of FFP that is effective in reducing mortality in traumatic injury patients (13).
One major challenge in treating severe bleeding in trauma patients is determining whether the blood loss is due to coagulopathy or surgical causes. If the patient is coagulopathic, it is better to specify the cause of coagulopathy. Because studies have shown that co-administration with FFP plasma and packed RBCs reduces mortality in severe trauma cases, the administration of FFP in these cases has greatly increased (14).
A study by Geeraedts et al. (15) showed that the majority of massively transfused patients who exsanguinated the first 24 hours after hospital admissions received inadequate amounts of FFP and PC. Recent studies have shown that early and aggressive transfusion of FFP and PC is associated with a higher survival rate among major trauma patients (16-21).
Many studies are being conducted in regard to the ideal ratio of FFP to packed RBCs, but there is currently no consensus. The last meta-analysis ratio was a 1:1.4 of FFP to packed RBCs (22). A study by Mitra et al. (22) has shown increased initial survival in association with higher FFP to packed RBC ratios during massive transfusion of blunt injuries. This study also showed that the association is difficult to interpret because of an inherent survival bias. Along with the increase in prescribed FFP, some studies have shown that FFP administration leads to increased morbidity in the sub-acute phases of trauma (23). Massive transfusion should reflect an equal ratio of packed RBCs and FFP to limit coagulopathy, and prospective randomized trials are needed to standardize an effective protocol (24).
Studies show that FFP prescription, despite a positive impact in reducing mortality, directly increases the risk of morbidity and complications in some patients (23). Therefore, finding a way to isolate fibrinogen from FFP may make it easier for patients to benefit from FFP while avoiding its adverse effects.
This study showed that in a significant number of patients, blood fibrinogen levels were lower than normal. Therefore, we suggest that the blood fibrinogen levels of trauma patients be determined, either by direct measurement or indirect measurements such as thromboelastography. To better clarify the role of fibrinogen in trauma induced coagulopathy, it is important to arrange a study to measure the performance of fibrinogen in trauma patients. The risk of transfusion-associated infections should also be considered. Therefore, we should try to find the component of FFP that is responsible for the decrease in mortality and isolate it from FFP. With the administration of this component as a highly purified product, we will be able to avoid the complications and the side effects of transfusing fresh plasma. We suggest that fibrinogen alone or in contact with other unknown factors is one of the possible responsible factors. Therefore, administration of fibrinogen containing products in order to maintain blood fibrinogen levels above 150 - 200 gr/dl may help patients recover to a normal coagulation state and finally reduce mortality rates.
References
-
1.
Maegele M, Lefering R, Yucel N, Tjardes T, Rixen D, Paffrath T, et al. Early coagulopathy in multiple injury: an analysis from the German Trauma Registry on 8724 patients. Injury. 2007;38(3):298-304. [PubMed ID: 17214989]. https://doi.org/10.1016/j.injury.2006.10.003.
-
2.
Brohi K, Cohen MJ, Davenport RA. Acute coagulopathy of trauma: mechanism, identification and effect. Curr Opin Crit Care. 2007;13(6):680-5. [PubMed ID: 17975390]. https://doi.org/10.1097/MCC.0b013e3282f1e78f.
-
3.
Kashuk JL, Moore EE, Johnson JL, Haenel J, Wilson M, Moore JB, et al. Postinjury life threatening coagulopathy: is 1:1 fresh frozen plasma:packed red blood cells the answer? J Trauma. 2008;65(2):261-70. [PubMed ID: 18695460]. https://doi.org/10.1097/TA.0b013e31817de3e1.
-
4.
Haynes GR, Navickis RJ, Wilkes MM. Albumin administration--what is the evidence of clinical benefit? A systematic review of randomized controlled trials. Eur J Anaesthesiol. 2003;20(10):771-93. [PubMed ID: 14580047].
-
5.
Bica I, McGovern B, Dhar R, Stone D, McGowan K, Scheib R, et al. Increasing mortality due to end-stage liver disease in patients with human immunodeficiency virus infection. Clin Infect Dis. 2001;32(3):492-7. [PubMed ID: 11170959]. https://doi.org/10.1086/318501.
-
6.
Schlimp CJ, Schochl H. The role of fibrinogen in trauma-induced coagulopathy. Hamostaseologie. 2014;34(1):29-39. [PubMed ID: 24172764]. https://doi.org/10.5482/HAMO-13-07-0038.
-
7.
Toss H, Lindahl B, Siegbahn A, Wallentin L. Prognostic influence of increased fibrinogen and C-reactive protein levels in unstable coronary artery disease. FRISC Study Group. Fragmin during Instability in Coronary Artery Disease. Circulation. 1997;96(12):4204-10. [PubMed ID: 9416883].
-
8.
Schochl H, Nienaber U, Hofer G, Voelckel W, Jambor C, Scharbert G, et al. Goal-directed coagulation management of major trauma patients using thromboelastometry (ROTEM)-guided administration of fibrinogen concentrate and prothrombin complex concentrate. Crit Care. 2010;14(2):R55. [PubMed ID: 20374650]. https://doi.org/10.1186/cc8948.
-
9.
Shore-Lesserson L, Manspeizer HE, DePerio M, Francis S, Vela-Cantos F, Ergin MA. Thromboelastography-guided transfusion algorithm reduces transfusions in complex cardiac surgery. Anesth Analg. 1999;88(2):312-9. [PubMed ID: 9972747].
-
10.
Hess JR, Brohi K, Dutton RP, Hauser CJ, Holcomb JB, Kluger Y, et al. The coagulopathy of trauma: a review of mechanisms. J Trauma. 2008;65(4):748-54. [PubMed ID: 18849786]. https://doi.org/10.1097/TA.0b013e3181877a9c.
-
11.
Dunbar NM, Chandler WL. Thrombin generation in trauma patients. Transfusion. 2009;49(12):2652-60. [PubMed ID: 19682336]. https://doi.org/10.1111/j.1537-2995.2009.02335.x.
-
12.
Hiippala ST, Myllyla GJ, Vahtera EM. Hemostatic factors and replacement of major blood loss with plasma-poor red cell concentrates. Anesth Analg. 1995;81(2):360-5. [PubMed ID: 7542432].
-
13.
Fries D, Martini WZ. Role of fibrinogen in trauma-induced coagulopathy. Br J Anaesth. 2010;105(2):116-21. [PubMed ID: 20627882]. https://doi.org/10.1093/bja/aeq161.
-
14.
Schochl H, Maegele M, Solomon C, Gorlinger K, Voelckel W. Early and individualized goal-directed therapy for trauma-induced coagulopathy. Scand J Trauma Resusc Emerg Med. 2012;20:15. [PubMed ID: 22364525]. https://doi.org/10.1186/1757-7241-20-15.
-
15.
Geeraedts LMG, Demiral H, Schaap NP, Kamphuisen PW, Pompe JC, Frolke JP. 'Blind' transfusion of blood products in exsanguinating trauma patients. Resuscitation. 2007;73(3):382-8. [PubMed ID: 17292528]. https://doi.org/10.1016/j.resuscitation.2006.10.005.
-
16.
Borgman MA, Spinella PC, Perkins JG, Grathwohl KW, Repine T, Beekley AC, et al. The ratio of blood products transfused affects mortality in patients receiving massive transfusions at a combat support hospital. J Trauma. 2007;63(4):805-13. [PubMed ID: 18090009]. https://doi.org/10.1097/TA.0b013e3181271ba3.
-
17.
Cotton BA, Au BK, Nunez TC, Gunter OL, Robertson AM, Young PP. Predefined massive transfusion protocols are associated with a reduction in organ failure and postinjury complications. J Trauma. 2009;66(1):41-8. [PubMed ID: 19131804]. https://doi.org/10.1097/TA.0b013e31819313bb.
-
18.
Duchesne JC, Kimonis K, Marr AB, Rennie KV, Wahl G, Wells JE, et al. Damage control resuscitation in combination with damage control laparotomy: a survival advantage. J Trauma. 2010;69(1):46-52. [PubMed ID: 20622577]. https://doi.org/10.1097/TA.0b013e3181df91fa.
-
19.
Holcomb JB, Wade CE, Michalek JE, Chisholm GB, Zarzabal LA, Schreiber MA, et al. Increased plasma and platelet to red blood cell ratios improves outcome in 466 massively transfused civilian trauma patients. Ann Surg. 2008;248(3):447-58. [PubMed ID: 18791365]. https://doi.org/10.1097/SLA.0b013e318185a9ad.
-
20.
Lustenberger T, Frischknecht A, Bruesch M, Keel MJ. Blood component ratios in massively transfused, blunt trauma patients--a time-dependent covariate analysis. J Trauma. 2011;71(5):1144-50. [PubMed ID: 22071921]. https://doi.org/10.1097/TA.0b013e318230e89b.
-
21.
Maegele M, Lefering R, Paffrath T, Tjardes T, Simanski C, Bouillon B, et al. Red-blood-cell to plasma ratios transfused during massive transfusion are associated with mortality in severe multiple injury: a retrospective analysis from the Trauma Registry of the Deutsche Gesellschaft fur Unfallchirurgie. Vox Sang. 2008;95(2):112-9. [PubMed ID: 18557827]. https://doi.org/10.1111/j.1423-0410.2008.01074.x.
-
22.
Mitra B, Mori A, Cameron PA, Fitzgerald M, Paul E, Street A. Fresh frozen plasma (FFP) use during massive blood transfusion in trauma resuscitation. Injury. 2010;41(1):35-9. [PubMed ID: 19833331]. https://doi.org/10.1016/j.injury.2009.09.029.
-
23.
McMillian WD, Rogers FB. Management of prehospital antiplatelet and anticoagulant therapy in traumatic head injury: a review. J Trauma. 2009;66(3):942-50. [PubMed ID: 19276776]. https://doi.org/10.1097/TA.0b013e3181978e7b.
-
24.
Fraga GP, Bansal V, Coimbra R. Transfusion of blood products in trauma: an update. J Emerg Med. 2010;39(2):253-60. [PubMed ID: 19345046]. https://doi.org/10.1016/j.jemermed.2009.02.034.