1. Introduction
Cholecystectomy is one of the most common surgeries worldwide (1). Following acute or chronic cholecystitis due to bile duct obstruction and as a result of factors such as duct stone formation and bacterial infections, the patient with pain in the upper right quadrant of the abdomen, fever, and leukocytosis may visit a doctor (2, 3). After the final diagnosis of cholecystitis using diagnostic tests and confirmation by a specialist, the patient was prepared for surgery to remove the gallbladder. There are different methods for cholecystectomy surgery, including open surgery, total laparoscopic (4), and subtotal surgery (5). In cases where the gallbladder becomes severely attached to the liver due to inflammation, it is difficult to separate it from the liver bed; thus, surgeons may continue surgery with partial cholecystectomy or subtotal surgery (6). Sometimes part of the gallbladder remains in the body due to lack of access and visibility during surgery (7, 8). This method prevents damage to the liver and hepatic artery but will also cause complications such as bile leakage, postoperative pain, and recurrence of stones (9-11). A study showed that about 0.8% of people who undergo this surgical procedure die. Also, this surgical method increases the duration of hospitalization and treatment costs (1). Therefore, surgeons should be careful in choosing this surgical method and select it only when they have to because it can have many harmful complications for the patient. In this study, we introduced a patient who, after subtotal cholecystectomy, still had symptoms of gallbladder inflammation and underwent surgery to remove the remaining parts.
2. Case Presentation
A 41-year-old male patient was referred to a physician in July 2021 with symptoms of pain in the upper abdomen and fever. The patient's history indicated no underlying disease, but he had undergone cholecystectomy three months ago.
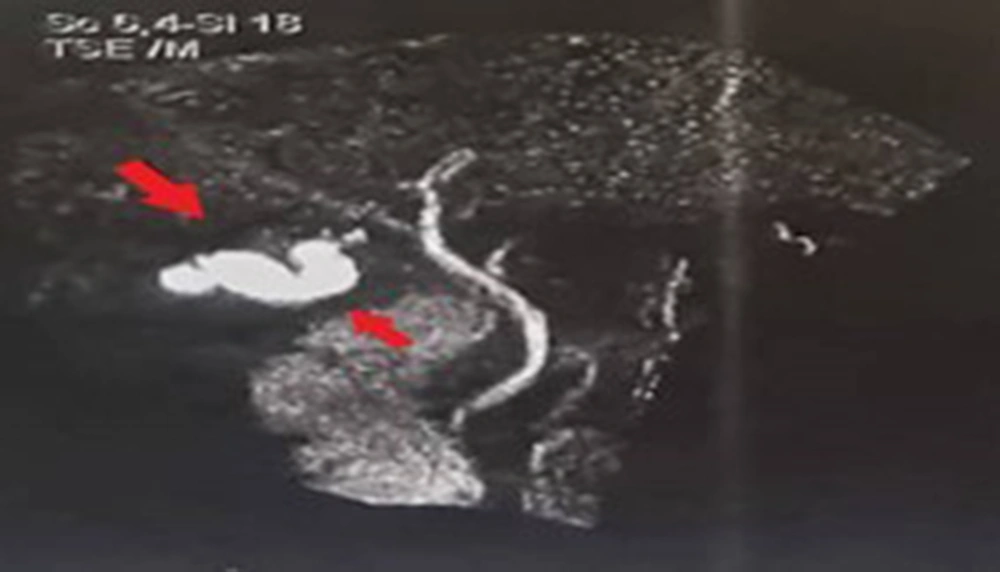
After the examination and according to the patient's surgical history, a specialist requested MRCP and ultrasound imaging of the abdomen and pelvis. The ultrasound showed that the liver, spleen, kidneys, bladder, and prostate were healthy and normal-sized, and no free fluid was seen inside the abdomen. Nevertheless, after the ultrasound imaging of the upper right quadrant, under the liver and in the gallbladder, a mass with dimensions of 20 × 33 × 33 and thickness of 2 mm with several stones with a diameter of 5 to 6 mm was observed (Figure 1). Also, the images obtained by the MRCP method confirmed their existence (Figure 2).
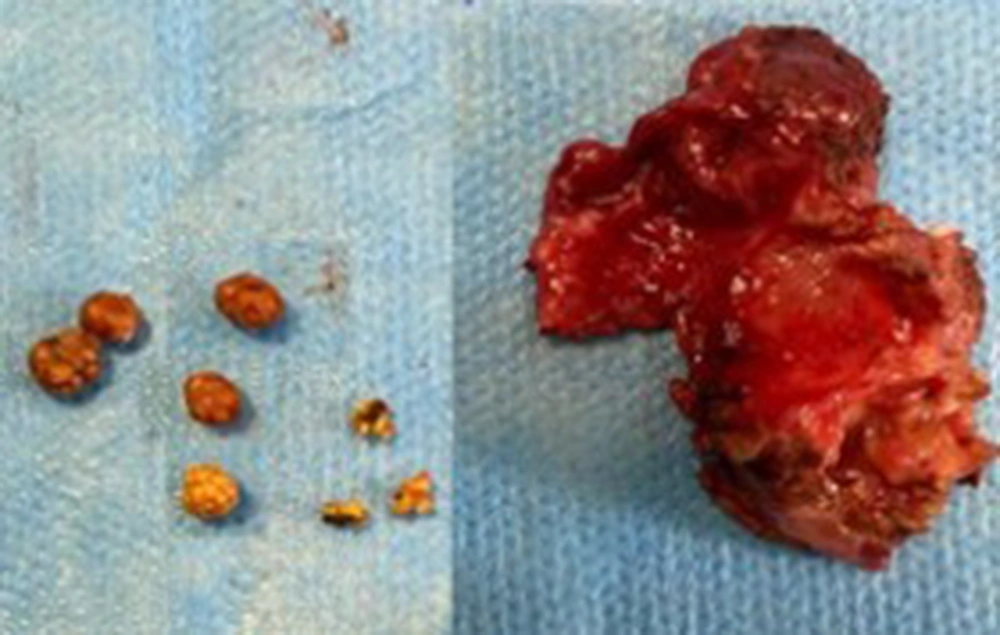
By referring to the patient's file and studying the report of the previous surgery, it was found that this mass was part of the gallbladder along with its stones, which were not removed during the last surgery performed by the subtotal method due to adhesion and the possibility of damage to the liver tissue. Finally, according to the evidence and symptoms, the patient again underwent laparoscopic cholecystectomy to remove the remaining tissues. In the second surgery, the surgeons removed all the remaining parts of the gallbladder along with the stones (Figure 3). After one day in the ward, the patient was discharged in good general condition. Within one month after surgery, the patient had no pain or complaints, and all symptoms related to the residual gallbladder disappeared.
3. Discussion
Laparoscopic gallbladder surgery is a common surgery worldwide. Because of the lack of damage to the abdominal wall, the creation of small incisions in the abdominal surface to inserting laparoscopic instruments, the reduced risk of complications following open surgery, and faster patient recovery, this surgery has been welcomed by surgeons (12). All these factors have made this method accepted by patients candidates for gallbladder removal surgery (13). However, in a study examining the opinions of 260 patients, the researchers concluded that patient satisfaction with the two surgical methods was not significantly different (14). Although surgeons and, in some cases, patients welcome laparoscopic surgery, this method can cause many complications (15). also, due to limited access, the surgeon may not successfully remove all the desired tissues or has to choose methods such as subtotal cholecystectomy (16). These tissue remnants may cause complications (17). In our case, part of the gallbladder with the stones remained inside, causing patient symptoms for three months.
Similar to our study, Demetriades et al. (16) introduced three patients who did not have a gallbladder removed after laparoscopic surgery, and the patients showed symptoms. All three patients showed gallbladder retention in 3 to 5 years after the first surgery in this study. However, in our study, the patient had intermittent periods of pain and fever from one week after surgery. In another study, El Nakeeb et al. (11) reported 21 patients who had gallbladders remaining after surgery, in which, like our study, ultrasound was used for diagnosis. However, cholangiography was also used in this study. In our research, because the ultrasound showed the remaining bile tissue well, there was no need to diagnose with cholangiography.
Finally, this study shows that performing subtotal cholecystectomy surgery imposes many costs on the patient and the treatment system due to the possibility of recurrence and the need for re-surgery. Therefore, the researchers recommend that total cholecystectomy surgery is the best option for treating patients, and the subtotal method should be minimized due to its complications and losses.