Abstract
Background:
Measles is one of the main causes of death among children, especially in developing countries. Although over 30 years have passed since the availability of measles vaccine; it is still uncontrolled in many countries.In Iran the highest incidence of confirmed measles cases have occurred in Sistan and Baluchistan province.Objectives:
This study was conducted to determine demographic and epidemiological characteristics of measles cases in order to improve strategies to eliminate measles in this province.Patients and Method:
All suspected and confirmed measles cases from April 2006 until March 2011 were evaluated in this province.Results:
Overall 456 suspected cases of measles were reported. 19.7% of cases were reported clinically positive, and positive test ratio was 56%. During our study measles incidence rate had increasing trend. The most incidence cases have occurred in spring and summer and the most cases have occurred in 1-4 years age group. Chabahar city has had the most confirmed cases. About measles vaccination history, 56.4% of all reported cases never vaccinated before.Conclusions:
Improving vaccination coverage and more accurate control of the cold chain can reduce probable outbreaks of measles and also it is proposed to expand health services in the eastern border to health control of immigrants.Keywords
1. Background
Measles is a vaccine-preventable disease and it is able to create outbreaks. Measles is one of the main causes of death among children, especially in developing countries (1, 2). Still, between the vaccine-preventable diseases, measles is the major cause of mortality in children, especially malnourished children (3). Although over 30 years have passed since the availability of measles vaccine, it is still uncontrolled in many countries, as in 2002, several European countries have reported outbreaks of measles (4) Iran Ministry of Health and Medical Education initiated comprehensive strategy to eliminate measles in 2002. These strategies included immunization for all people 5 to 25 years, by measles and rubella vaccine (MR) (5). Since 2004, routine vaccination program was carried out at 12 months and 4-6 years and in 2008 it was changed to 12 and 18 months. One of the goals of eliminating measles strategy in Iran is vaccination coverage of 95% in both the first and second dose (6). In Iran the highest incidence of confirmed measles cases have occurred in Sistan and Baluchistan province (7), considering the high incidence of measles disease in this province and several outbreaks of measles in recent years.
2. Objectives
This study was conducted to determine demographic and epidemiological characteristics of measles cases, and in order to evaluate and improve strategies to eliminate measles in this province.
3. Patients and Method
This is a cohort study that all suspected and confirmed measles cases from April 2006 until March 2011 were evaluated. All patients who were clinically reported by a physician were considered as clinical cases. The clinical diagnosis of Measles performed based on maculopapular rash (non vesicular) with a cough, coryza or conjunctivitis (7). The confirmation was performed by virological tests on blood, urine and throat specimens in health department of Tehran University of Medical Sciences. Epidemiologic data were collected from surveillance measles sheets that were available from control diseases centers in Zahedan Health Center. Then data were analyzed with SPSS 18 version.
4. Results
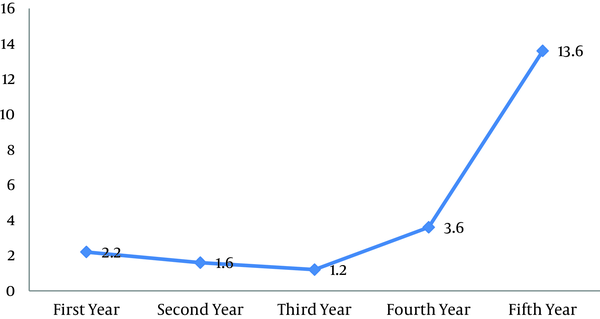
During our study, 456 suspected cases of measles were reported. 90 patients (19.7%0) have diagnosed only based on clinical manifestation or epidemiological contact. Laboratory confirmation test was performed for 366 patients (80.3%).Test result was negative in 161 patients and it was positive in 205 patients. On the other hand, positive test ratio (the ratio of patients who had positive result to all patients who performed serologic test) was 56%. Figure 1 shows incidence rate trend of suspected measles cases during five years. During our study measles incidence rate had increasing trend. As in the last year compared to the year before, it has had more than 4-fold increase.
Suspected Measles Incidence Rate (Case/100,000) during April 2006 to March 2011 inSistan and Baluchestan Province
The most incidence cases have occurred in spring and summer especially in May and June (respectively; 24.1% and 30.5%). Patient's demographic data is summarized in Table 1.As shown 87.7% (400 cases) of all patients were Iranian and 12.3% (56 cases) were foreigners. 50.9% of patients were male and 049.1% were female. Overall 65.3% were rural and 34.7% were urban. Among suspected patients who performed laboratory tests; there was no significantly statistical difference between test result (positive or negative) and residency (rural or urban), as well as between incidence cases and gender (based on χ2 test).
Demographic data and Vaccination History in Patients
| Patient group | Serologic Positive, No. | Serologic Negative, No. | Clinically Diagnosis, No. | Total, No. |
|---|---|---|---|---|
| City | ||||
| Zahedan | 29 | 32 | 18 | 79 |
| Khashan | 5 | 2 | 2 | 9 |
| Iranshahr | 10 | 26 | 8 | 44 |
| Saravan | 20 | 18 | 4 | 42 |
| Sarbaz | 9 | 21 | 5 | 35 |
| Nikshahr | 12 | 10 | 0 | 22 |
| Konarak | 26 | 17 | 9 | 52 |
| Chabahar | 94 | 35 | 44 | 173 |
| Vaccination History | ||||
| One dose | 23 | 30 | 19 | 72 |
| Two doses | 57 | 29 | 14 | 100 |
| No vaccination | 113 | 91 | 53 | 257 |
| Unknown | 12 | 11 | 4 | 27 |
| Residency | ||||
| Rural | 70 | 57 | 31 | 158 |
| Urban | 135 | 104 | 59 | 299 |
| Age Group, y | ||||
| < 1 | 16 | 11 | 10 | 37 |
| 1-4 | 80 | 85 | 53 | 218 |
| 5-9 | 70 | 27 | 17 | 114 |
| 10-14 | 22 | 18 | 0 | 40 |
| 15-19 | 1 | 6 | 0 | 7 |
| 20-24 | 4 | 3 | 4 | 11 |
| > 25 | 12 | 11 | 6 | 29 |
| Gender | ||||
| Male | 102 | 82 | 48 | 232 |
| Female | 103 | 79 | 42 | 224 |
| Nationality | ||||
| Iranian | 176 | 141 | 83 | 400 |
| Pakistani | 8 | 10 | 3 | 21 |
| Afghan | 21 | 10 | 4 | 35 |
The most cases (clinical and serological confirmed cases) have occurred in 1-4 years age group but the highest positive test ratio was related to 5-9 years of age whose difference was statistically significant (P < 0.001). Chabahar city has had the most confirmed cases (clinically and serologically) and based on χ2 test this difference between cities was statistically significant (P < 0.001).
About measles vaccination history, 56.4% of all reported cases never vaccinated before, 15.8% had vaccinated one dose and 21.9% had vaccinated 2 doses before. There was statistically significant relationship between confirmed measles and measles vaccination history in suspected patients (P < 0.001).
5. Discussion
Most cases in our study, belonged to age group 1 to 4 years and then to the age group 5 to 9 years. In various studies, different age groups were introduced as the most common age of measles incidence. In a study in Tehran by Mokhtari et al., most measles cases have been related to the age group 15 to 19 years (8). In a similar study in the years 2004 to 2008 by Zahra'i and colleagues in Iran, most cases were reported in age group 1 to 4 years (7). Al-Kuwari et al. conducted a study in Qatar in 2007 and concluded most measles cases have been occurred in the age group 5 to 14 years. They showed a significant difference between incidence cases (clinical and serological) and different age groups (1).
Our study significantly found relations between measles cases (clinical and serological) and measles vaccination history. Few infected persons are enough to circulate virus in a population of several hundred thousand people. And when the virus arrived in population, 90 to 100 percent of exposed non immune individuals develop clinical symptoms (5). Gradual accumulation of susceptible individuals to the disease caused by lack of proper vaccination or failure to response to the vaccine could be the underlying cause of measles outbreaks (4, 7, 9). Therefore, coverage improvement of vaccination can be effective in preventing the probable outbreaks. As Zahraie, et al. investigated measles epidemiology in Iran and concluded that after measles and rubella mass vaccination program the ratio of confirmed measles cases reduced (7).
More immunity is expected with increasing frequency of vaccine doses, as Mokhtari et al. in their study in Tehran showed, fewer cases of measles have reported in persons who had received two doses of vaccine than those who had received one dose of measles vaccine (8). But in our study, the more cases of measles have occurred in persons who had received two doses of vaccine than those who had received one dose of measles vaccine. So this could be due to poor quality of vaccines and low vaccine efficacy. In similar studies in some Eastern European countries, measles infection among vaccinated populations have been reported, as 41% of measles cases in Poland and 36% in Ukraine had received two doses of MMR vaccine1. Since the efficacy of measles vaccine is not 100 percent, usually 2 to 10% of vaccinated persons remain susceptible to measles, approximately, 95% of individuals seroconvert when measles vaccine is administered at first year of age or older (10, 11). Mokhtari et al. expressed that cause of low measles vaccine efficacy can be related to inaccurate and inadequate vaccine inoculation, the lack of a suitable solvent, inadequate cold chain or exposing the vaccine to light and heat (8). Yekta and colleagues in a study inUrmia city in northwestern Iran proposed to measure the IgG antibody titer against measles in order to determine the immunity in different age groups before and after vaccination (12). A study by Moodi and colleagues in primary schools in Zahedan city (Southeast of Iran) has showed that the current immunization program in Iran was not sufficient to establish enough immunity and proposed vaccination in ages 12-15 months and 4-6 years (13). Al-Kuwari et al. found an increase in measles cases in the spring and in the months of April and Junewhich was compatible with our results.
Most cases were reported from Chabahar city and the least cases from Khash city. Despite the cold weather in Khash city, the climate of Chabahar city is hot and humid that can cause cold chain disruption and reduce the vaccine efficiency in Chabahar city. So in such cities with hot weather, more accurate control of the cold chain appears to be essential.
Long border with Afghanistan and Pakistan and uncontrolled cross border traveling is another problem in measles surveillance (14). Zahraie et al. concluded that more measles incidence in Sistan and Baluchestan province than other areas in Iran can be due to foreigners traveling, dispersion rural population and high deprivation in province. They introduced low immunization coverage in the eastern neighbors of Iran and uncontrolled immigration and cross border travel as the most difficulties in measles elimination programs (7). Al-Kuwari and colleagues showed that 40 percent of measles cases in Qatar have occurred among Pakistani children who had not been vaccinated against measles (1).
Based on U.S. Department of Health and Human Services recommendation; before any international travel, children aged 6–11 months traveling outside the United States should receive 1 dose of measles, mumps, and rubella (MMR) vaccine, and children aged ≥ 12 months should receive 2 doses of MMR vaccine at least 28 days apart (15).
6. Conclusions
It is proposed to have more accurate control of the cold chain, improve the quality of measles vaccination in this province, and expand health services in the eastern border to health control of immigrants. Also contributing to improving vaccination coverage in eastern countries can reduce probable outbreaks of measles. Obviously, the success of such programs requires long term planning, the financial and human resources, inter-sectoral cooperation, careful management and continuous assessment.
Acknowledgements
References
-
1.
Alkuwari MG, Nazzal ZA, Alkhenji AA. Epidemiology of measles outbreaks in Qatar in 2007. Eastern Mediterranean Health J. 2011;17(3).
-
2.
Halsey NA. Measles in developing countries. BMJ. 2006;333(7581):1234. [PubMed ID: 17170396]. https://doi.org/10.1136/bmj.39058.361620.BE.
-
3.
Behjati M, Ayatollahi J, Karimi M, Tabatabaei F, Ghadiri A. Epidemiologic feature of measles in Yazd province Iran 1996 - 2000. Hakim J. 2002;6(3).
-
4.
Muscat M, Sciberras MT. owards Measles Elimination. Malta Med J. 2003;15:36-38.
-
5.
Zahraei SM, Dadras MN, Sabouri A. National guideline for measles Surveillance (Elimination Phase). 1th ed. Tehran Iran Ministry of health. Control Diseases Center. 2009.
-
6.
Shahmahmoodi S, Mehrabi Z, Eshraghian MR, Azad TM, Tabatabaie H, Yousefi M, et al. First detection of enterovirus 71 from an acute flaccid paralysis case with residual paralysis in Iran. J Clin Virol. 2008;42(4):409-11. [PubMed ID: 18403258]. https://doi.org/10.1016/j.jcv.2008.02.013.
-
7.
Zahraei SM, Gooya MM, Mokhtari Azad T. Epidemiological findings of measles in Iran 2004-2008. Iran J Infect Dis Trop Med. 2009;14(46):1-5.
-
8.
Mokhtari Azad T, Alavi Moghaddam M, Yadegari D, Salehi M, Shahim F, Zarebani I. Epidemiologic survey of documented measles outbreak in Tehran. Tabib-e-shargh J. 2004;6(2):123-128.
-
9.
Stanley A, Plotkin Walter A, Orenstein Pau l A. Vaccines. 2008.
-
10.
Orenstein WA, Markowitz L, Preblud SR, Hinman AR, Tomasi A, Bart KJ. Appropriate age for measles vaccination in the United States. Dev Biol Stand. 1986;65:13-21. [PubMed ID: 3549395].
-
11.
Moss WJ, Harry Feinstone W, Scott S. 2009. The Immunological Basis for Immunization Series. Module 7: Measles Update 2009: World Health Organization. Available from: http://www.who.int/immunization/documents/ISBN9789241597555/en/index.html.
-
12.
Yekta Z, Pourali R, Taravati MR, Shahabi S, Salary S, Khalily F, et al. Immune response to measles vaccine after mass vaccination in Urmia, Islamic Republic of Iran. East Mediterr Health J. 2009;15(3):516-25. [PubMed ID: 19731767].
-
13.
Mood BS, Naini RN, Salehi M, Kouhpayeh HR, Azad TM, Poor TN. Immunity against measles among vaccinated school going children in Zahedan, southeast of Iran. Indian J Med Microbiol. 2005;23(4):274-5. [PubMed ID: 16327132].
-
14.
Allam MF. Measles vaccination. J Prev Med Hyg. 2009;50(4):201-5. [PubMed ID: 20812514].
-
15.
Roper W, Moran J, Robert A. Measles Imported by Returning U.S Travelers Aged 6-23 Months, 2001-2011. Mortality and Morbidity Weekly Report.CDC. 2011;60(13):399.