1. Background
A high neuraxial block is one of the serious complications in obstetric epidural anesthesia (1). The term “high” is used to describe a higher level of sensorimotor block than that is required for the surgery. Since a high neuraxial block is associated with significant cardiovascular or respiratory compromise, rapid diagnosis and treatment are crucial for a better prognosis of obstetric patients. Previously, Hawkins et al. (2) showed that 9% of 129 anesthesia-related maternal deaths were caused by high neuraxial blocks. The prevention of high neuraxial block and appropriate management in the case of such incidents are relevant to decrease maternal deaths. The occurrence of a high neuraxial block, however, is rare (3-8). Therefore, a simulation study would be required for educating healthcare providers in the diagnosis and treatment of this serious complication.
2. Objectives
This study aimed to evaluate the effects of a simulation study of the high neuraxial block during epidural analgesia for labor pain on pre- and post-simulation tests in junior clinical trainees.
3. Methods
This prospective study was approved by the Ethics Committee of Hyogo College of Medicine. Twenty-two junior clinical trainees participated in this study from September 2016 to May 2017. The participants had graduated Medical School within one or two years and were under a two-month program for anesthesia during the Japanese Postgraduate Medical Education. They had been distributed toto hospitals for postgraduate education by test scores of Japan Residency Matching Program before graduation of Medical School. Written informed consent was obtained from all participants.
3.1. Pre- and Post-Simulation Tests
Before the simulation training, the participants passed a pre-simulation test (pretest), providing written responses on “how to approach and treat the rapid spread of anesthesia in painless epidural delivery” in a bullet-point form. After debriefing of simulation training, written responses were obtained to a posttest containing the same content as the pretest (posttest). Twelve correct answers for pretest and posttest, which had been selected based on previous studies (4, 5, 9-12), were as follows: mask ventilation, preparation for tracheal intubation, oxygenation, supraglottic airway placement, checking the breathing, checking oxygen saturation using pulse oximetry, checking blood pressure, ephedrine injection, checking epidural tube, assessing the level of sensory block, assessing the level of consciousness, and left uterine displacement. The assessment of the effects of the simulation study was performed by comparing the number of correct answers to 12 items in the pretest and posttest.
3.2. Simulation Training
The simulation training, including briefing and debriefing, was performed at the Hyogo College of Medicine Hospital under the supervision of a board-certified anesthesiologist of the Japanese Society of Anesthesiologists (JSA), using a simulator (SIMMAN®, Laerdal Medical AS, Stavanger, Norway) in accordance with a scenario that was originally developed by us for this study (Table 1). After the training, a debriefing was performed by the same board-certified anesthesiologist at the briefing and training, using a checklist modified from previous studies (Table 2) (4, 5, 9-12).
| Patient | Epidural Analgesia for Labor Pain | |
|---|---|---|
| A 25-year-old woman at gestational week 39 | An epidural catheter was inserted into the epidural space at the L3/4 level. 20 mL of 0.2% ropivacaine was administered epidurally. | |
| Time Course | Maternal State | Trainee Response |
| 1. Scenario start | ||
| 2. Rapid appearance of sensory block: worsening of physical status within 3 to 5 min after the start of the scenario | Lower limbs are numb | Verification of sensory block |
| Cannot move lower limbs | Verification of motor block | |
| Decrease in blood pressure (100/70 to 70/40 mmHg) | Differential diagnosis of high neuraxial block (e.g., anaphylaxis, amniotic fluid embolism, or pulmonary embolism) | |
| Decrease in oxygen saturation from 97% to 90% | ||
| Dyspnea, phonation difficulty | ||
| 3. Rapid cephalad spread of anesthesia | Unrest | Awareness of rapid exacerbations |
| Serious hypotension (55/30 mmHg) | Call for help | |
| Left uterine displacement | ||
| Pulse palpation | ||
| Rapid infusion, ephedrine injection: blood pressure recovers if these are performed. | ||
| Decrease in fetal heart rate to 80 - 100/min or lower | Airway management, ventilation: oxygen saturation recovers after the start of ventilation. | |
| Discontinuation of epidural administration | ||
| 4. Loss of consciousness | Respiratory arrest | ACLS survey |
| Cardiac arrest if airway management is inadequate | ||
| 5. Conclusion of the scenario | ||
The Scenario for Simulation Training of High Neuraxial Anesthesia During Epidural Analgesia for Labor Pain
| Details | |
|---|---|
| Technical skills | Symptoms and findings of the high neuraxial block (dyspnea, phonation difficulty, consciousness level) |
| Diagnostic method of the high neuraxial block (rapid cephalad spread of anesthesia, decreased oxygen saturation, bradycardia or arrhythmia, hypotension, respiratory suppression) | |
| Hypotension management (left uterine displacement, vasopressor, fluid infusion) | |
| Respiratory support (mask ventilation, tracheal intubation, cricoid cartilage compression) | |
| Cardiopulmonary resuscitation of the pregnant woman (call for help, defibrillator, emergency cart, difficult airway management trolley, ACLS survey, left uterine displacement, removal of cardiotocometer or labor monitoring device during defibrillation, preparation of fine tracheal tube, emergency or perimortem cesarean delivery) | |
| Knowledge | Mechanisms of high neuraxial block |
| Small divided dose administration for epidural analgesia | |
| Maximum dose of local anesthetic, effects on cardiovascular and respiratory systems | |
| Content and dose of the test dose | |
| Pharmacological effects of resuscitation drugs | |
| Physiological changes in the pregnant woman and factors affecting cardiopulmonary resuscitation (supine hypotension syndrome, increased oxygen demand) | |
| Laryngeal edema, enlarged tongue, decreased gastroesophageal sphincter muscle tone | |
| Non-technical skills | Was there adequate communication between the training members? |
| Were instructions clear? | |
| Was the communication closed loop? | |
| Call for help (as above) | |
| Who to call for help (skilled anesthesiologist, cardiac surgeon, clinical engineer, neonatal resuscitation team) | |
| Gather instruments (as above) |
Key Points of Scenario Debriefing
3.3. Statistics
All statistical tests were two-sided with a significance level of 5% and performed using JMS Pro version 13.1.0 (SAS Institute Inc. Cary, NC, United States). The response rates were evaluated by comparing the number of response items in the pretest and posttest. The Kruskal-Wallis test and the Wilcoxon test were used to compare the two variables.
4. Results
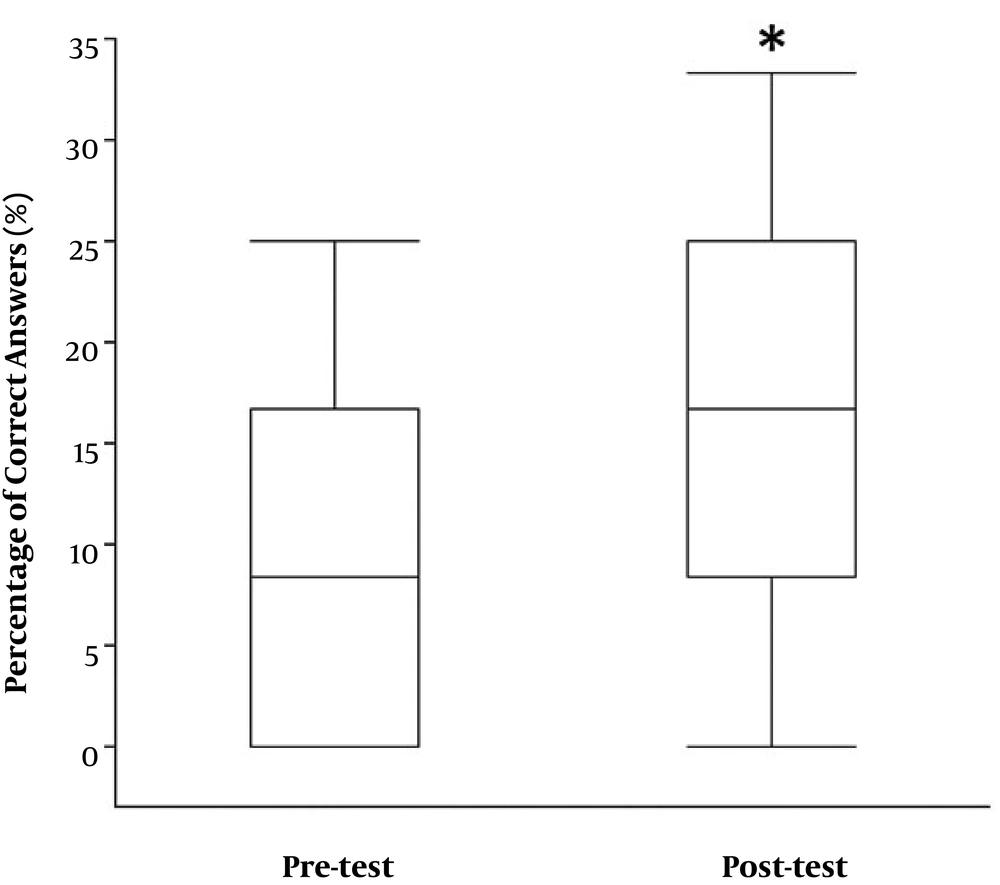
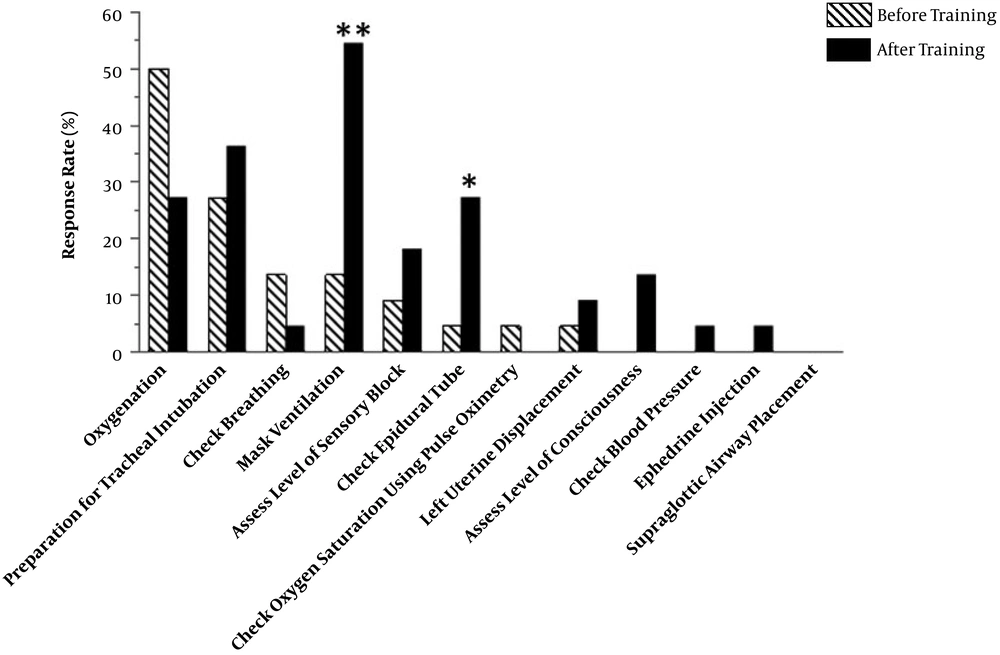
The response rate per participant significantly increased from 8.3% [0.0 - 16.7] to 16.7% [8.3 - 25.0] from the pretest to the posttest (P = 0.041) (Figure 1). Figure 2 shows the response rate of clinical trainees who answered the correct item in the 12 selected answers before and after training. The response rates for “mask ventilation” and “check epidural tube” significantly increased from 13.6% to 54.5% (P = 0.004) and from 4.5% to 27.3% from the pretest to the posttest (P = 0.039), respectively (Figure 2).
5. Discussion
Rapid diagnosis and treatment can save parturient patients who suffer high neuraxial block during epidural analgesia for labor and delivery. The present study showed that our simulation training of high neuraxial block for junior clinical trainees improved the response rate of 12 items, which are the required items for the rapid diagnosis and treatment at the time of high neuraxial block during epidural analgesia in pregnant women.
Davies et al. (13) investigated liability profiles in obstetric anesthesia claims and reported that high neuraxial block was the most common anesthetic cause of maternal death/brain damage in regional anesthesia claims. They also showed that “delay”, “inadequate monitoring”, “inadequate airway management in the labor room”, and “drug administration” were implicated in the claim reports (13). Since the incidence of this serious complication is fairly low (3-8), simulation-based education is needed to improve the appropriateness of diagnosis and treatment for high neuraxial anesthesia in healthcare providers. The respiratory arrest reportedly occurs at the early phase of a high neuraxial block (14, 15). Therefore, we set our scenario, in which either dyspnea or difficulty in vocalization occurs within 5 min after the start of the scenario. We also set the scenario, in which appropriate airway management recovers oxygen desaturation caused by respiratory arrest. After performing our simulation training, the response rate of “mask ventilation” increased dramatically in the present study. This improvement may represent the educational effects of our simulation training on rapid diagnosis and treatment of high neuraxial block during epidural analgesia in labor.
Our simulation training system, including pretest, posttest, scenario, and checklist, was originally developed and its validity was assessed for the first time in the present study. Since our study comprised a small number of participants, further investigations are required to evaluate the validity and stability of this training system in larger participants.
The increased ratio of the response rate per participant was low even after a debriefing of our training scenario in the present study. To increase the response rate, further improvement of our training system is needed for better management of high neuraxial block during epidural analgesia for labor. The prevention of high neuraxial blocks is also relevant to decrease maternal death, in addition to appropriate management. High neuraxial block can be prevented by injecting small divided doses of local anesthetic through an epidural tube (4, 16). Since the present scenario starts after the occurrence of the high neuraxial block during epidural analgesia, a new scenario is required to educate the prevention of high neuraxial block during epidural analgesia.
In conclusion, we performed a scenario simulation of inadvertent high spinal block occurring after epidural anesthesia in a pregnant woman to investigate the validity of the simulation training for junior clinical trainees using a manikin simulator. We found that the response rates for “mask ventilation” and “check epidural tube” significantly improved after the simulation training. A simulation training is one of the effective methods to educate rapid diagnosis and treatment of high neuraxial block.