1. Background
Laparoscopic surgery is increasing in frequency in many laparotomy procedures. It is also well-established in gynecological surgeries in the Trendelenburg position (1-3). Laparoscopy is used to diagnose and treat gynecological pathologies such as pelvic lymphadenectomy, ovarian cyst removal, myomectomy, fallopian tube ligation, hysterectomy, and diagnosis of infertility (2, 4). Although it can provide distinct advantages by decreasing the length of hospitalization, offering better cosmetic outcomes, and reducing the bleeding and pain after the surgery, pneumoperitoneum requirement and the position during laparoscopy raise concerns about the management of anesthesia during the surgery (5, 6). The insufflation of carbon dioxide (CO2) into the peritoneum to keep away the abdominal organs increases the Intra-abdominal Pressure (IAP) up to 12 - 14 mmHg, which affects respiratory and cardiac function (7). The Trendelenburg position also increased IAP from 8.8 to 13.3 mmHg (8). All of these can predominantly increase intraperitoneal CO2, resulting in the cranial displacement of the diaphragm (9). This displacement can lead to decreased respiratory capacity, including Functional Residual Capacity (FRC), decreased compliance, increased airway pressure, and increased resistance and ventilation-perfusion mismatch (7, 10-12). On the other hand, general anesthesia can also impair respiratory function by developing atelectasis (12, 13). Taken together, during prolonged laparoscopic procedures, changes in cardiorespiratory parameters can have clinically significant adverse effects such as reduced arterial oxygenation in the patient (12, 13). Various intraoperative ventilatory techniques have been used to prevent these changes. positive-pressure ventilation (PPV) has been widely used for controlling ventilation, but it can increase the airway pressure in pneumoperitoneum and Trendelenburg position (14, 15). Pressure-controlled ventilation (PCV) is one of the suggested methods to be used during general anesthesia. Mechanical ventilation with Positive End-Expiratory Pressure (PEEP) can affect respiration and hemodynamics during pneumoperitoneum by increasing FRC and reducing atelectasis (10, 15, 16). It is not common to use PEEP routinely in the surgical situation, and it is preferred to be used in high-risk patients such as CO2 embolization cases (1).
2. Objectives
Based on the paucity of data regarding the effect of PEEP and its amount during laparoscopy, we aimed to evaluate the effect of different levels of PEEP on the respiratory status of patients undergoing gynecologic laparoscopy.
3. Methods
3.1. Study Population
After gaining approval from the Ethics Committee (code 1395.1277.IR.TBZMED.REC) and obtaining written informed consent for the double-blind randomized clinical trial, the study was conducted prospectively on 60 patients (ASA physical status I, aged 18 - 60 years) who underwent general anesthesia for gynecologic laparoscopy in the Shohada Tajrish Medical Center. Consecutive patients were selected based on their entrance. The technique of randomization was performed via randomly permuted blocks using online software (www.randomizer.org). The double-blind technique was used to blind both participants and members of the research team. Patients were excluded from the study if they had BMI > 30, systemic diseases including cardio-cerebrovascular, hepato-renal, and respiratory diseases, psychological disorders, emergency surgery, cigarette smoking, the history of atopy and refusal to participate.
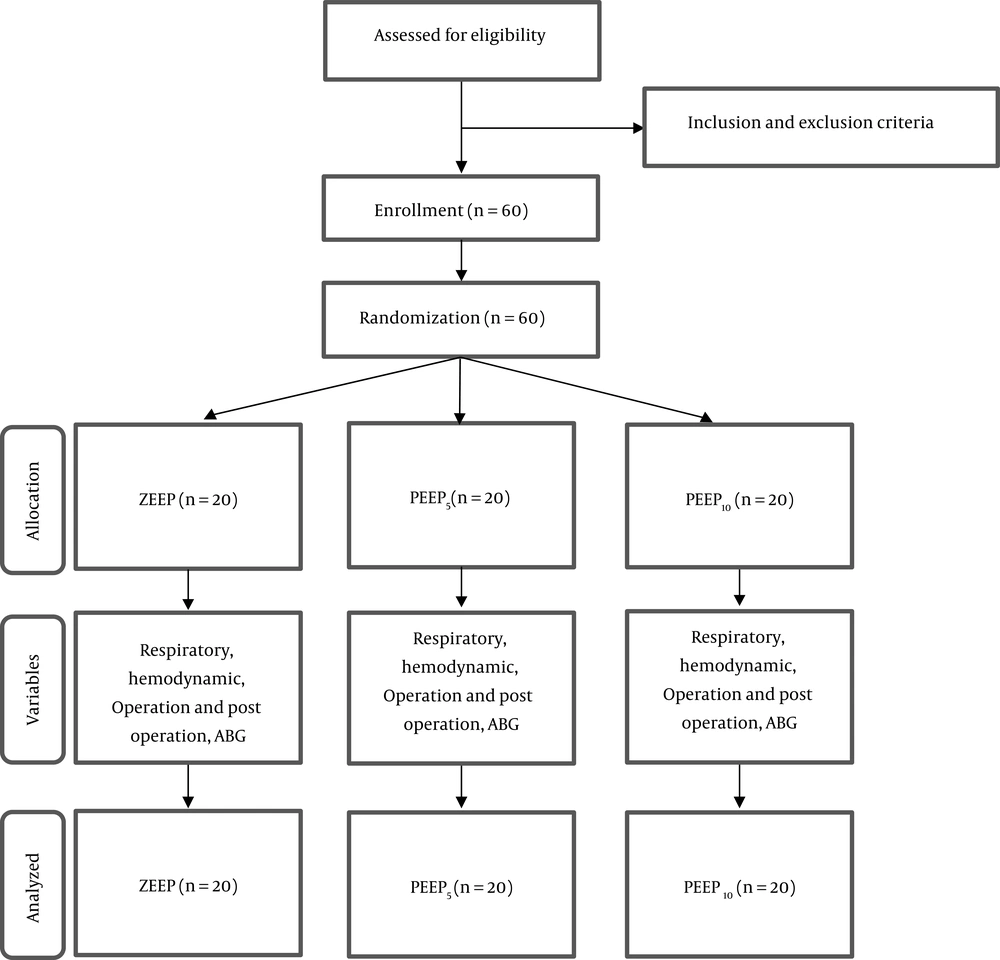
The patients were randomized to treatment by the 1:1:1 ratio. The randomization was done by online rand list software into three groups (n = 20 in each group): ZEEP (PEEP = 0 cmH2O), PEEP5 (PEEP = 5 cmH2O), and PEEP10 (PEEP = 10 cmH2O). Respiratory and hemodynamic variables of patients including heart rate (HR), blood pressure (BP), mean arterial pressure (MBP), peripheral capillary oxygen saturation (SPO2), and end-tidal carbon dioxide (EtCO2) pressure were compared before general anesthetic induction and immediately after CO2 insufflation at intervals of 5, 10, 20, 30, and 60 min and the end of the operation in the three study groups. Operative and postoperative variables, including operation time, duration of anesthesia, pneumoperitoneum time, intravenous (IV) volume, bleeding volume, urine output, and dysrhythmia, were recorded. Blood samples were obtained for arterial blood gas (ABG) analysis after anesthetic induction, immediately before CO2 insufflation, and 30 min after the initiation of operation. The infusion of ephedrine (5 - 20 mg) and atropine (0.5 - 3 mg) was given to the patients if blood pressure and heart rate reduced more than 25%, and adrenaline (0.1 - 5 mg) was infused to maintain the anesthesia. If their blood pressures and heart rates did not increase, they were excluded from the study. Figure 1 illustrates the patient selection process of the study in three groups.
3.2. Anesthetic Induction
As premedication, the patients received 10 - 12 mL/kg/h normal saline intravenously. General anesthesia was induced with 0.03 mg/kg midazolam, 1 μg/kg remifentanil, 2 mg/kg propofol, and 0.5 mg/kg atracurium. After induction, the trachea was intubated with an endotracheal tube of appropriate size (7 - 7.5). During the operation, patients’ non-invasive blood pressure (NIBP), electrocardiography (ECG), SpO2, and EtCO2 were monitored. After the insertion of a Veress needle, carbon dioxide (CO2) was insufflated into the peritoneum. The insufflation of the peritoneum with CO2 was maintained at a pressure of 12 - 14 mmHg with a flow of 1 - 2.5 L/min. Thereafter, the reverse Trendelenburg position was standardized at an angle of 30 degrees. Anesthesia was maintained with the infusion of propofol 50 - 150 μg/kg/min, remifentanil 0.1 - 1 μg/kg/min, and atracurium 0.2 - 0.3 mg/kg, if needed. The patients were mechanically ventilated (Fabius, Drager Medical; S-ORC AG&CO.kg Germany, D023452 Lubeck). They were ventilated with positive pressure ventilation (PPV) and volume-controlled ventilation (VCV) with a tidal volume (TV) of 10 mL/min, respiratory rate of 12 breaths/min, an inspiratory-to-expiratory ratio of 1:2 to maintain EtCO2 between 35 and 45 mmHg, and airway pressure of 30 mmHg.
3.3. Statistical Analysis
The statistical analysis was performed using IBM SPSS software for Windows (version 16.0). The data were expressed as mean ± standard deviation. Statistical comparison of variables was conducted by the chi-square test. The multivariate analysis of variance (repeated-measures ANOVA) was used to evaluate the differences in variables. For evaluating the effect of time, we used the post hoc test. Multiple regression analysis was performed to predict the multivariate effect of variables. A P value of less than 0.05 was considered statistically significant.
4. Results
In this study, 60 women (mean age: 30.28 years) with ASA I underwent gynecological laparoscopy under general anesthesia and were included in the final analysis. The mean pneumoperitoneum time was 61.81 ± 17.68, the operation time was 70.43 ± 18.42, and anesthesia time was 81.73 ± 18.42. The most performed surgery was ovarian cystectomy, with a frequency of 24 (40%) patients (Table 1).
| Variables | ZEEP (N = 20) | PEEP5 (N = 20) | PEEP10 (N = 20) | P Value |
|---|---|---|---|---|
| Age, y | 30.05 ± 7.42 | 28.35 ± 6.58 | 32.45 ± 7.47 | 0.201 |
| Weight, kg | 68.80 ± 11.21 | 68.45 ± 11.21 | 74.50 ± 9.79 | 0.080 |
| Height, cm | 160.35 ± 4.33 | 161.85 ± 5.28 | 162.30 ± 3.98 | 0.374 |
| Type of surgery | 0.180 | |||
| Ovarian cyst | 25 (5) | 50 (10) | 45 (9) | |
| EP | 35 (7) | 35 (7) | 15 (3) | |
| Infertility | 40 (8) | 15 (3) | 40 (8) | |
| Pneumoperitoneum time, min | 57.95 ± 23.18 | 68.95 ± 13.51 | 58.55 ± 13.07 | 0.085 |
| Operation time, min | 66.00 ± 24.54 | 76.95 ± 13.77 | 68.35 ± 13.86 | 0.141 |
| Anesthesia time, min | 77.90 ± 24.85 | 88.00 ± 13.39 | 79.30 ± 13.83 | 0.172 |
4.1. Hemodynamics and Respiration Variables
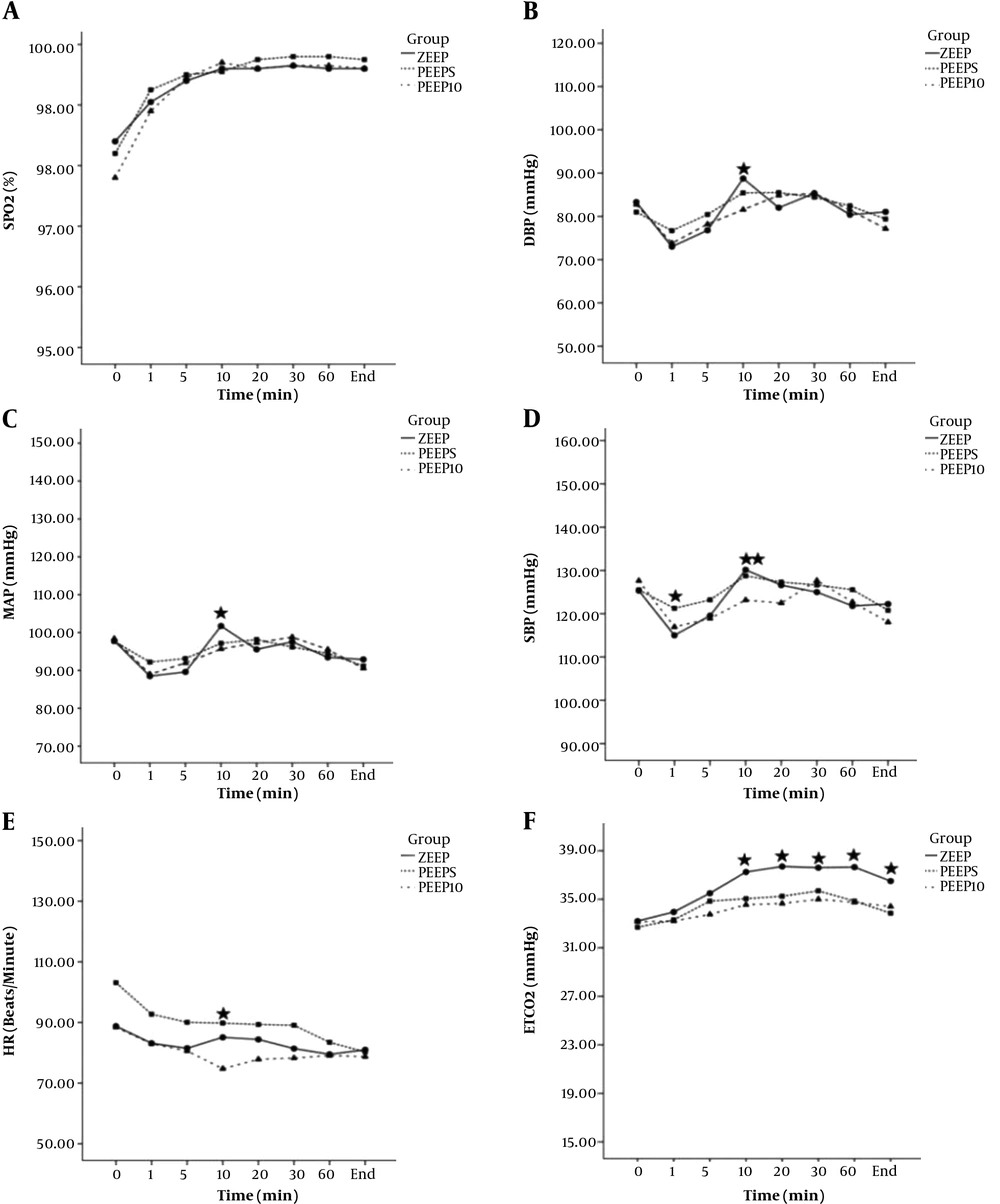
Systolic blood pressure difference was statistically significant between ZEEP and PEEP5 (P = 0.016) immediately after pneumoperitoneum induction and also between ZEEP and PEEP10 (P = 0.012) 10 min after induction. Diastolic blood pressure, MBP, and HR were statistically significantly different between ZEEP and PEEP10 groups 10 min after induction (P = 0.009, P = 0.003, and P = 0.002, respectively). The EtCO2 difference between ZEEP and PEEP10 was also significant at 10, 20, 30, and 60 min and after the operation (P = 0.001, P = 0.002, P = 0.001, P = 0.019, and P = 0.004, respectively). In comparison, SPO2 was not statistically significant between the three groups (P > 0.05) (Figure 2).
4.2. Gas Exchange
Table 2 demonstrates the ABG analysis immediately before CO2 insufflation and also 30 min after the initiation of operation. Besides, pH after pneumoperitoneum was statistically significantly different between the ZEEP and PEEP5 groups (P = 0.016) and also between ZEEP and PEEP10 (P = 0.006). After the pneumoperitoneum, the reduction of pH was significantly more in the ZEEP group than in the other groups.
| Variables | ZEEP (N = 20) | PEEP5 (N = 20) | PEEP10 (N = 20) |
|---|---|---|---|
| pH | |||
| T1 | 7.42 ± 0.02 | 7.42 ± 0.03 | 7.42 ± 0.03 |
| T2 | 7.26 ± 0.07 | 7.31 ± 0.04 | 7.32 ± 0.05 |
| P value | 0.003 | 0.198 | 0.201 |
| PaO2 | |||
| T1 | 248.30 ± 127.59 | 196.50 ± 153.21 | 138.75 ± 108.85 |
| T2 | 208.10 ± 146.87 | 201.79 ± 147.76 | 244.75 ± 145.76 |
| P value | 0.005 | 0.289 | 0.028 |
| PaCO2 | |||
| T1 | 31.51 ± 4.79 | 35.11 ± 13.34 | 32.75 ± 4.56 |
| T2 | 45.88 ± 8.86 | 46.16 ± 12.73 | 39.60 ± 7.32 |
| P value | 0.047 | 0.034 | 0.047 |
| HCO3- | |||
| T1 | 20.54 ± 2.56 | 20.57 ± 2.06 | 20.70 ± 1.80 |
| T2 | 20.11 ± 2.34 | 19.89 ± 5.43 | 20.47 ± 2.47 |
| P value | 0.978 | 0.781 | 0.977 |
| BE | |||
| T1 | -2.79 ± 1.87 | -2.60 ± 1.78 | -2.62 ± 2.07 |
| T2 | -6.42 ± 3.03 | -5.01 ± 1.94 | -5.02 ± 2.71 |
| P value | 0.001 | 0.003 | 0.010 |
| SPO2 | |||
| T1 | 98.74 ± 1.82 | 95.36 ± 10.51 | 97.05 ± 2.37 |
| T2 | 87.06 ± 27.11 | 97.20 ± 3.33 | 98.20 ± 3.22 |
| P value | 0.089 | 0.098 | 0.103 |
In addition, PaO2 was statistically significantly different between ZEEP and PEEP10 after pneumoperitoneum with the P value of 0.028. The reduction in PaO2 after pneumoperitoneum was significantly more in the ZEEP group than in the other groups before pneumoperitoneum. In addition, the increase in PaO2 was significantly more in the PEEP10 group than in the PEEP5 group after pneumoperitoneum.
However, PaCO2 showed no statistically significant differences between the groups. The increase in PaCO2 was higher in the ZEEP group than in other groups after pneumoperitoneum, and it was significantly higher in PEEP5 than in PEEP10. Besides, HCO3, BE, and SPO2 showed no statistically significant differences between the groups. There were no differences between the groups before and after pneumoperitoneum in HCO3. However, BE had statistically significant differences within the groups. Also, SPO2 was significantly lower after pneumoperitoneum in the ZEEP group than in other groups. Although SPO2 was higher in the PEEP5 and PEEP10 groups after pneumoperitoneum, the amount of SPO2 did not show any difference in these groups.
4.3. Complications and Treatment After Operation
Table 3 demonstrates major complications and management after pneumoperitoneum induction in the three groups. The mean IV volume was 1800 ± 368.11 milliliter (mL). There were significant differences between ZEEP and PEEP10 (P = 0.001) and also between PEEP5 and PEEP10 (P = 0.002) in the IV volume infusion, while PEEP10 received the least IV volume infusion.
| Variables | ZEEP (N = 20) | PEEP5 (N = 20) | PEEP10 (N = 20) | Total | P Value |
|---|---|---|---|---|---|
| Intraoperative fluid, mL | 19.60 ± 335.84 | 1940 ± 237.64 | 1500 ± 330.47 | 1800 ± 368.11 | 0.001 |
| Bleeding, mL | 112 ± 92.88 | 108 ± 50.01 | 39 ± 56.65 | 86.33 ± 75.88 | 0.002 |
| Urinary output, mL | 182 ± 92.99 | 187.50 ± 85.77 | 110.75 ± 47.46 | 160.08 ± 84.39 | 0.004 |
| Complications, % | |||||
| Hypertension | 1 (5) | 2 (10) | 2 (10) | 5 (8.3) | 0.804 |
| Tachycardia | 2 (10) | 2 (10) | 1 (5) | 5 (8.3) | 0.804 |
| Dysrhythmia | 4 (20) | 4 (20) | 1 (5) | 9 (15) | 0.308 |
| Treatment, % | |||||
| Ephedrine | 1 (5) | 0 | 2 (10) | 3 (5) | 0.349 |
| Phenylephrine | 0 | 3 (15) | 0 | 3 (5) | 0.043 |
| Atropine | 2 (10) | 5 (1) | 5 (1) | 4 (6.7) | 0.765 |
| Lidocaine | 4 (20) | 4 (20) | 1 (5) | 9 (15) | 0.308 |
The mean bleeding volume was 86.33 ± 75.88 mL. There were statistically significant differences between the groups. The bleeding volume was lower in PEEP10 than in ZEEP (0.001) and PEEP5 (P = 0.001). The lowest bleeding volume was seen in the PEEP10 group.
The mean urinary output was 160.08 ± 84.39 mL. The PEEP10 group had the lowest volume of urinary output, and there were significant differences between PEEP10 and ZEEP (P = 0.003) and PEEP5 (P = 0.002).
The most frequent complication after pneumoperitoneum induction was dysrhythmia, which occurred in nine patients (15%), mostly in the ZEEP and PEEP5 groups. It was statistically significant between ZEEP and PEEP10 (P = 0.004). The most medical treatment after dysrhythmia was lidocaine injection in nine patients (15%). There were significant differences between ZEEP and PEEP5 (P =0.002) and also between ZEEP and PEEP10 (P = 0.007) in receiving lidocaine injection, with the ZEEP group being at the top.
5. Discussions
Because the diaphragm is mechanically attached to the abdominal wall, an increase in intra-abdominal pressure can cause a cranial shift of the diaphragm and decrease FRC (2, 17-19). Pneumoperitoneum induction also affects the circulatory system by increasing MAP and mean systemic filling pressure. The application of PEEP has been beneficial for both prophylaxis and therapy of the patients during laparoscopy to improve oxygenation, decrease atelectasis in the lungs, increase FRC (12, 20), and preserve the circulatory system (12). In this study, we aimed to evaluate the effects of different levels of PEEP on respiratory function during gynecologic laparoscopy. In all three groups, respiratory status was not affected by confounding variables such as age, weight, and height. Although PEEP can interfere with intra-thoracic pressure and reduce venous return and cardiac output, the administration of adequate levels of PEEP has been advocated as a therapeutic modality to improve oxygenation and hemodynamics (AHSHEMZADEH) (VMF Mendez). In our study, the use of PEEP5 caused a modification in blood pressure, MAP, HR, and SPO2, and PEEP10 had more hemodynamic effects than PEEP5. Our study showed that the application of PEEP after pneumoperitoneum induction in patients submitted to gynecological laparoscopy surgery in the Trendelenburg position under general anesthesia could improve the ABG exchange such as pH and PaO2.
Luz et al. performed laparoscopic lymphadenectomy in a dog model study. Their study demonstrated that the combination of increased intra-abdominal pressure and PEEP could significantly reduce the hemodynamic variables during laparoscopy. Our result is in line with their results. Although, in our study, MAP increased 20 ± 10 min after pneumoperitoneum induction, this may be due to the differences in human and animal species (20).
Cinnella et al. performed a study on patients undergoing pelvic laparoscopy in the Trendelenburg position. They showed the application of PEEP after pneumoperitoneum induction led to the improvement of the chest wall and lung elastance. Moreover, they found that PEEP of 5 cmH2O led to the improvement of HR (2). Our result showed that the induction of PEEP of 10 cmH2O could increase HR after 10 min.
In the current study, those patients who received PEEP10 had less IV volume requirement than patients in other groups, and they had less bleeding volume, as well. It is suggested that the increased bleeding volume can be the result of increased afterload in the left ventricle due to pneumoperitoneum induction. However, the application of PEEP10 reduced the bleeding volume during the surgery, so increased left ventricular afterload could be reserved by applying moderate PEEP10. Fellahi et al. investigated eight healthy individuals to evaluate the effect of PEEP on hemodynamics during abdominal hyper-pressure. They found that the application of moderate PEEP of 10 cmH2O could significantly decrease the intra-abdominal pressure and consequently decrease the left ventricular end-diastolic volume (21). In this study, we demonstrated that the application of PEEP could decrease the hemodynamic instability by increasing intra-abdominal pressure as a result of the decrease in end-systolic left ventricular wall stress.
In our study, SaO2 was higher in the PEEP5 group than in other groups. In patients undergoing pneumoperitoneum induction, abdominal hyper-pressure and reduction in lung capacity would decrease the FRC. Previous studies showed the main effect of PEEP is to increase FRC by eliminating atelectasis formation. Neumann et al. conducted a study on 13 patients undergoing elective diagnostic gynecologic laparoscopy. They observed that using PEEP10 could improve SaO2 and prevent atelectasis formation (22).
Russo et al. investigated the effects of ventilation with PEEP of 5 cmH2O and 10 cmH2O on the respiratory system and cardiac function by using transthoracic echocardiography. They showed that PaO2 values were improved in the PEEP groups, and both PaCO2 and EtCO2 increased after gas insufflation in the control group. Although both were decreased with PEEP10, using PEEP5 only improved the EtCO2 values (7). In the current study, the increases in PaCO2 and EtCO2 were lower in PEEP10 than in other groups after pneumoperitoneum induction. In addition, similar to Russo et al. study, EtCO2 was lower only in PEEP5.
Dysrhythmia was the most frequent complication that occurred after pneumoperitoneum induction in our study. It was significantly lower in the PEEP10 than in other groups, which could lead to the absorption of CO2 and the increase of PaCO2. Applying a high level of PEEP demonstrated to eliminate this complication. Gutt et al. investigated the effect of CO2 insufflation on the occurrence of complications after laparoscopy. They found that hypercarbia and acidosis following CO2 insufflation could lead to hemodynamic changes through the cardiovascular system and sympathoadrenal stimulation. The direct effects of increased PaCO2 and acidosis include decreasing cardiac contractility and sensitization to the arrhythmogenic effects of catecholamines (9).
The laparoscopic procedure is increasingly performed under general anesthesia, but respiratory compromises after pneumoperitoneum induction raise concerns about the adverse effects on respiratory mechanics. Despite different factors affecting the respiratory status, applying PEEP demonstrated to improve atelectasis caused by pneumoperitoneum, as well as gas exchange and oxygenation.
5.1. Conclusion
Based on the results, the PEEP application was associated with the improvement of ABG in patients with gynecologic laparoscopy. The application of PEEP of 10 cm H2O had a greater effect on the improvement of respiratory parameters and complications of pneumoperitoneum such as hemodynamic instability including hemorrhage, tachycardia, and hypertension. Further studies are required to perform on larger populations and the elderly because age can influence respiratory mechanisms and SPO2.