1. Background
Due to the high expense of complex and painful surgeries, many governments attempt to encourage these surgeries to be conducted as day surgery. This has caused a considerable change in inpatient and outpatient surgery (1). Although painful surgeries can be performed in an ambulatory setting, the postoperative analgesia after day surgery can become an enormous challenge for patients. Unlike hospital stay which provides the patients specialized personnel, different types of analgesics, and various routes of administration (2, 3), home care can have a lot of limitations in terms of the mentioned factors (4). This can explain the high prevalence of acute pain in the first 24 - 48 hours after acute day surgery, despite the increased awareness and introduction of multimodal pain therapy strategies over the last decades (5-10). Studies on postoperative pain after day surgery mostly focus on the first 24 - 48 hours after the surgery because it is believed that the postoperative pain diminishes quickly over time. Consequently, most pain-treatment schedules are prescribed for only the first 2 - 5 postoperative days (11, 12). However, more than 35% of patients undergoing typical painful ambulatory surgical procedures (e.g., inguinal hernia repair, hemorrhoid surgery, arthroscopic knee, and shoulder surgery) still suffer from moderate to severe pain on the fourth POD (4, 13). Therefore, the scope of postoperative pain research should be extended to the first week and the first month after the painful types of daily surgery. An optimal description of the acute postoperative pain trajectory in the first month after surgery can be a valuable asset to develop future procedure-specific pain-treatment schedules.
Proper adherence to prescribed postoperative pain medication is a prerequisite to prevent the pain after ambulant surgery (14). Adherence is “the extent of similarity between the patient's actual dosage and the predefined schedule” (15). The reasons for medication non-adherence are categorized into two groups: intentional and unintentional (16). Unintentional non-adherence can occur when a patient wants to follow the schedule but is prohibited due to a poor recall or financial issues (14, 16). Intentional non-adherence can occur when the patient is deliberately not adhering to the treatment schedule because of fear of adverse effects (14, 16). It has already been demonstrated that analgesic non-adherence and partial adherence after day surgery is rather common (14). However, there is limited research regarding the reasons for analgesic non-adherence and partial adherence, intentional or unintentional non-adherence.
2. Objectives
The present study aimed to compare 4-week postoperative pain profiles of 4 painful ambulatory surgical procedures and analyze the prevalence and reasons for non-adherence and partial adherence to a pharmacological treatment schedule after day surgery.
3. Methods
In this propective and observational survey, we analyzed the data from a large randomized trial to evaluate whether or not metamizole combined with paracetamol is non-inferior compared to ibuprofen combined with paracetamol in the treatment of postoperative pain after different types of ambulant surgery at the JESSA Hospital Hasselt, Belgium. These data have been published in the European Journal of Anaesthesiology (17). The study protocol was already published in Trials (2). This study was approved by the ethical committee of the JESSA Hospital Hasselt, Belgium (Chairperson Dr. Koen Magerman, registration number 15.105/pijn15.02), and the European Union Drug Regulating Authorities Clinical Trials (EudraCT Number 2015-003987-35) on 21 September 2015. The inclusion criteria included all patients between ≥ 18 and ≤ 70 years old with a bodyweight of > 50 kg and < 100 kg scheduled for ambulatory haemorrhoid surgery, shoulder or knee arthroscopy, and inguinal hernia repair with an American Society of Anaesthesiologists’ (ASA) physical status 1 to 3. The exclusion criteria were patients with an ASA score > 3, patients with a bodyweight < 50 kg or > 100 kg, age < 18 years and > 70 years, hospital stay, pregnancy and breastfeeding, cognitive impairment or lack of understanding of the Dutch language, severe liver or kindney dysfunction, preoperative pharmacologic treatment of pain (opioids) and/or a history of chronic pain, fibromyalgia, Chronic Regional Pain Syndrome, a history of drugs, alcohol or opioids abuse, the use of medication with a suppressive effect on the central nervous system for instance benzodiazepins, the use of anti-rheumatic treatment, allergies to or contraindications for the use of metamizole, paracetamol or ibuprofen (or other NSAIDs), porphyria, asthma, rhinosinusitis or nasal polyps, COPD or emphysema, chronic obstipation, hypotension, heart failure, haematological disease, ulcus pepticum or gastro-intestinal bleeding (active or anamnesis), gastro-intestinal bleeding or perforation due to the use of cyclooxygenase inhibitors in anamnesis, congenital deficiency of glucose-6-phosphate dehydrogenase, fever or other signs of infection, and patients undergoing arthroscopy shoulder: refusal of an interscalene block.
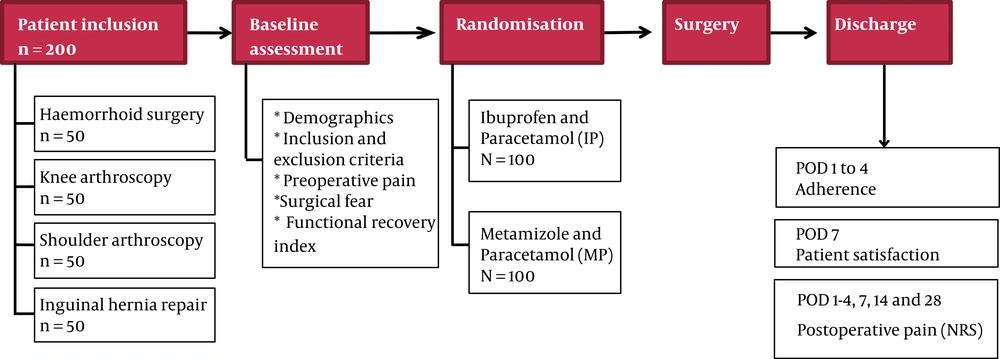
An overview of the study set-up was provided in Figure 1.
Baseline assessment included the patients’ demographics, profession, education, body mass index (BMI), history of (related) surgery and fear of the surgery (18, 19), evaluated with an 8-item questionnaire covering a range of short-term (item 1 - 4, i.e afraid of operation, anesthesia, postoperative pain, side effects, health deterioration) and long-term (item 5 - 8, i.e. failed operation, incomplete recovery, and long duration of rehabilitation ) surgery-related fears. All items are scored on an NRS scale ranging from 0 (not at all afraid) to 10 (very afraid). This results in a score of 0 - 40 for each subscale and a total score of 0 to 80. Moreover, pre-operative pain and expected pain were measured by an 11-point numerical rating score (NRS) where 0 indicates no pain; 10 indicates the worst possible pain. The impact of pain on daily life was measured with an NRS scale where 0 indicates no influence at all, and 10 indicates the maximum amount of influence. Finally, the baseline functional recovery index (FRI) was evaluated. FRI is a validated questionnaire developed to evaluate the recovery of patients after discharge and covers different items categorized into 3 groups: pain together with social activities, the functioning of the lower limbs, and physical activity (20).
3.1. Perioperative Procedure
Patients who underwent a shoulder arthroscopy received an interscalene block preoperatively. Interscalene blocks were performed according to the extra-plexic technique described by Spence et al. (21). An in-plane ultrasound-guided puncture was made through the middle scalene muscle. The tip of the needle was placed inferoposterior to the C6 root without making contact with the neural structures (extraplexic technique). After confirming the extravascular position of the needle tip, 20 mL of 0.75% ropivacaine was incrementally injected under continuous ultrasound vision. General anaesthesia was induced with alfentanil 10 mcg/kg i.v., sufentanil 0.15 mcg/kg i.v., and propofol 2mg/kg i.v. Patients scheduled for a shoulder arthroscopy or an inguinal hernia repair received rocuronium 0.6 mg/kg i.v. before endotracheal intubation. A laryngeal mask airway was inserted in other patients. Anesthesia was continued with sevoflurane together with a mixture of 50:50 air/oxygen. Postoperatively, all patients received bolus injections of piritramide 2 mg intravenously until an NRS ≤ 3 was achieved in the Post Anaesthesia Care Unit (PACU). All patients received the treatment schedule along with the instructions before discharge. Patients were randomized to the combination of metamizole with paracetamol (MP) or the combination of ibuprofen with paracetamol (IP). Patients in the MP-group were instructed to take metamizole 1gr orally three times a day for 4 PODs and patients in the IP-group were instructed to take ibuprofen 600 mg orally 3 times a day for 4 PODs. All patients were instructed to take paracetamol 1 g orally four times a day during the first 4 POD. The first dose of study medication was given 30 minutes before surgery. Rescue medication consisted of oral tramadol 50 mg up to 3 times a day if pain relief wasn’t satisfactory. An accurate treatment plan was provided to the patients, and the exact cases showed the time required to obtain the IP/MP along with the oral instructions of the study team, stating that proper adherence to analgesics could prevent postoperative pain. Finally, they were contacted daily to assess adherence to a pre-defined treatment schedule.
3.2. Outcome Measures
Average postoperative pain together with average pain at movement and in rest was measured with an NRS scale at discharge and at POD 1, 2, 3, 4, 7, 14, and 28 to create a 4-week pain profile. Moderate pain is defined as an NRS > 3, severe pain as an NRS > 5 (13).
Adherence to MP/IP was assessed at POD 1 to 4 as follows: Full adherence: analgesia use as prescribed “Yes, the treatment schedule is always followed”, partial adherence: analgesia use as prescribed “No, the treatment scheduled is not followed for 1 or 2 POD”, non-adherence: analgesia use as prescribed “No, the treatment schedule is never correctly followed”. The satisfaction of the patients concerning the MP/IP was evaluated with an 11-point NRS scale with 0 indicating not satisfied and 10 indicating fully satisfied on POD 7.
3.3. Statistical Analysis
All data were anonymized and saved into an online CRF (Questback) and eventually exported to SPSS 24.0 (IBM® SPSS® Inc, Chicago, Illinois, USA) to analyze outcome measures. Multiple imputations (10) were issued to account for missing baseline values. Continuous data were shown as mean (standard deviation) (SD) or median (25th - 75th percentile) and categorical data as numbers (%). Analyses were performed with the student’s t-test in case of parametric data, the Mann-Whitney U test in case of nonparametric data, and Pearson’s χ2 or Fisher’s exact test (in case of an observed count < 10) for categorical data. Values of P ≤ 0.05 were considered statistically significant. Graphs were made using Prism 7.0 (Prism®, GraphPad Software Inc, La Jolla, California, USA).
4. Results
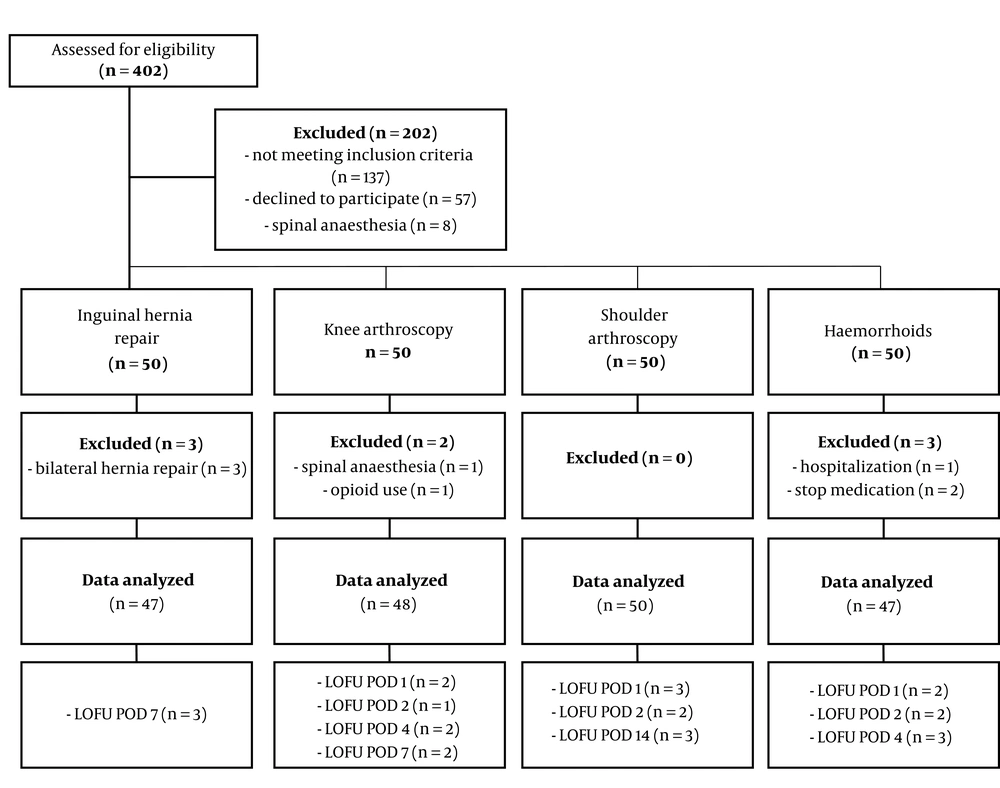
A flow chart of patient selection and exclusion stratified per type of surgery is depicted in Figure 2. Baseline and perioperative characteristics are presented in Table 1.
| Haemorrhoids (N = 50) | Inguinal Hernia Repair (N = 47) | Knee Arthroscopy (N = 49) | Shoulder Arthroscopy (N = 50) | |
|---|---|---|---|---|
| Age (years) | 48.5 (37.8 - 56.0) | 58.0 (46.0 - 62.0) | 50.0 (44.0 - 59.5) | 49.0 (42.0 - 53.3) |
| Gender (m/f) | 31/19 (62.0/38.0) | 44/3 (93.6/6.4) | 36/13 (73.5/26.5) | 20/30 (40.0/60.0) |
| Profession | ||||
| Unemployed | 14 (28.0) | 21 (44.7) | 13 (26.5) | 12 (24.0) |
| Employed | 35 (70.0) | 26 (55.3) | 36 (73.5) | 38 (76.0) |
| Missing | 1 (2.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Education | ||||
| Primary/junior secondary | 9 (18.0) | 11 (23.4) | 9 (18.4) | 16 (32.0) |
| Higher secondary | 27 (54.0) | 19 (40.4) | 24 (48.98) | 16 (32.0) |
| Tertiary | 14 (28.0) | 17 (36.2) | 16 (32.7) | 17 (34.0) |
| Missing | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (2.0) |
| ASA-classification | ||||
| ASA I | 15 (30.0) | 19 (40.4) | 23 (48.9) | 14 (28.0) |
| ASA II | 31 (62.0) | 26 (55.3) | 18 (36.7) | 28 (56.0) |
| ASA III | 2 (4.0) | 0 (0.0) | 2 (4.1) | 3 (6.0) |
| Missing | 2 (4.0) | 2 (4.3) | 6 (12.2) | 5 (1.0) |
| Operation last year (yes/no)? | 10/40 (20.0/80.0) | 6/41 (12.8/87.2) | 10/39 (20.4/79.6) | 11/39 (22.0/78.0) |
| Related to surgery (yes/no)? | 1/9 (30.0/70.0) | 0/6 (0.0/100.0) | 4/6 (40.0/60.0) | 4/7 (36.4/63.6) |
| Last week: pain related to surgery/condition (yes/no/missing)? | 25/21/4 (50.0/42.0/8.0) | 22/22/3 (46.8/46.8/6.4) | 27/11/1 (55.1/22.4/2.0) | 45/2/3 (90.0/4.0/6.0) |
| Average pain | 4.0 (3.5 - 8.0) | 3.5 (2.0 - 5.0) | 4.0 (3.0 - 6.0) | 6.0 (6.0 - 8.0) |
| Impact pain on daily life | 5.0 (2.0 - 8.0) | 2.0 (1.8 - 5.0) | 4 (2.5 - 6.0) | 6.0 (5.0 - 8.0) |
| Short-term surgical fear | 17.0 (8.3 - 24.0)b | 10.0 (4.0 - 19.8)c | 9.0 (3.0 - 15.0)d | 11.0 (6.0 - 22.0)d |
| Long-term surgical fear | 6.0 (3.0 - 12.0)d | 5.0 (1.0 - 9.0)e | 5.5 (3.0 - 11.8)c | 12.0 (7.0 - 18.0)d |
| Expected pain | 7.0 (6.0 - 8.0)f | 5.0 (3.0 - 6.0)e | 5.0 (3.0 - 7.0)d | 5.0 (2.0 - 7.0)e |
| Duration of surgery (min) | 14.0 (10.0 - 20.0) | 22.0 (18.0 - 30.0) | 28.0 (21.5 - 29.0) | 43.0 (39.0 - 53.0) |
aData are presented as median (25th - 75th percentile) or as absolute numbers (%).
bN = 49
cN = 44
dN = 47
eN = 43
fN = 48
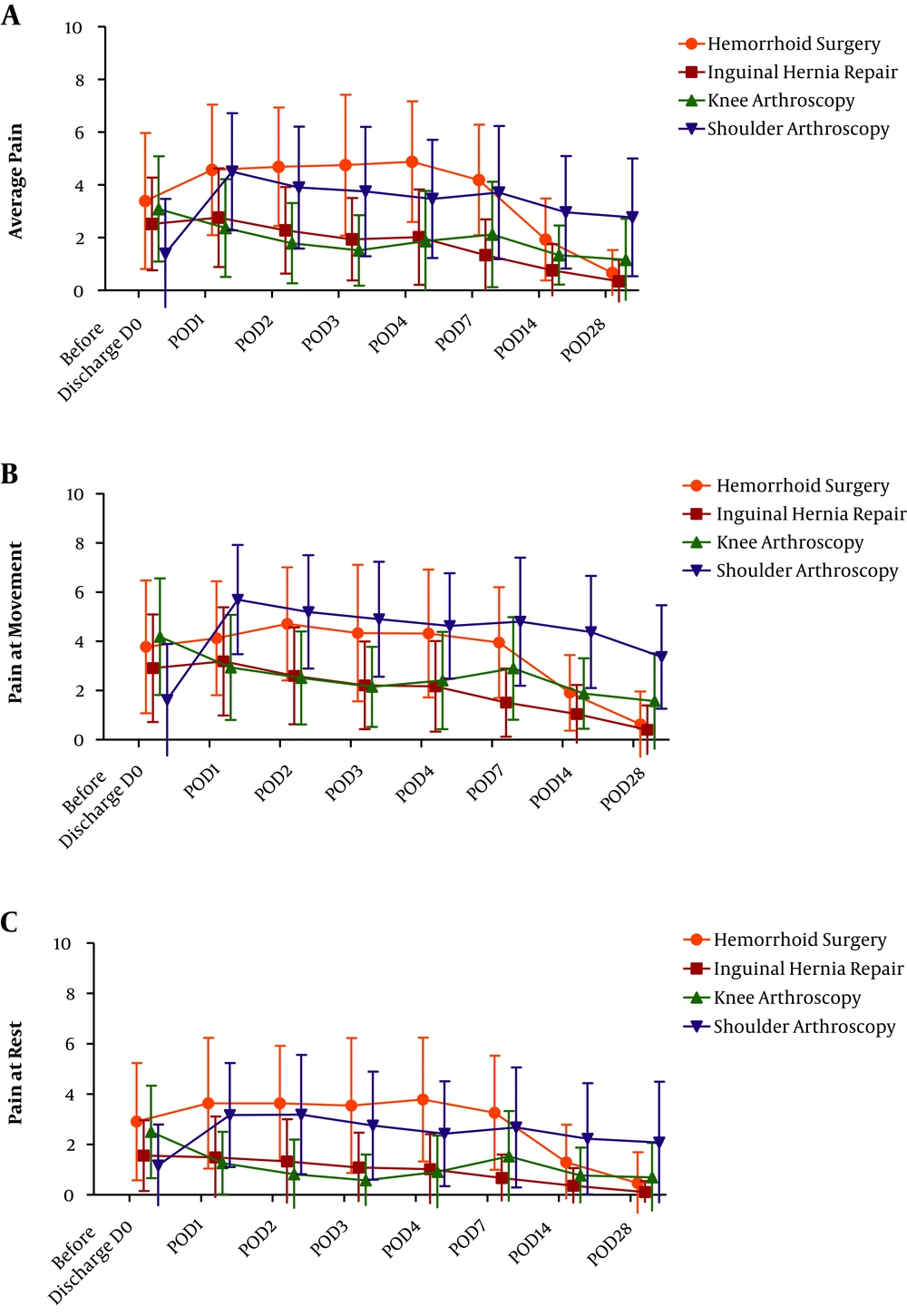
The 4-week pain profile of average pain, pain at movement, and pain at rest for each type of surgery are shown in Figures 3A, 3B, and 3C, respectively. Each type of surgery has a unique 4-week pain profile. For example, median pain scores at movement were highest (NRS > 5, indicating severe pain) during the first 3 PODs after shoulder arthroscopy. Median average pain scores were the highest (NRS > 4) from POD 2 to 7 after hemorrhoid surgery.
Table 2 shows the average pain scores at fixed postoperative time points stratified per type of surgery are presented in. Median average pain scores were above an NRS of 3 during the first postoperative week after the shoulder arthroscopy and even above 4 during the first postoperative week after hemorrhoid surgery. Median average pain scores were below an NRS of 3 during the whole study period after inguinal hernia repair and knee arthroscopy, indicating adequate postoperative pain management. Twenty-six percent of patients undergoing shoulder arthroscopy and hemorrhoid surgery still reported moderate pain up to 1 week after surgery (Table 2). This percentage persisted in patients undergoing shoulder arthroscopy until the second postoperative week. 2% of inguinal hernia repair patients and 6% of knee arthroscopy patients had severe pain in the first postoperative week, while this percentage was 26% in patients undergoing hemorrhoid surgery and shoulder arthroscopy (Table 2).
| Haemorrhoid Surgery (N = 47) | Inguinal Hernia Repair (N = 47) | Knee Arthroscopy (N = 48) | Shoulder Arthroscopy (N = 50) | |
|---|---|---|---|---|
| Average Postoperative Pain Scores | ||||
| Before discharge | 3.00 (1.00, 4.00) | 2.00 (1.00, 4.00) | 3.00 (1.00, 4.00) | 0.00 (0.00, 2.00) |
| POD1 | 5.00 (2.25, 6.00) | 2.00 (1.00, 4.00) | 2.00 (1.00, 4.00) | 4.50 (3.00, 5.25) |
| POD2 | 5.00 (3.00, 6.00) | 2.00 (1.00, 3.00) | 2.00 (1.00, 3.00) | 4.00 (2.00, 5.00) |
| POD3 | 5.00 (2.75, 7.00) | 1.50 (1.00, 3.00) | 2.00 (1.00, 2.50) | 3.00 (1.00, 5.50) |
| POD4 | 5.00 (3.00, 7.00) | 1.00 (1.00, 3.00) | 1.00 (0.75, 3.25) | 3.50 (2.00, 5.00) |
| POD7 | 4.00 (3.00, 6.00) | 1.00 (0.00, 2.00) | 2.00 (1.00, 4.00) | 4.00 (1.50, 5.50) |
| POD14 | 2.00 (1.00, 3.00) | 0.50 (0.00, 1.00) | 1.00 (1.00, 2.00) | 3.00 (1.00, 4.00) |
| POD28 | 0.00 (0.00, 1.00) | 0.00 (0.00, 0.00) | 1.00 (0.00, 2.00) | 2.00 (1.00, 3.75) |
| Moderate Postoperative Pain Scores | ||||
| Before discharge | 8 (17.0) | 10 (21.2) | 13 (27.0) | 6 (12.0) |
| POD1 | 13 (27.6) | 10 (21.2) | 7 (14.5) | 22 (44.0) |
| POD2 | 13 (27.6) | 9 (19.1) | 6 (12.5) | 15 (30.0) |
| POD3 | 12 (25.5) | 4 (8.5) | 4 (8.3) | 11 (22.0) |
| POD4 | 14 (29.7) | 7 (14.8) | 8 (16.6) | 14 (28.0) |
| POD7 | 12 (25.5) | 2 (4.2) | 8 (16.6) | 13 (26.0) |
| POD14 | 4 (8.5) | 1 (2.1) | 2 (4.1) | 13 (26.0) |
| POD28 | 0 (0.0) | 1 (2.1) | 2 (4.1) | 5 (10.0) |
| Severe Postoperative Pain Scores | ||||
| Before discharge | 10 (21.2) | 2 (4.2) | 5 (10.4) | 3 (6.0) |
| POD1 | 16 (34.0) | 5 (10.6) | 3 (6.2) | 14 (28.0) |
| POD2 | 20 (42.5) | 2 (4.2) | 1 (2.0) | 10 (20.0) |
| POD3 | 18 (38.2) | 2 (4.2) | 0 (0.0) | 13 (26.0) |
| POD4 | 17 (36.1) | 1 (2.1) | 2 (4.1) | 9 (18.0) |
| POD7 | 12 (25.5) | 1 (2.1) | 3 (6.2) | 13 (26.0) |
| POD14 | 1 (2.1) | 0 (0.0) | 0 (0.0) | 4 (8.0) |
| POD28 | 0 (0.0) | 0 (0.0) | 2 (4.1) | 6 (12.0) |
aValues are presented as median (25th - 75th percentile) or as numbers (%)
From a total of 191 patients, 47 (24.61%) did not use the MP/IP as prescribed: 11 patients (5.76%) were non-adherent, and 36 patients (18.85%) were partially adherent. Although a few more non-adhering patients in the MP group was observed (29 patients versus 18 patients of the control group) [χ2 (1) = 3.569, P = 0.059], no significant differences were seen between both groups.
There were significantly more female patients in the partial/no adherence group than the full adherence group. Moreover, patients in the partial/no adherence group reported significantly higher baseline FRI values for pain and interference with social activity. Other baseline characteristics showed no significant differences between both groups (Table 3).
| Patient Characteristics | Partial/No Adherence (N = 47) | Full Adherence (N = 144) | P Value |
|---|---|---|---|
| Age (years) | 48.00 (39.00 - 53.75) | 51.00 (43.25 - 58.00) | 0.209 |
| Gender (m/f) | 24/23 (51.06/48.94) | 105/39 (72.92/27.08) | 0.005b |
| Profession | 0.917 | ||
| Unemployed | 14 (29.79) | 45 (31.25) | |
| Employed | 32 (68.09) | 99 (68.75) | |
| Missing (N = 5) | 1 (2.13) | 0 (0.00) | |
| Education | 0.351 | ||
| Primary/junior secondary | 9 (19.15) | 36 (25.00) | |
| Higher secondary | 19 (40.43) | 65 (45.14) | |
| Tertiary | 19 (40.43) | 42 (29.67) | |
| Missing (N = 5) | 0 (0.00) | 1 (0.69) | |
| Short-term surgical fear | 17.00 (8.00 - 26.00) | 11.00 (5.00 - 19.00) | 0.108 |
| Long-term surgical fear | 6.00 (3.00 - 12.00) | 8.00 (3.00 - 15.50) | 0.059 |
| Baseline FRI | |||
| Pain and social activity | 23.00 (10.25 - 37.50) | 11.00 (4.00 - 26.00) | 0.024b |
| Lower limb activity | 1.50 (0.00 - 14.75) | 4.00 (0.00 - 12.75) | 0.139 |
| General physical activity | 0.00 (0.00 - 7.50) | 2.00 (0.00 - 8.00) | 0.696 |
| Preoperative pain | 4.50 (0.25 - 7.00) | 3.00 (0.00 - 6.00) | 0.085 |
| Impact pain on daily life | 4.00 (0.00 - 7.00) | 2.00 (0.00 - 6.00) | 0.221 |
| Expected pain | 5.20 (2.68) | 5.22 (2.36) | 0.944 |
aData are depicted as mean (SD), median (25th - 75th percentile) or as absolute numbers (%).
bP value ≤ 0.05.
The main reason for patients not adhering to the treatment schedule was the occurrence of side effects, such as nausea, pyrosis, and tiredness (n = 25). Furthermore, 11 patients stopped taking their MP/IP due to no pain on POD 1, 2, and/or 3. Other reasons for not adhering to MP/IP schedule included personal reasons (n = 4), fear of taking to much medication (n = 4), hospitalization (n = 3), excessive pain (n = 2), forgotten (n = 1), the surgeon’s instructions to stop their medication (n = 2), and thinking that medication is unhealthy (n = 1).
On postoperative day 1, 21.4% of the non-adherence group and 31.2% of the adherence group reported the intake of tramadol. On postoperative day 2, it decreased to 9% in the non-adherence group compared to 24.6% in the adherence group. On postoperative day 3, 14.2% of patients in the non-adherence group and 15% in the adherence group reported the intake of rescue mediation. On postoperative day 4, 7% in the non-adherence, and 13% in the adherence group reported the intake of tramadol.
Overall, the patient satisfaction with MP/IP was significantly higher in the adherence group than the group of patients who were not or partially adherent (9 (8, 10) vs. 8 (6, 9.25), P = 0.02).
5. Discussion
In this secondary analysis of a prospective, randomized controlled trial, we investigated the 4-week pain profile of average pain, pain at movement, and pain at rest after 4 types of painful ambulatory surgery.
The results of the present study suggested that the 4-week pain profile and recovery was different depending on the type of surgery.
Median average pain scores were above an NRS of 3 during the first postoperative week after shoulder arthroscopy and even above 4 during the first postoperative week after hemorrhoid surgery. More than 26% of patients undergoing shoulder arthroscopy and hemorrhoid surgery reported moderate and severe pain in the first postoperative week. Furthermore, this level of moderate pain proceeded in the second postoperative week in patients undergoing shoulder arthroscopy while median average pain scores were below an NRS of 3 during the whole study period after inguinal hernia repair and knee arthroscopy. These results indicated inadequate postoperative pain management in patients undergoing shoulder arthroscopy and hemorrhoid surgery and are in line with those of previous studies. Ceulemans et al. concluded that patients undergoing hemorrhoid surgery still suffer from moderate postoperative pain in the first postoperative week, despite multimodal analgesic treatment (22). Carvajal Lopez et al. even report moderate postoperative pain up till POD9 after hemorrhoid surgery (23), confirming the need for a longer follow-up period after ambulant surgery. A promising new tool to optimize the follow-up of patients undergoing ambulant surgery was e-health, defined as the use of information and communication technology for health. It has been shown that a systematic follow-up with a smartphone-based assessment may increase the recovery of patients after the ambulant surgery (24). Further research may include personal e-health interventions at home that are taken as a result of alarm signals from patient information, which may reduce the average postoperative pain after a painful day surgery in the future.
The second objective if the present study was to assess the prevalence and reasons for patient non-adherence and partial adherence to a predefined treatment schedule after ambulant surgery. Despite clear oral and written instructions, 24.61% of all patients did not adhere to MP/IP, 5.76% of whom never correctly followed the medication schedule, and 18.85% did not adhere to MP/IP for one or two PODs. The reasons for not adhering to their MP/IP are in most cases, intentional with patients who are afraid of unwanted side effects and those fearlessly do not adhere to the treatment schedule. Furthermore, 3 patients were afraid to take too much medication and 1 patient did not want to take medication because he or she thought this was unhealthy. Only did one patient forget his medication, which was considered to be an unintentional reason for being non-adherent. We also found that women and patients with high baseline levels for pain and pain interference with social activities were underrepresented in the full-adherence group. Furthermore, patients in the full adherence group were overall more satisfied with their medication than the non-adherence/partial adherence group, which was in line with our previously published results (14). Recently, we published the results of a prospective cohort study (n = 1248) assessing the prevalence of adherence to a treatment schedule for pain after ambulant surgery (14). We demonstrated a prevalence of respectively 21.60% and 20.00% of non-adherence and partial adherence to the treatment schedule after ambulant surgery (14). Booysen et al. reported 43.3% of patients undergoing day-case orthopedic surgery being non-adherent to their prescribed medication evaluated by self-reported pill counts (25), while others report 27% of patients being non-adherent with their analgesia after day-case surgery (26). Hence, the prevalence of partial and non-adherence in the present study was remarkably lower. That might be only due to the inclusion of primarily painful ambulatory surgical procedures in the present trial. Also, the less is the proportion of non-adherent patients, the more will be the average postoperative pain intensity (14, 22).
In some studies, access to postoperative pain medication wasn´t identical. Patients received only a prescription for their pain medication (14). In the present trial, however, all patients were provided with the MP/IP for 4 days together with a treatment schedule and a thorough explanation. As a consequence, there was no need for patients to go to the pharmacy, which would explain the low prevalence of unintentional non-adherence in our trial. Moreover, pleasant communication via oral and written instructions is still important for good adherence (27, 28). Unlike the reported correlation between female gender and non-adherence, we demonstrated a positive association between male gender and non-adherence in a previous study (14). This apparent paradox might be explained by the inclusion of different types of surgery in two studies. For example, the inclusion of less painful scrotal surgery in the former study might have inflated the proportion of men in the non-adherence group. This statement supports the fact that gender has deviated from the ultimate model of logistic regression, indicating that postoperative pain is less likely to be a major predictor of adherence to pain medications as well as the short duration of action (14).
The present study faced several limitations. Firstly, this trial was not powered for secondary outcomes. Therefore, no firm conclusions could be drawn regarding the prevalence and predictors of patient non-adherence to pain medication. Secondly, patients had to assess their non-adherence to their study medication by themselves. Self-report was a subjective method to underestimate non-adherence (14, 29). Thirdly, patients were assessed at fixed time-points through telephone follow-up which may have been partly considered as an adherence intervention. Indeed, this method may have influenced the patients’ behavior regarding medication adherence and therefore, may have biased our results.
Further research is required to focus on different types of ambulatory surgery, each of which has its unique pain profile. Therefore, it be added to a better postoperative treatment plan after surgery. It is important to evaluate the adherence of patients undergoing ambulatory surgery in a standardized manner via e-health interventions and tele monitoring-based medication boxes.
5.1. Conclusion
Our results suggested that different ambulant surgeries have their own unprecedented postoperative pain trajectory. Therefore, new strategies should be developed for the treatment of pain at home, particularly after ambulatory arthroscopic shoulder surgery, and hemorrhoid surgery. If the patients are provided with a multimodal analgesic home kit together with clear verbal and written instructions and intensive follow-up, the patient adherence will be likely.