1. Background
Postoperative cognitive disorders and delirium are common in the old hospitalized patients, especially after major surgeries, leading to higher mortality and morbidity rates. The prevalence of femoral and pelvic fractures in the elderly is high; according to a health survey result, 320,000 admissions due to hip fractures occur annually in the United States (1-3). All surgeries cause some stress in the elderly, and it will be sufficient to disturb the physiological and psychological balance in these patients. Postoperative delirium is one of the most common complications among hospitalized elderly patients, especially in those undergoing orthopedic surgery (3-6). The prevalence of delirium in patients undergoing pelvic surgery has been reported to be up to 53.3% (3). In the study of Holly et al. (7), delirium levels in people over 65y reached 62%. This complication often occurs 2 - 5 days after surgery in patients with hip fracture (8).
Delirium progression in the hospital is associated with increased mortality, length of stay, dependence on others, hospital-acquired complications, medical costs, and sometimes permanent cognitive impairment. Delirium is also a predictor of treatment failure or delay in functional recovery in patients with hip fractures (3, 7). There are various theories regarding the pathophysiology of delirium, including metabolic encephalopathy, drug poisoning (especially anticholinergics), hypoglycemia, stress, surgery and increased corticosteroids induced by it, hypotension, preoperative hypoxia, type of anesthesia, sleep deprivation, pain, electrolyte imbalance, old age, as well as hearing and visual disorders (9-13). The mortality rate of these patients is between 10% to 65%, which is equal to the risk of acute myocardial infarction and sepsis (7-9).
Therefore, due to the high prevalence of this complication in patients undergoing hip surgery, high morbidity and mortality rate, hospital-acquired complications due to prolonged hospital stay, economic burden, and also given that there are conflicting results regarding the impact of general or regional anesthesia on delirium and early cognitive disorders in previous studies (14, 15).
2. Objectives
This study aimed to compare the effect of general and spinal anesthesia on the incidence of postoperative delirium and POCD in elderly candidates for surgery due to hip fracture.
3. Methods
The present study was a single-blinded non-randomized clinical trial (RCT). After approving the study protocol by the Ethics Committee (code of ethics: IR. IUMS-FMD.REC1396.9511174001) and by the Iranian Clinical Trial Registration Center (no.: IRCT20121107011398N13), a total number of 108 patients including men and women over the age of 50 years, with the diagnosis of proximal femoral bone fracture who were scheduled for open fixation surgery, were enrolled in the study. Exclusion criteria were: Preoperative cognitive impairment, significant auditory impairment, alcoholism, and drug abuse, American society of anesthesiologists physical status (ASA-PS) > III, acid-base and electrolyte abnormalities, patient’s dissatisfaction, a history of similar surgery in the past month, history of a recent cerebrovascular accident as well as taking psychotropic drugs and benzodiazepines in the week before or inadvertently after surgery.
Mini-Mental State examination (MMSE) and Wechsler tests were used to evaluate postoperative delirium and POCD, both of which were used once before surgery to assess the baseline cognitive status of patients, and three times after surgery i.e., in three successive days. The MMSE test can measure patients’ orientation to time and place, as well as the patient’s attention, memory, and computing power (16). Wechsler’s test is a set of intelligence tests used to assess the patient’s verbal and nonverbal cognition and the capacity and ability of the patient’s overall intelligence and cognitive ability (17).
The primary outcome of this study was POCD, and the secondary outcome was postoperative delirium. Delirium was diagnosed using DSM-IV criteria, and POCD diagnosis was performed using patient-acquired scores from MMSE and Wechsler tests. A decrease of up to 2 points in these tests was considered as mild cognitive impairment, and a decrease of more than 2 points in the postoperative phase as compared to preoperative values was considered as severe cognitive impairment (delirium equivalent).
After obtaining informed consent, the patients were divided into two groups: general (GA) or spinal (SA) anesthesia. The type of anesthesia was selected by an anesthesiologist who was unaware of the study protocol. In the GA group after routine monitoring (ECG, NIBP, SPO2, ET-Co2, BT), for premedication, fentanyl 2 µg/kg and for induction of anesthesia, lidocaine 1 mg/kg, propofol 1.5 mg/kg, and cisatracurium 0.2 mg/kg body weight was used. The patients were then intubated, and for maintenance of anesthesia, propofol 50 - 150 µg/kg/min was infused. Cisatracurium 0.05 mg/kg every 30 min and fentanyl 50 µg every hour was repeated. At the end of the surgery, the neuromuscular block was reversed with 40 µg/kg of neostigmine and 20 µg/kg of atropine, and the patients were extubated according to the clinical criteria.
In the spinal anesthesia group, 12.5 - 15 mg hypertonic bupivacaine plus 25 µg fentanyl in the sitting position were used for spinal anesthesia. In some patients (6 cases), the epidural catheter had been fixed in the L2-L3 before doing spinal anesthesia. Benzodiazepine was not used in any of the study group members during the operation and postoperative phase. In order to control the postoperative pain, 1gr of paracetamol was infused at the end of the operation, and 3 g was perfused with a patient-controlled analgesia pump.
Patients’ level of education, drug history, and preoperative laboratory tests, including the plasma hematocrit, plasma glucose, and serum electrolytes, were recorded. The type of surgery, duration of operation and anesthesia, mean intraoperative blood pressure, the blood loss during operation, amount of fluid administered, and in case of transfusion, the type and amount of the blood products used were recorded as well.
3.1. Sample Size Determination and Data Analysis Method
A reduction of POCD incidence from 40% to 15% was considered clinically significant. Power analysis was performed using an online calculator available from the University of British Columbia (Vancouver, BC, Canada) considering α = 0.05 with a power (β) of 80 percent. The sample size was determined to be a minimum of 47 patients in each group. Data were analyzed using SPSS-V22 software. Qualitative variables were reported by relative frequency, percentage, and quantitative variables using mean and standard deviation. Independent t-test, chi-square, Fisher exact test, and Mann-Whitney test were used to examine the significance of the variables. The level of significance was set at 0.05.
4. Results
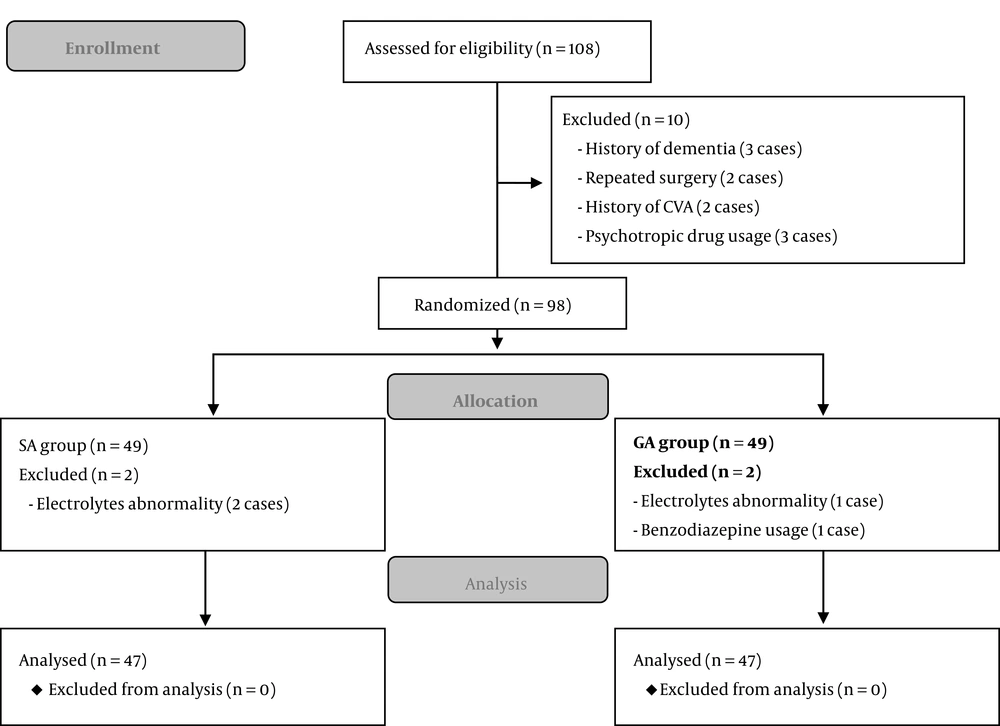
A total of 108 patients were enrolled in the study, of which 14 were excluded because of different reasons, and the final data from 94 patients were analyzed (Figure 1).
Patients were similar in the two study groups in terms of demographic data (Table 1). There was no significant difference in terms of the ASA-PS (P = 0.324), and also educational backgrounds between the study groups. The mean duration of operation in the GA and SA groups were 3.43 ± 0.53 hours and 3.27 ± 0.43 hours, respectively, and it was longer in the GA group (P = 0.031). The amount of bleeding was comparable between the groups, 414.9 ± 265 ml in the GA group versus 416.4 ± 259 in RA (P = 0.978). Ten patients in each group were transferred to the ICU after surgery.
| Variables | Study Groups | Total | P Value | |
|---|---|---|---|---|
| GA | SA | |||
| Sex | 0.063 | |||
| Male | 27 | 18 | 45 | |
| Female | 20 | 29 | 49 | |
| ASA class | 0.324 | |||
| 1 | 16 | 23 | 39 | |
| 2 | 28 | 21 | 49 | |
| 3 | 3 | 3 | 6 | |
| Education level | NSa | |||
| Illiterate | 4 | 0 | 4 | |
| Elementary | 2 | 10 | 12 | |
| High school | 30 | 22 | 52 | |
| Diploma | 7 | 12 | 19 | |
| Bachelor’s | 4 | 3 | 7 | 0.131 |
| Age, y | 68.06 | 64.48 | 67.12 | |
Abbreviations: GA, general anesthesia; SA, spinal anesthesia.
aNon-significant.
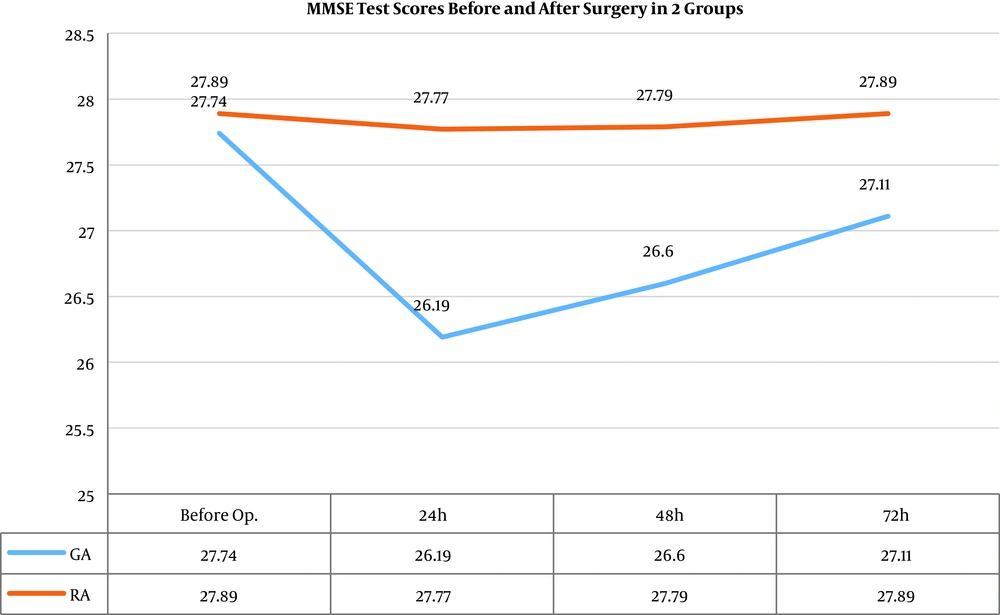
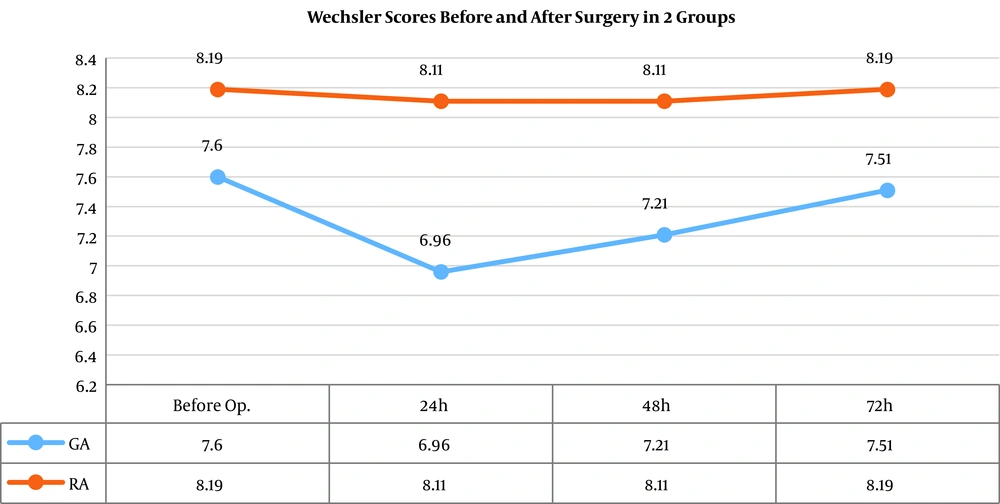
The results of MMSE tests showed that the mean scores of the two groups were similar preoperatively (P = 0.765). However, a significant difference in the mean scores was observed in the postoperative phase at 24 and 48 hours, that is, the scores were significantly lower in GA group than those in SA group. On the third day (72 hours after surgery), these variables did not show a significant difference between the two groups (Figure 2). The comparison of the Wechsler test in (Figure 3) shows that the mean value of this score on the first postoperative day was significantly lower in the GA group than in the spinal group (P value = 0.029), whereas in the preoperative stage, second and third postoperative day, there were no significant differences between the study groups.
The overall prevalence of cognitive disorders in the two groups was 17.02% (n = 16). The drops of MMSE test scores were at least 1 point and a maximum of 17 points, with a mean of 4.19 points on the first day and 2.94 points on the second day after surgery. Given that MMSE and Wechsler scores were more than 2 points in the first 48 hours, the severity of perioperative neurocognitive disorders (PND) in most patients (14 out of 16) can be classified as major. The incidence of delirium and POCD was significantly different between GA and SA groups, 14 patients (29.7%), and only 2 patients (4.25%), respectively (P = 0.001).
Based on the results, there was a significant relationship between age and incidence of POCD. The mean age of patients with PND was 67.9 years and the mean age of non-PND patients was 62.2 years (P = 0.048). There was no significant relationship between intraoperative hemorrhage, fluid intake, and operation time with the delirium and POCD (Table 2).
| POCD | Numbers | Values | P Value | |
|---|---|---|---|---|
| Age, y | No | 78 | 62.25 ± 10.608 | 0.048 |
| Yes | 16 | 67.91 ± 7.646 | ||
| Bleeding, cc | No | 78 | 402.18 ± 232.412 | 0.272 |
| Yes | 16 | 481.25 ± 374.110 | ||
| Fluid intake, L | No | 78 | 3.02 ± 0.42 | 0.960 |
| Yes | 16 | 3.03 ± 0.28 | ||
| Operation time, h | No | 78 | 3.351 ± 0.4840 | 0.955 |
| Yes | 16 | 3.344 ± 0.5072 |
Abbreviation: POCD, postoperative cognitive disorders.
aValues are expressed as mean ± SD.
The results also showed that there was a significant relationship between gender, educational level, and ASA class of patients with cognitive impairment occurring postoperatively (Table 3). Increased educational attainment decreased the probability of delirium and POCD (P = 0.034). The results also showed that the rate of cognitive disorders in men was significantly higher than in women (P = 0.026).
| Variables | POCD Number | P Value | |
|---|---|---|---|
| No | Yes | ||
| Gender | 0.026 | ||
| Male | 34 | 11 | |
| Female | 44 | 5 | |
| ICU-admission | 0.346 | ||
| No | 60 | 14 | |
| Yes | 18 | 2 | |
| Education | 0.018 | ||
| Illiterate | 1 | 3 | |
| Elementary | 12 | 0 | |
| High school | 42 | 9 | |
| Diploma | 16 | 3 | |
| Bachelor | 6 | 1 | |
| ASAclass | 0.034 | ||
| 1 | 36 | 3 | |
| 2 | 36 | 13 | |
| 3 | 6 | 0 | |
Abbreviations: ASA class, American Society of Anesthesiologists physical status; ICU, Intensive Care Unit; POCD, postoperative cognitive disorders.
5. Discussion
Cognitive disorders after surgery and anesthesia have been known for about 100 years but named as POCD since the late 1990s, and many studies are still ongoing. Definitions and nomenclatures are constantly changing, and in the latest issue of Miller (18), perioperative cognitive disorders were named as perioperative neurocognitive disorders (PND), and were divided into two types of mild and severe form, including delirium and dementia (18).
This study showed that the incidence of POCD was 17.02%, which was significantly higher in the GA group. These findings are consistent with the results of other studies that have shown that general anesthesia causes more cognitive disorders than regional anesthesia. There are some other studies declaring that the type of anesthesia has no effect on such disorders. In general, the idea of the effect of anesthesia on the incidence of delirium and cognitive dysfunction remains controversial.
Anwer et al. (19). and colleagues reported that general anesthesia is associated with an increased risk of early cognitive impairment in elderly patients. However, in young patients, there was no relationship between the type of anesthesia and the incidence of POCD. Also, in a review study by Ritchie et al. (20), similar results were reported, but due to the many confounding factors, this relationship regarding late cognitive impairments and dementia cannot be proven.
In a similar study published by Zhang et al. (21), the authors concluded that spinal anesthesia had better results, in terms of verbal communication, and MMSE score, and a reduced prevalence of POCD in elderly patients undergoing orthopedic surgery. In a systematic review by Mason et al. (22), they reported that general anesthesia did not increase the incidence of delirium compared to regional, but did minimally increase the chance of cognitive impairment (odd’s Ratio = 1.34). They have also concluded that regional anesthesia might be preferred in patients at high risk for cognitive impairment (22).
Contrary to the above studies and this study, Silbert et al. (23). concluded that although the prevalence of POCD in patients undergoing general anesthesia was higher than the regional group at day 7 and 3 months postoperatively, but based on statistical analysis, the type of anesthesia does not affect the prevalence of postoperative cognitive disorders; instead, other risk factors such as the type of operation are important. However, the type of surgery selected in this study (lithotripsy) and the duration of follow-up, perhaps justifies the difference between this study with others. In addition, in a study by Tzimas et al. (24) on 70 elderly patients who were candidates for hip fractures, the prevalence of delirium was reported to be 12% in the general anesthesia group and 27% in the spinal group. Finally, they concluded that the choice of anesthesia did not significantly affect the prevalence of POCD in orthopedic elderly patients.
In a study by Olin et al. (25) in elderly patients with major abdominal surgeries, the prevalence of delirium after general anesthesia was reported in approximately 50% of patients, which was higher than the present study. Of course, this difference may be related to the type of surgery and the age of the patients participating in the two studies. The minimum age of participants in that study was 65 years (25).
The prevalence of delirium and cognitive disorders in this study (17.02%) was lower than from several previous studies, such as the studies of Morimoto et al. (26), Biedler et al. (27), and Juliebo et al. (28) with the reported incidence of 25%, 25.8%, and 36.4%, respectively. The following can be pointed out in explaining the causes of this variability: differences in diagnostic tools, the time of evaluation of cognitive functions, the types of surgeries, elective or emergency, major or minor, and the type of anesthesia performed (general or spinal), as well as ecological differences.
Another result of the present study, as we expected, was that the rate of POCD increased with age. There are some other studies with similar results; increasing age is one of the major risk factors for delirium (1, 13). Also, based on the analysis of the present study, there was a significant relationship between gender, educational level, and ASA class of patients with delirium incidence, such that with an increasing educational level, the probability of delirium and POCD decreased. The results of this study also showed that the rate of POCD in men was significantly higher than in women. There was no significant relationship between delirium and intraoperative bleeding, fluid intake, and duration of operation. However, the duration of operation in the GA group was slightly longer than in the RA group, which was not considered clinically significant.
5.1. Limitations of the Study
As predicted and other studies have also emphasized this, we faced serious limitations in this study, the most important of these were: lack of randomization due to ethical considerations, lack of blindness of the patients, the difficulty of engaging and communicating with patients due to their old age, and the problem of learning impact on repeated tests, as well as the short duration of follow-up.
5.2. Conclusions
The results of this study are consistent with many other studies that have shown a relatively higher incidence of POCD in patients undergoing general anesthesia compared to spinal anesthesia. However, given the fact that these abnormalities are limited to 48 hours postoperatively, and patients’ cognitive abilities return to their preoperative status over time, it can be concluded that general anesthesia is associated with early POCD to a greater extent than spinal anesthesia. However, due to the limitations of the study, such as non-randomization and impossibility of blinding, the results of the study cannot be generalized to all patient groups.
Finally, given the results of this study and other beneficial effects that have been proven in previous studies for spinal anesthesia (such as reduced bleeding, and lower thromboembolism risk), this anesthesia technique may be considered as a preferred method to general anesthesia in patients at a high risk of postoperative cognitive impairment.