1. Background
The tourniquet is applied to control bleeding in surgical and pre-hospital settings, and it provides a bloodless operative field (1, 2). Improper application of tourniquet causes serious injuries (3), such as soft tissue damage (4). The incidence and severity of tourniquet-related complications are due to high tourniquet pressure and prolonged tourniquet use (5). Although low inflation pressures are suggested (6), the optimal inflation pressure is not standardized (7). Limb occlusion pressure (LOP) and arterial occlusion pressure (AOP) have been defined as the lowest tourniquet pressure needed to stop the arterial blood flow into the limb distal to the cuff (8, 9). Limb occlusion pressure is determined by gradual cuff inflation until the disappearance of arterial pulse with Doppler flowmeter or pulse oximeter (9). Arterial occlusion pressure can be estimated by the following formula:
AOP = [SBP + 10]/KTP
where SBP is systolic blood pressure, and KTP is the tissue padding coefficient (Appendix 1 in Supplementary File) (10-12).
To adjust the tourniquet pressure, it is recommended to add a safety margin to LOP or AOP (8, 13-15). To our knowledge, one study used the LOP determination method during induced hypotension as a method for determining minimal inflation tourniquet pressure (14), and so far, no publication has compared the AOP estimation method and LOP determination for determining tourniquet inflation pressures for upper limb surgery under induced hypotensive anesthesia. We assumed that the use of the AOP estimation method for determining the minimal inflation tourniquet pressure during induced hypotension may offer a lower effective minimal inflation tourniquet pressure and cause less tourniquet-related complications.
2. Objectives
This research aimed to evaluate the effectiveness of tourniquet pressure using AOP or LOP values during induced hypotension for elective upper limb surgeries. The primary outcome measures were the LOP and AOP levels and tourniquet inflation pressures. Secondary outcome measures were tourniquet efficacy as determined by the surgeon’s rating of tourniquet performance and complications related to tourniquet (e.g., pain or nerve injury).
3. Methods
This randomized, double-blind (the anesthesia resident who recorded the data and the surgical team were unaware of the research protocol), a comparative study was performed at Beni-Suef University Hospital, Egypt, from August to November 2019 after obtaining approval from the local research and ethical committee and registration at (ClinicalTrials.gov ID: NCT04055779; release Date: August 10, 2019). Written informed consents were obtained from 40 male and female patients with ASA physical status I and II, age range 20-50 years who had undergone elective upper limb surgeries (e.g., repair of a cut tendon or excision of simple ganglion) under general anesthesia.
The patients were excluded if they refused to participate, had contraindication for using the tourniquet (e.g., peripheral vascular disease or hemolytic blood disorder), contraindications for induced hypotensive anesthesia (e.g., coronary artery disease, cerebrovascular disease renal impaired kidney function), or were hypertensive patients.
Preoperative investigations (i.e., complete blood count, coagulation profile, liver functions, renal functions, and electrocardiograms) were performed. The study procedure was explained to the patients, and symptoms related to tourniquet complications such as pain, burning, coldness, and numbness were discussed with the patients.
On arrival to the operating room, an intravenous cannula was placed in a vein on the dorsum of the hand that was not operated, and intravenous injection of 10 mg metoclopramide and 40 mg omeprazole was given as premedication. IV fluid infusion was started using a lactated ringer solution. Monitoring was applied (pulse oximetry, 5leads electrocardiography, end-tidal carbon dioxide [ETCO2], and non-invasive arterial blood pressure). After 3 minutes of mask ventilation using oxygen 100%, anesthesia was induced by fentanyl (2 ug/Kg), propofol, and atracurium. Laryngoscopy and endotracheal intubation were performed using an oral cuffed tube lubricated with lidocaine jelly. After induction of anesthesia, a 20-gauge cannula was placed in the radial artery of the non-operative hand under aseptic technique after performing the Modified Allens test for invasive arterial blood pressure monitoring. The mean blood pressure was kept at 60 - 65 mmHg by nitroglycerine (0.5 - 2 μg/kg/min).
Anesthesia was maintained using isoflurane 2% in O2/Air mixture. Ventilation was adjusted to maintain an ETCO2 36 - 40 mmHg. Vital signs (arterial blood pressure, pulse rate, and oxygen saturation) and ETCO2 were observed. After arm exsanguination using Esmarch bandage, the pneumatic tourniquet cuff of 11 cm width was applied.
The patients were divided into two groups using the closed envelope technique for randomization.
- Group (A): The tourniquet inflation pressure was determined based on the AOP, which was calculated by the estimation formula (AOP = [SBP + 10]/KTP) (10) and adding 20 mmHg safety margin (15).
- Group (B): The tourniquet inflation pressure was based on LOP. Using the ultrasound Doppler technique (Philips HD 5 doppler US), the tourniquet was inflated gradually until the arterial pulsations stopped at the side of the operation. This tourniquet pressure was recorded as LOP. The tourniquet cuff was inflated, and the tourniquet inflation pressure was adjusted as recommended by the Association of Perioperative Registered Nurses (AORN) by adding a safety margin of 40 mmHg for pressures below 130 mmHg, 60 mmHg for pressures between 131 mmHg and 190 mmHg, and 80 mmHg for pressures above190 mmHg for adult patients (8).
At the end of the surgery, the tourniquet was deflated; nitroglycerine infusion and inhaled anesthetic were discontinued. After the reversal of muscle relaxation and full recovery, the patients were monitored at the recovery unit.
The following data were recorded by an anesthesiologist unaware of the study protocol to avoid bias in the study:
- Demographic data of the patients (age and gender)
- Arm circumference (Cm)
- Tourniquet application times (minutes)
- Initial and Maximal systolic blood pressure (mmHg)
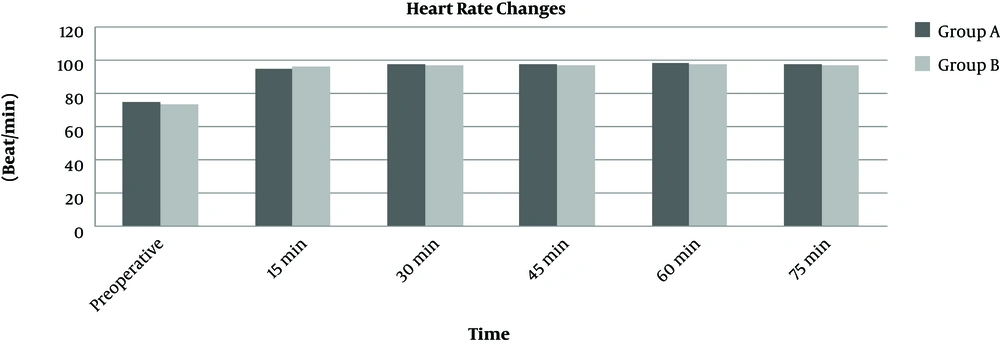
- Heart rate (beat/min) (recorded preoperative, and checked every 5 minutes intraoperative and recorded every 15 minutes)
- Intraoperative fentanyl requirement; (Intraoperative fentanyl requirement;(fentanyl 2 mcg/kg IV was used during induction of anesthesia if the intraoperative heart rate increased by 20% from the base line reading additional 1 mcg/kg was administrated)
- The time needed to estimate the AOP and determine the LOP and set the tourniquet inflation pressure (seconds)
- Primary outcomes: Arterial occlusion pressure (AOP) for patients in group A (mmHg), limb occlusion pressure (LOP) for patients in group B (mmHg), and tourniquet inflation pressure based on AOP or LOP (mmHg).
- Secondary outcome: A surgeon evaluated the effectiveness of tourniquet by the quality of the operative field using a 4-point scale (the same surgeon performed all the operations) (12).
- Patients were examined immediately, 6 h and a day after surgery for signs of tourniquet-related complications such as pain, burning, coldness, and numbness.
3.1. Statistical Analysis
The calculation of sample size was based on the results of Tuncali (14). Assuming 20% reduction in the maximum tourniquet pressure in the groups (primary outcome), 13 patients were required in each group with a power of 90% and α value of 0.05. Twenty patients were included in each group in case of a drop of any patient. The calculation was done using Biostatistics, version 3.01.
Data were presented as mean ± standard deviation (SD) for the quantitative variables and numbers or percentages for the categorical variables. The groups were compared using a t-test or Mann Whitney U test for continuous variables and the chi-square test for categorical variables. Statistical analyses were done by Microsoft office (Excel 2010), and P value less than 0.05 was considered significant.
4. Results
All the patients completed the research, as shown in Figure 1.
The demographic characteristics (e.g., age and gender), upper extremity circumference, the mean tourniquet application times, and intraoperative fentanyl requirements were comparable in both groups and were not significantly different (Table 1).
| Group (A) (N = 20) | Group (B) (N = 20) | P Value | |
|---|---|---|---|
| Age (year) | 25.6 ± 6.9 | 27.2 ± 9.6 | 0.280 |
| Gender (male/female) | 14/6 | 13/7 | |
| Arm circumference (cm) | 27.6 ± 1.6 | 28.3 ± 1.4 | 0.082 |
| Tourniquet time (minutes) | 55 ± 21 | 58 ± 20 | 0.630 |
| Fentanyl requirements (mcg) | 171 ± 16.24 | 175 ± 15.8 | 0.209 |
Less time was recorded for measuring AOP than determining LOP to calculate the minimal inflation pressure (in seconds) for the group (A) than group (B) (62 ± 2 vs. 120 ± 3 for groups A and B, respectively; P < 0.001). The estimated AOP in group (A) was significantly higher than the determined LOP in group B (118 ± 2 mmHg vs. 91 ± 2 mmHg; P < 0.001). Initial tourniquet inflation pressures (mmHg) were not significantly different between the two groups (as the SBP was maintained between 85 - 95 mmHg, the initial tourniquet pressure was sufficient to provide satisfactory surgical field, and there was no need to change the tourniquet pressure throughout the surgery) (Table 2).
| Group (A) (N = 20) | Group (B) (N = 20) | P Value | |
|---|---|---|---|
| Time to estimate AOP or determinate LOP and set the tourniquet cuff pressure (seconds) | 62 ± 15 | 120.8 ± 3.4* | < 0.001 |
| AOP in group A or LOP in group B (mmHg) | 118 ± 2 | 91 ± 2* | < 0.001 |
| Tourniquet inflation pressure (mmHg) | 133 ± 2 | 132 ± 2 | 0.068 |
| Initial SBP (mmHg) | 88.1 ± 3.6 | 89.9 ± 3.5 | 0.061 |
| Maximal SBP (mmHg) | 89.1 ± 2.3 | 90.2 ± 2.9 | 0.093 |
There were no significant differences in initial and maximal SBP between the two groups (Table 2), and their heart rate was comparable (Figure 2).
Tourniquet performance was excellent or good during the operation (Table 3), and tourniquet-related complications were not reported.
| Group (A) (N = 20) | Group (B) (N = 20) | |||||
|---|---|---|---|---|---|---|
| Initial | Middle | End | Initial | Middle | End | |
| Excellent | 19 (95) | 19 (95) | 18 (95) | 18 (90) | 18 (90) | 18 (90) |
| Good | 1 (5) | 1 (5) | 1 (5) | 2 (10) | 2 (10) | 2 (10) |
| Fair | 0 | 0 | 0 | 0 | 0 | 0 |
| Poor | 0 | 0 | 0 | 0 | 0 | 0 |
5. Discussion
This study showed that tourniquet inflation pressure setting based on either AOP estimation or LOP determination methods during induced hypotensive anesthesia provides an equally effective bloodless surgical field in upper limb surgeries without pressure-related tourniquet complications. However, the AOP estimation method causes significant reduced time required for cuff pressure adjustment.
It was reported that increasing inflation pressures lead to more hazards (4). It has been practiced by orthopedic surgeons to apply fixed tourniquet pressure 250 - 300 mmHg or add fixed pressure 100 - 150 mmHg above SAP (16, 17); recently, it was reported that using the minimal effective tourniquet inflation pressure to provide a bloodless surgical field is preferred (18).
Previous studies confirmed that limb circumference and SBP influence inflation pressures (8, 9, 11, 18-20). Some studies have tried to find the best technique to reach the minimal inflation pressure using the AOP estimation formula or LOP determination method. Tuncali et al. (12) used the AOP method to adjust tourniquet pressure for lower limb surgery and found it efficient and useful to reach tourniquet pressures lower than values previously recommended. In another study, Tuncali et al. (15) compared the LOP and AOP methods for setting tourniquet pressure in normotensive adult patients and found both methods were comparable. Kasem et al. (21) concluded that the AOP method was more effective than the mathematical formula of Hong-yun Liu et al. (22) in knee arthroscopy.
In this study, we compared the AOP estimation method and LOP determination for determining the tourniquet inflation pressures under induced hypotensive anesthesia and found a significant difference between the mean estimated AOP and the determined LOP (118 ± 2 mmHg vs. 91 ± 2 mmHg). In both groups, the extremity circumference and the initial SBP of patients were comparable, but since induced hypotensive anesthesia was used, even after adding a safety margin of 40 mmHg for the LOP to determine the tourniquet inflation pressure, according to AORN (8), and 20 mmHg for AOP as described in the study of Tuncali et al. (15), the tourniquet inflation pressure (mmHg) was not significantly different between the two studied groups (133 ± 2 mmHg and 132 ± 2 mmHg for the group (A) and group (B), respectively).
There were no evidence of tourniquet-induced pain, as shown in stable SBP and HR throughout the operation, and no difference in intraoperative fentanyl requirements.
The performance of tourniquet was rated by the surgical team as “excellent” and “good”; Tuncali et al. (14) used LOP-based method with controlled hypotension and reported adequate bloodless surgical field with a tourniquet inflation pressure of 118.2 ± 7.2 mmHg for upper limb surgeries, the explanation for the difference in tourniquet pressure is the safety margin being 20 mmHg in Tuncali et al. (14) study and 40 mmHg in the present study.
In this research, the time required to estimate AOP and set the tourniquet pressure in group A was less than that for group B; (P < 0.001), similar results were reported by Tuncali et al. (15).
The limitation of the present study was the small sample size. Therefore, we recommend trying these techniques on larger numbers of patients in the upper and lower extremities.
Conclusion: Using AOP estimation or LOP determination methods to set the tourniquet inflation pressure with hypotensive anesthesia were comparable in providing effective minimal inflation pressure and satisfactory surgical field for upper extremity surgeries without developing tourniquet-induced complications. However, the LOP determination method requires more time and additional equipment and skills.