1. Background
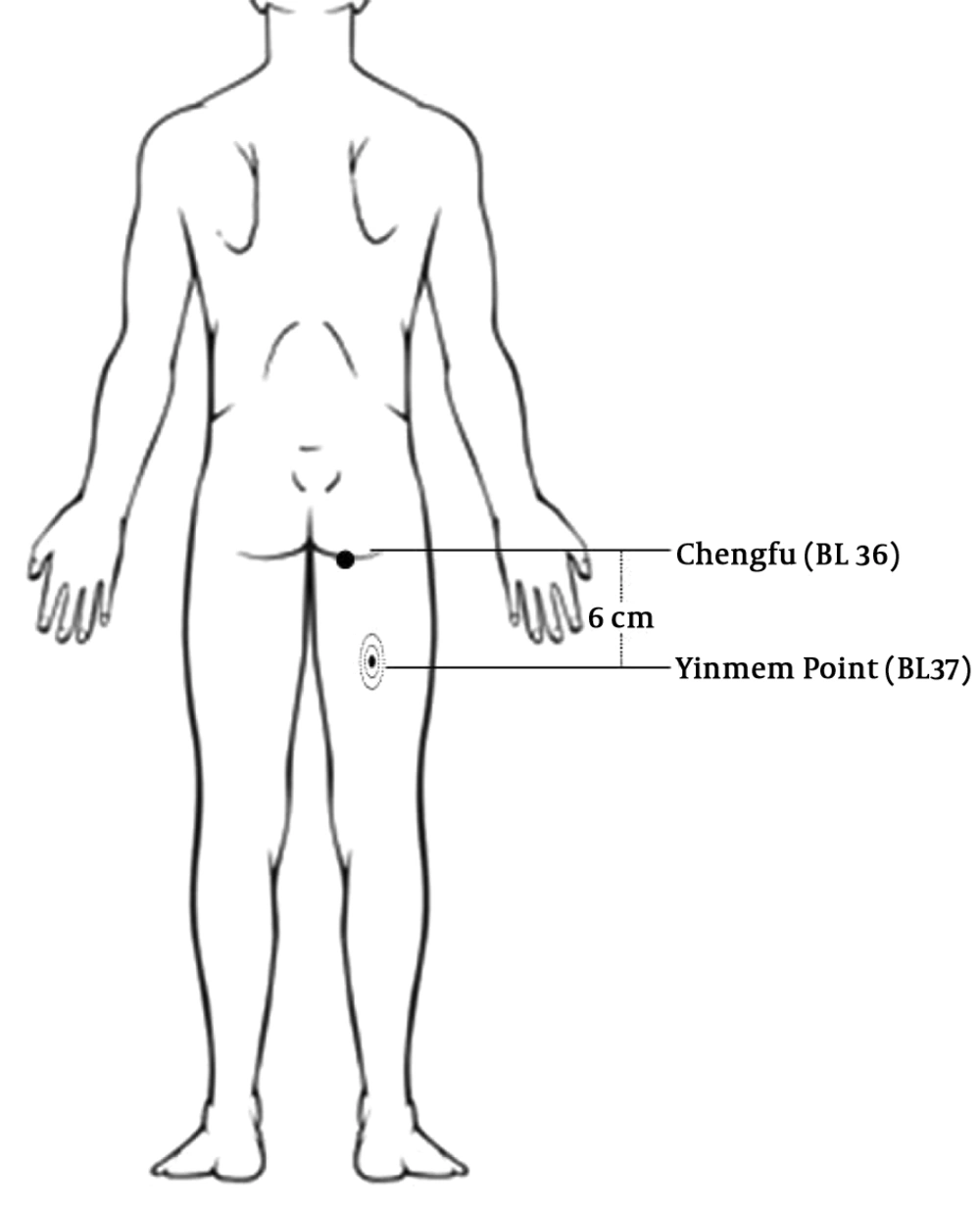
Acute pain following surgery is a major cause of patients’ discomfort. Hence, postoperative pain management is one of the main responsibilities of treating doctors, particularly anesthesiologists. Failing to adequately manage the pain not only is a predictor of prolonged hospitalization (1, 2) but also contributes to many acute and chronic adverse effects. Analgesics are widely used to manage postoperative pain control. Different analgesic methods have been introduced, including oral or IV drugs, regional or neuraxial analgesia, and local infiltration. However, they may cause severe complications (1, 3). Therefore, clinicians often prefer to use drugless pain control modalities or complementary medicine to avoid such complications, including acupuncture, cryoanalgesia, transcutaneous electrical nerve stimulation (TENS), and sport and music therapy (1, 3, 4). These methods are based on transmitting the pain impulses from peripheral receptors to the central nervous system (CNS). In acupuncture, for example, fine needles are inserted at specific points along especial nerves to modify impulse transmission. The Yinmen point (BL37) is an important acupoint, that is located posterior to the thigh (along with sciatic nerve), on the line joining Chengfu (BL 36) and Weizhong (BL 40).
The main mechanisms proposed for pain perception are based on the transmission of the pain to the peripheral receptors (i.e., nociceptors), which are the distal branches of A-delta nerve fibers and C fibers, then to the spinal dorsal root ganglion. The spinothalamic carries pain information to the brain, where the pain stimulus is received, interpreted, and understood. Different regulators in various areas of the CNS influence this process (4). The basic mechanism of pain transmission is decreasing the pain through non-extreme stimulation by activating the pressure-sensitive (thick) nerve fibers Aβ. In turn, severe stimulation leads to the transmission of pain by activating the (average size) nerve fibers Aδ and the (thin) nerve fibers C, which are sensitive to oxygen deprivation.
This is a justification proposed by the gate control theory of pain and can be one of the possible mechanisms to relieve pain. According to this theory, stimulation of small-diameter fibers close to the gate prevents carrying pain information on the dorsal root ganglion. However, the exact reason is not yet known (5). Several studies have focused on the control of the pain by stimulations of and by applying direct pressure on it in some others.
For example, Macgregor et al. investigated the models of pressure on a nerve and concluded that applying pressure with different forces at various times has different effects; also, they argued that the higher the pressure, the more would relieve the pain (6). Stimulation of peripheral nerves can increase the pain threshold. Nevertheless, it’s more effective to alleviate acute clinical pains. The chronic pressure on the sciatic nerve causes hyperalgesia, but acute pressure may attenuate the pain perception in the short term (7). Tuina originated in China, originally termed massage or anqiao, is believed to be one of the earliest methods of Chinses traditional medicine, nearly 2000 years ago. It is a therapeutic modality that utilizes massage (mild mechanical stimulation) applied to certain parts or points (acupuncture points). In China, tuina is widely using to treat sensory dysfunction and health conditions caused by peripheral nerve injury (8), mainly through regulating nerve growth factor and its related receptors in dorsal horn neurons and C fibers in the superficial layers of the spinal cord that promotes repair of the peripheral nerve injury (9). The three points and three methods mean that strumming, kneading manipulation, and point pressing performed in three acupoints (8). The most common sub-methods of tuina work on the three most common acupuncture points on the lower extremity (Yinmen, Chengshan, and Yang-lingquan) to treat peripheral nerve injury. Anatomically the Yinmen acupoint is located on the sciatic nerve trunk (8). The Chengfu is an acupoint located on the sciatic nerve, a few centimeters above the Yinmen acupoint. He et al. (10) showed that applying short-term pressure on the sciatic nerve near the Chengfu point can relieve renal pain. However, applying acupuncture methods to manage postoperative pain has some limitations. First and foremost, to apply pressure on the sciatic nerve in such acupoints, the patient must be placed in a prone position easily and without any risk to the patient or surgical process.
2. Objectives
The current comparative study is conducted on patients who underwent middle ear surgery (tympanoplasty) to assess how pressure on Yinmen point is effective in reducing postoperative pain intensity.
3. Methods
This study is approved by the local institutional ethical committee (code: 1394.443), and written informed consent was obtained from all participants. Besides, it’s also approved by the Iranian Registry of Clinical Trials (IRCT: 201504051772N18). Participants were recruited among all adult patients aged 20 - 60 years who were scheduled for elective tympanoplasty. In total, 100 adult patients who met inclusion criteria were recruited in 12 months. Then, were randomly allocated to two groups of Yinmen and placebo, each with 50 subjects. Those who had background diseases (such as neuropathy, radiculopathy, diabetes mellitus), history of drug abuse, and taking psychotomimetic agents, as well as those who were unable to get prone position, were not allowed to enter this study.
All patients received oxazepam 10 mg orally the night before surgery. Anesthesia was induced intravenously with midazolam 0.02 mg/kg, fentanyl 100 µg, propofol 2 - 3 mg/kg, and atracurium 0.5 mg/kg. Anesthesia was maintained with remifentanil 0.2 - 0.5 µg/kg/min and propofol 50 µg/kg/min infusions, and isoflurane/O2/N2O gas mixture. N2O discontinued 10 - 15 min before new tympanic membrane instillation. All patients received ondansetron 2mg and fentanyl 100 µg, IV, 10 - 20 minutes before ending of surgery. At the end of surgery the remifentanil, propofol, and isoflurane discontinued, and the residual muscular blockage was reversed using neostigmine 2 mg and atropine 1 mg, IV. After reassuring effective respiratory efforts, patients were suctioned and extubated while in deep anesthesia. Then patients were admitted to the post-anesthesia care unit (PACU) for routine care. Afterward, they were discharged to the ward according to the criteria.
On admission to the ward, the pain intensity of patients was measured using the visual analog score (VAS), ranging from 0 to 10. Then, they were asked to take the prone position. Afterward, using a previously prepared randomization list, patients were allocated to Yinmen or placebo groups. Patients of the Yinmen group received 11 - 20 kg pressure on the Yinmen points for 2 minutes, by the researcher herself (Figure 1). While in the placebo group, the researcher kept only a soft skin-fist contact, without applying any pressure. After 2 minutes, patients were requested to lay supine, and the intervention was repeated every 2 hours up to four times. The intensity of the pain was recorded for all patients by a member of the research team who was blinded about the randomization, every hour, up to 8 hours.
For those with a VAS score higher than 4, paracetamol 5 - 15 mg/kg was administered intravenously. For those with resistant pain, meperidine 10 - 20 mg was injected. Nausea and vomiting were treated using ondansetron 2 mg, IV. Data on patients’ demographic, anesthesia, and surgical characteristics, post-operation pain, complication rate, and drug requirements were recorded and compared between the two groups.
3.1. Data Analysis
Data on patients’ demographic, anesthesia, and surgical characteristics, post-operation pain, complication rate, and drug requirements were analyzed and compared using SPSS version 22. The results were expressed as the mean ± SD or frequency (percentage) for parametric and categorical data, respectively. The unpaired student t-test was used to compare parametric data between the two groups. The chi-square or Fisher’s exact tests were used to compare categorical data. The repeated ANOVA test was used to monitor the intensity of the pain within groups. A P value < 0.05 was considered statistically significant.
4. Results
All 100 participants completed the study, and their demographic and perioperative characteristics are shown in Table 1. No significant difference was found concerning the gender, weight, height, and age between the two groups.
| Yinmen Group (N = 50) | Placebo Group (N = 50) | Total (N = 100) | P Value | |
|---|---|---|---|---|
| Male/Female | 17/33 | 14/36 | 31/69 | 0.67 |
| Weight, kg | 70.82 ± 10.65 | 73.44 ± 12.52 | 72.13 ± 11.64 | o.26 |
| Height, cm | 163.30 ± 8.62 | 165.02 ± 8.16 | 164.16 ± 8.40 | 0.31 |
| Age, y | 39.68 ± 10.91 | 38.00 ± 11.69 | 39.30 ± 11.28 | 0.47 |
| Basic MBP, mmHg | 99.77 ± 10.53 | 96.55 ± 11.06 | 97.66 ± 10.80 | 0.31 |
| Basic HR, bpm | 76.92 ± 5.13 | 79.20 ± 7.72 | 78.06 ± 6.62 | 0.09 |
| Anesthesia time, min | 111.30 ± 15.75 | 105.93 ± 12.35 | 108.62 ± 14.34 | 0.06 |
| Basic pain, VAS | 6.32 ± 1.02 | 6.20 ± 0.95 | 6.27 ± 0.99 | 0.54 |
| Total paracetamol consumption, mg/kg | 6.68 ± 2.58 | 10.42 ± 3.87 | 8.55 ± 3.77 | 0.001 |
| Total meperidine consumption, mg/kg | 0.21 ± 0.17 | 0.39 ± 0.23 | 0.30 ± 0.19 | 0.001 |
aValues are expressed as mean ± SD.
The anesthesia time, initial mean arterial blood pressure, and heart rate on admission to the ward were the same between the two groups. Before the intervention, the pain score of both groups was similar (P value 0.54). The total consumption of paracetamol (6.68 ± 2.58 vs. 10.42 ± 3.87 mg/kg) and meperidine (0.21 ± 0.17 vs. 0.39 ± 0.23 mg/kg) was low in the Yinmen group (P value 0.001).
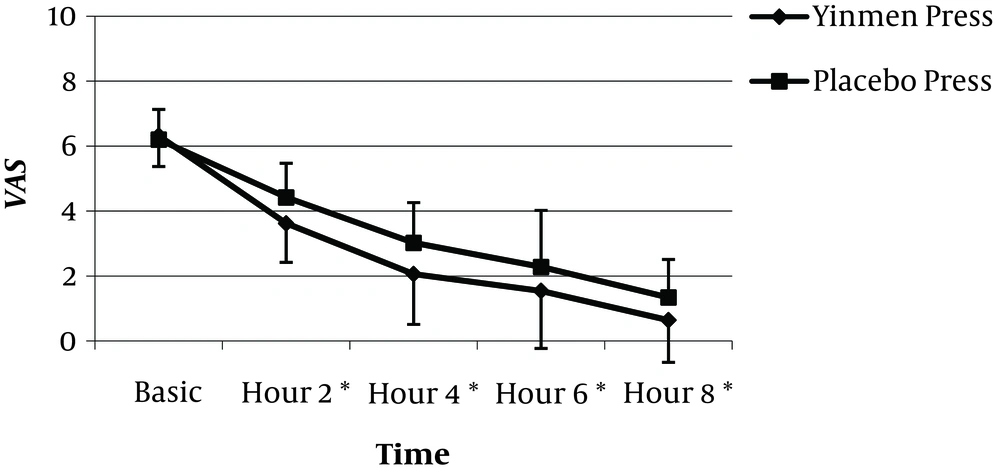
Pain intensity at 2-hour intervals during the first 8-hour after surgery is shown in Figure 2. For all measurements, patients in the Yinmen group had lower pain scores than the placebo.
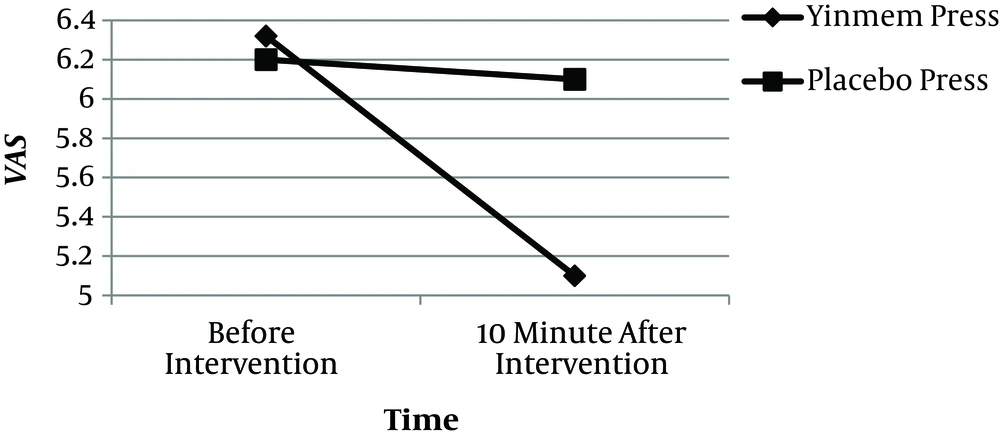
The effect of the true pressure on Yinmen acupoint on the postoperative pain score is shown in Figure 3. In the Yinmen group, 10 minutes after the first intervention, the pain score was significantly low. The ondansetron was used to manage postoperative nausea and vomiting (PONV) in patients with codes 11 and 13 in the Yinmen and placebo groups, respectively (P value 0.81).
5. Discussion
The present study showed that applying short-term pressure on the sciatic nerve at the Yinmen acupoint can decrease the pain after middle ear surgery. In an animal study, Wang et al. reported the inhibitory effect of the pressure on the sciatic nerve on the wide dynamic range (WDR) neurons of the spinal dorsal horn. WDR neurons carry the nociceptive impulses from the spinal cord to the higher cerebral centers (11). We applied a short-term pressure about 11 - 20 kg at the Yinmen acupoint along the sciatic nerve. Compared to the placebo group, patients in the Yinmen group had lower pain scores, measured using the VAS. However, it worth noting that chronic pressure on the sciatic nerve may exacerbate the pain, instead of relieving the pain (12). Chronic pressure may cause sciatic nerve dysfunction. The findings of the present study are consistent with previous studies. Overall, patients in the Yinmen group had lower pain and were more comfortable than those in the placebo group. In a similar study, He et al. (10) applied pressure near the Chengfu acupoint and reported significant pain relief after dental and renal procedures. In another similar study, authors reported significant pain relief among patients at dental, renal neoplastic diseases, and emergency wards (13). Stimulating peripheral nerves increases the pain threshold (9-13). According to the Melzack gate control theory of pain, a non-painful input closes the nerve gates to the painful stimuli. In other words, only a single painful stimulation can enter the ascending pain pathways, and then the gates will be closed (14). So, stimulation of small-diameter fibers results in closure of the gates, and average and small-diameter fibers won’t be stimulated (11).
This theory is suggestive of rapid pain relief in some cases (5, 15). Moreover, electrical stimulation of peripheral nerves leads to inhibitory input to the transmission pathways at the spinal cord level (16). Wang et al., in a study on rats, concluded that applying acute pressure to the sciatic nerve creates a rapid inhibitory effect on the WDR neuronal response to both noxious and innocuous stimulus (11). This can be used as an argument for the analgesic effects of the pressure. As WDR neurons in the spinal cord dorsal horn is the first synaptic relay for afferent, it has an important role in relieving pain. These neurons have a significant effect on modifying noxious input transmission. Staud (17) showed that WDR neurons are the first branch of synapses in dorsal horn neurons, which play an important role in pain transmission; hence, applying pressure on the sciatic nerve can influence (weaken) the transmission of pain messages in these neurons. In the present study, we have probably increased the patients' pain threshold and their comfort by stimulating their thick nerves via pressure.
Yao et al. (18) performed a study on low-frequency stimulation of the sciatic nerve in rats and theorized that the endogenous opioids, those which are released during the pain, may be associated with increased pain threshold, up to 50%. The findings of the present study are in line with several studies and reports which reported that a short-term pressure on the sciatic nerve is associated with increased pain threshold, which in turn leads to pain relief (7, 10, 11, 13, 15, 19). Nevertheless, it worth noting that these studies had significantly different contexts. Based on the findings, the aforementioned maneuver could effectively relieve the pain in adult patients who underwent middle ear surgery. He et al. (10, 13) conducted a similar study on procedures that were provided in dental, renal, neoplastic diseases, and emergency wards. Yao et al. (18) investigated the effect of low-frequency stimulation on the sciatic nerve in rats. The postoperative period after middle ear surgery is a very frustrating period, with the most compliant of the pain. Thus, it seems that postoperative pain management is the main cornerstone of middle ear surgery (20). The Yinmen point (BL37) is an Acupuncture point on the posterior aspect of the upper thigh (along with sciatic nerve), on the line joining Chengfu (BL 36) and Weizhong (BL 40). This point is located on the meridian of the bladder. In traditional Chinese medicine, the acupoint is used to manage edema of the lower part of the body, difficult urination, urinary retention, and low back pain (21).
In modern western medicine, it is believed that acupuncture is primarily based on that acupuncture induces signals in afferent nerves that, in turn, modulates the spinal signal transmission and pain perception in the brain. Based on recent studies, the limbic system in acupuncture medicine. Acupuncture and other related techniques trigger a sequence of events that result in modulation of pain signals processing and release of the neurotransmitters, endogenous opioid-like substances (enkephalin, β-endorphin, and endomorphin), and activation of c-fos within the central nervous system, which inhibits the nociceptive transmission (22). There are theories on the parallels between the influence of acupuncture and the theory of diffuse noxious inhibitory control; acupuncture may act as a part of a generalized stress response or as a result of an individual’s suggestibility (23).
Our study supports this theory, and we can conclude that, based on the findings, applying direct short-term pressure on the sciatic nerves modifies generalized stress response in patients with middle ear surgery, distant enough from the sciatic nerve. Therefore, as an easy-to-use, effective, and safe technique, it plays an important role in managing acute postoperative pain and patients’ need for analgesic drugs.
In the present study, 24% of participants developed PONV, and the maneuver did not intervene with the PONV treatment in both groups. Moreover, several studies have reported that acupuncture methods can attenuate PONV (24, 25). Noroozinia et al. (26) performed acupressure using an elastic wrist band on the Nei-Guan acupuncture point 30 min before spinal anesthesia in candidates of cesarean section. They reported that PONY incidence was reduced from 35.5 to 13.2% (26). According to the best knowledge of the authors, no study is published on the effect of Yinmen acupressure on PONV in middle ear surgery. Thus we couldn’t find any similar study to compare the results.
5.1. Conclusions
Short-term pressure on sciatic nerves at Yinmen acupoint is an effective, safe, and easy to perform method in acute postoperative pain management after middle ear surgery. This maneuver reduces the need for analgesic drugs. The authors recommend investigating its effect on postoperative nausea and vomiting in future studies.