1. Introduction
Shoulder pain is a common disease in adults and may become chronic not only due to the difficult detection of a good treatment strategy (1, 2), but also because of chronic neuroinflammation as it is observed in any osteoarticular disease. It can be determined by the impingement of articular capsule, disease of the rotator cuff, capsulitis, tendinitis, and degenerative disease (3, 4). The management of shoulder pain requires a multimodal approach, including mini-invasive procedures like pulsed radiofrequency (PRF) of the suprascapular nerve, which provides 70% sensory innervation of the shoulder (5, 6). Other techniques like steroid injection and anesthetic blocks have short-term efficacy, while surgical neurectomy causes irreversible paralysis of supraspinatus and infraspinatus muscle.
Pulsed radiofrequency of the suprascapular nerve is a good therapeutic option without damaging motor function, even if the results are not always the same in terms of duration (6-9). This can be due to different factors. First, there are limited published articles with homogeneous populations using the same stimulation parameters. Second, it is not easy to perfectly reach and stimulate small nerves like the suprascapular nerve with a radiofrequency needle. It is quite normal for a pain physician practicing PRF to have really good results or no pain benefit depending on the millimetric positioning of the needle tip, which often cannot be determined clearly. Ultrasonography has helped to reduce this bias by visualizing the suprascapular nerve and targeting it more clearly (10).
Another problem is related to the anatomic constitution of the suprascapular nerve that is targeted conventionally in the suprascapular notch but is divided into two branches, lateral and medial. They have different functions and supply innervation to the posterior supraspinatus and articular branches to the glenohumeral joint capsule (lateral) while the medial trunk provides motor innervation to the anterior region. This anatomical differentiation makes it important to preserve motor function by isolating and stimulating only the lateral part of the nerve.
As said before, ultrasonography may represent good support. Still, the suprascapular nerve is not very easy to be seen, and thus, the problem of correct PRF neuromodulation of the nerve still exists. For this reason, we tried an endoscopic approach to the suprascapular nerve to have an extremely clear vision of the anatomical structures, identify the neural trunk, and be sure of the stimulation field.
2. Case Presentation
The patient was a 63-year-old man, 181 cm tall, and 87 kg weight. Since he was 55-years-old, he had arterial hypertension on treatment. No other chronic or neurological pathologies or previous surgical treatments were reported. He had no allergic history to local anesthetics and no coagulation test abnormalities. His shoulder was painful for more than six months, with a limited range of motion of the arm. The pain was reported to the upper and anterior part of the shoulder, radiating to the biceps. He had 24-h pain exacerbated by the movements of internal and external rotation of the arm, with a very painful spotted area localized in the suprascapular notch zone.
The MRI exam had shown minor subscapularis insertional tendinopathy and acromioclavicular joint hypertrophic osteoarthropathy. The orthopedic surgeon had excluded surgical indications, and suggested physiotherapy, without benefits. The prescribed pharmacological treatment consisted of ibuprofen and acetaminophen daily, with limited results. He had received three intra-articular corticosteroid infiltrations, completely useless. A diagnostic suprascapular nerve block with 3 mL of lidocaine 2% using ultrasonography had shown the complete remission of pain for six hours.
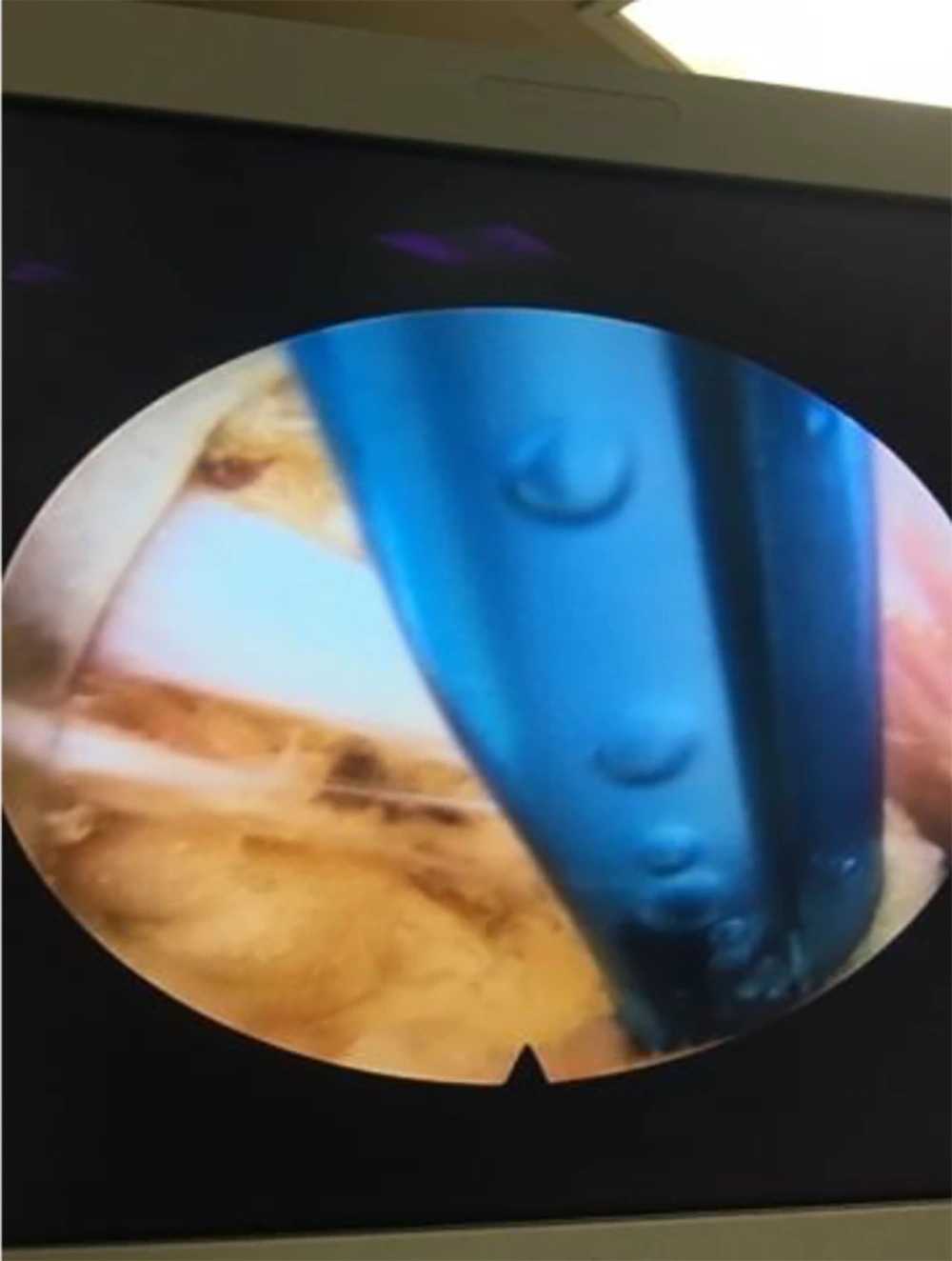
We decided to perform radiofrequency neuromodulation with an endoscopic approach. The patient received local anesthesia with mild sedation (10 mL of mepivacaine 2% injected in the surgical site and continuous iv. infusion of propofol 1.5 mg/kg/h). The procedure was performed using Joimax® endoscopic cannula, with small skin incision and continuous washing using normal saline to perform endoscopy. The point of entrance of the endoscope was identified 3 cm below the suprascapular notch to have plane access to minimize the risk of pleural damage. The visualization of the suprascapular nerve was good, and it was possible to have a clear vision of the nerve path through bone structures. The positioning of the stimulation probe was also clear. The stimulation probe was represented by an electro catheter (VoJager, Alfamed) for suprascapular nerve pulsed stimulation, 40 cm long, with a 1 cm tip stimulating terminal. The catheter is flexible with a rigid metallic guide that was removed before stimulation. The stimulation setting was pulsed radiofrequency (Baylis Medical Co.) as 20-millisecond stimulation, 480-millisecond pause, eight minutes total, 42°C temperature, and 45 Volt impulse power. Even if the nerve was under our eyes, we used electro-stimulation to be sure. We looked after a radiating pain sensation in the anterior part of the shoulder. The test was considered good when radiating pain was generated at 0.3 mA (Figures 1-3).
The monitoring of pain was made using the Visual Analog scale (VAS = 1 - 10) during resting, movement, and sleep, before and six times after the procedure (two weeks, one month, three months, six months, 12 months, and 18 months), as shown in Table 1. At the same time, the Shoulder Pain and Disability index (SPADI) was determined. The SPADI is a 13-item questionnaire to assess pain (five items = 0 - 50 points) and disability (eight items = 0 - 80 points) related to shoulder problems (Table 2).
| VAS | Basal | 15 Days | One Month | Three Months | Six Months | 12 Months | 18 Months |
|---|---|---|---|---|---|---|---|
| Resting | 5 | 3 | 3 | 3 | 3 | 3 | 3 |
| Movement | 9 | 4 | 3 | 4 | 2 | 4 | 4 |
| Sleep | 8 | 3 | 3 | 2 | 2 | 2 | 3 |
| Mean score | 7.33 | 3.33 | 3 | 3 | 2.33 | 3 | 3.33 |
Visual Analog Scale (VAS) Values Before and After the Procedure
| SPADI | Basal | 15 Days | One Month | Three Months | Six Months | 12 Months | 18 Months |
|---|---|---|---|---|---|---|---|
| Pain | 42 | 17 | 14 | 13 | 15 | 12 | 14 |
| Disability | 69 | 25 | 26 | 23 | 25 | 26 | 24 |
| Mean score | 55.5 | 21 | 20 | 18 | 20 | 19 | 19 |
Shoulder Pain and Disability Index Values Before and After the Procedure
The procedure lasted 45 min. It was conducted without side effects. The patient was discharged from the hospital 24 h after the surgery. The results of VAS and SPADI are summarized in Table 1 and Table 2, respectively. The reduction of VAS at rest (from 5 to 3), during movement (from 9 to 4), and at night (from 8 to 3) during the whole follow-up period made the patient satisfied. Also, the SPADI showed a significant decrease in pain (from 42 to 14) and disability (from 69 to 24) during the whole follow-up period.
3. Discussion
Pulsed radiofrequency is a good treatment option for shoulder pain in patients with no surgical indications (8-10). Its long-term efficacy is still not clear and in any case, it does not last longer than 12 - 18 months (5, 7). Pharmacological treatment is not always efficacious and may have side effects, especially in long-term treatment, even in the case of prescribing NSAIDs with long-lasting clinical use and good safety profile (11-13). Physiotherapy seems somewhat interesting, as much as educational programs are presented, especially for working adults (14, 15).
The use of endoscopy to detect the nerve trunk can be a good option to increase the positive results of PRF. This case report should be followed by a larger number of cases, possibly in a randomized clinical trial. In this case report, the patient showed very good and stable results for 18 months in terms of pain reduction and shoulder functionality. The technique requires a good knowledge of anatomical landmarks and endoscopic instruments; in our opinion, it can be particularly indicated in patients that had good pain relief with percutaneous PRF in need of repeated procedures.