1. Background
A pneumatic thigh tourniquet is routinely used during below-knee orthopedic surgery to provide a bloodless surgical field and decrease intraoperative blood loss. Tourniquet use is associated with some adverse effects. Pain and discomfort of the thigh are a common complication of tourniquet application during regional anesthesia. The patient may feel a poorly localized dull or burning pain in the area of the tourniquet, which its intensity gradually increases until it becomes severe (1). The exact cause of tourniquet pain is unclear. The combined effects of nerve ischemia and compression of the tissues under the tourniquet may be the main sources of the pain (2).
The numerous physiological advantages of ultrasound-guided peripheral nerve blocks (PNB) have made them a good substitute for general or neuraxial anesthesia. However, insufficient suppression of tourniquet-related pain has limited their routine use during lower limb surgeries. The sciatic nerve block in the popliteal fossa can be used as a sole anesthetic method for foot or ankle procedures when a thigh tourniquet is not placed (3). It has been suggested that if needed, adding the femoral block to the popliteal block is effective in tolerating the thigh pain (4, 5). However, the femoral block is insufficient to attenuate thigh pain (6), probably because it only anesthetizes the anteromedial surface of the thigh. The anterolateral part is supplied by the fully sensory lateral femoral cutaneous nerve (LFCN) (L2-L3) (7), which is said to conducts the pain of tourniquet rather than the surgical noxious stimulus (8). However, a single blockade of LFCN has been shown to have little effect on reducing thigh tourniquet pain (9). Alternatively, the combination of LFCN and femoral blocks may provide better relief of the tourniquet pain (10). However, to our knowledge, few studies have been published on this topic.
2. Objectives
Thus, the purpose of this study was to determine the effect of the combined block of LFCN and femoral nerve (FN) on tourniquet tolerance during foot or ankle orthopedic surgeries. We compared it with spinal anesthesia as it is the routine method of regional anesthesia in lower limb surgery (11). The primary outcome of the study was the intraoperative severity of tourniquet pain. The secondary outcomes were as follows: time to perform the block, surgical anesthetic effect time, and total doses of analgesics given intraoperatively. We hypothesized that the combined LFCN and femoral nerve block with a popliteal block would effectively attenuate tourniquet pain.
3. Methods
This prospective, single-blind, randomized, controlled clinical trial was registered at the Iranian Registry of Clinical Trials (code: IRCT20131108015322N3). The study was approved by the Ethics Committee of Shahid Beheshti University of Medical Sciences, Tehran, Iran (ethics code: IR.SBMU.MSP.REC.1398.058) and conducted between June 2018 and February 2019. Sixty American Society of Anesthesiologists’ physical status I-II patients, scheduled for the elective unilateral orthopedic surgery on ankle or foot using a pneumatic thigh tourniquet, were included in the study after obtaining the informed consent. They were randomly divided into two equal groups of spinal anesthesia (SA) and peripheral nerve block (PNB) using a random numbers table. Patients with sensitivity to the local anesthetics, the age of less than 14 and more than 80 years, coagulation disorders, opium addiction, infection at the block site, previous femoral or popliteal bypass surgery, body mass index > 30, sickle cell anemia, lack of cooperation, and anticipated tourniquet inflation time of less than 30 min were excluded from the study.
In the operating room, eligible patients were allocated to one of the two groups by chance by a staff not involved in the study. Monitoring consisted of the electrocardiogram, pulse oximetry, and noninvasive blood pressure. All cases received 1 mg intravenous midazolam prior to the procedure. In the SA group, the patient lied down on the side to be operated. Then, 3 cc (15 mg) of 0.5% hyperbaric bupivacaine was injected intrathecally at the L3-L4 level using a 25 G Quincke spinal needle by a senior anesthesiology resident. In the PNB group, the block of the FN, LFCN, and sciatic nerve in the popliteal fossa was performed using ultrasound guidance (SonoSite S-Nerve, Bothell, WA, USA) and a 6 - 13 MHz linear transducer and a 22 G-bevel 30°, 85 mm block needle (Visioplex®, Vygon, Ecouen, France) by the same expert regional anesthesiologist. For the popliteal block, 20 mL of 1.5% lidocaine + epinephrine 1:200000 with bicarbonate was administered while the patient was in the lateral position. Then, in the supine position, 15 and 5 mL of the same solution was injected for the FN and LFCN block, respectively, and adequate spread of the drug around the nerves were monitored. In both groups, sensory and motor blockade was evaluated by an observer unaware of the study groups. The level of sensory block was assessed by the pinprick testing and the motor block by the Bromage scale 1 - 4 (1 = complete (unable to move feet or knee), 2 = almost complete (able to move feet only), 3 = partial (just able to move knee), and 4 = no motor block (full flexion of knee and feet) (12). In the case of block failure, the patient was excluded from the study and replaced. When a complete sensory and motor block was achieved, a pneumatic thigh tourniquet inflated to a 300 mmHg pressure was applied in the proximal part of the thigh. The tourniquet pain was assessed by a blinded observer immediately after tourniquet inflation (time 0), every 5 min up to 20 min, and then every 15 min until the end of surgery with a 5-point verbal rating scale (VRS) (0 = no pain, 1 = mild pain, 2 = moderate pain, 3 = severe pain, and 4 = unbearable pain). When the patient complained of pain or VRS was > 1, if the level of surgical anesthesia was sufficient, intermittent bolus doses of intravenous fentanyl or ketamine were given alternatively. Fentanyl was given in 50 µg boluses, and in case of insufficient pain relief, additional analgesia with ketamine was given in 10 mg boluses. If inadequate, general anesthesia was established. The time taken to perform the block (block performance time), the time required from the end of local anesthetic injection to achieve adequate surgical anesthesia (anesthetic effect time), intraoperative tourniquet pain scores, the amount of fentanyl and ketamine, surgery duration, and any complication were recorded. At the end of the surgery, the patient’s satisfaction was graded as 4: very satisfied, 3: satisfied, 2: fairly satisfied, 1: poorly satisfied.
3.1. Statistical Analysis
SPSS version 23 and MATLAB software was used for statistical analyses. A sample size of at least 25 patients per group was required to detect a one-point difference in pain scores between the study groups, with a power of 80% and a significance level of 5%. The t-test and Mann-Whitney U-test were used to compare the quantitative variables and the chi-square and Fisher’s exact test to compare the categorical variables between the groups. A paired t-test and analysis of variance (ANOVA) were used to calculate intergroup pain score differences. Data are expressed as mean ± standard deviation or numbers. A P value of less than 0.05 was considered significant.
4. Results
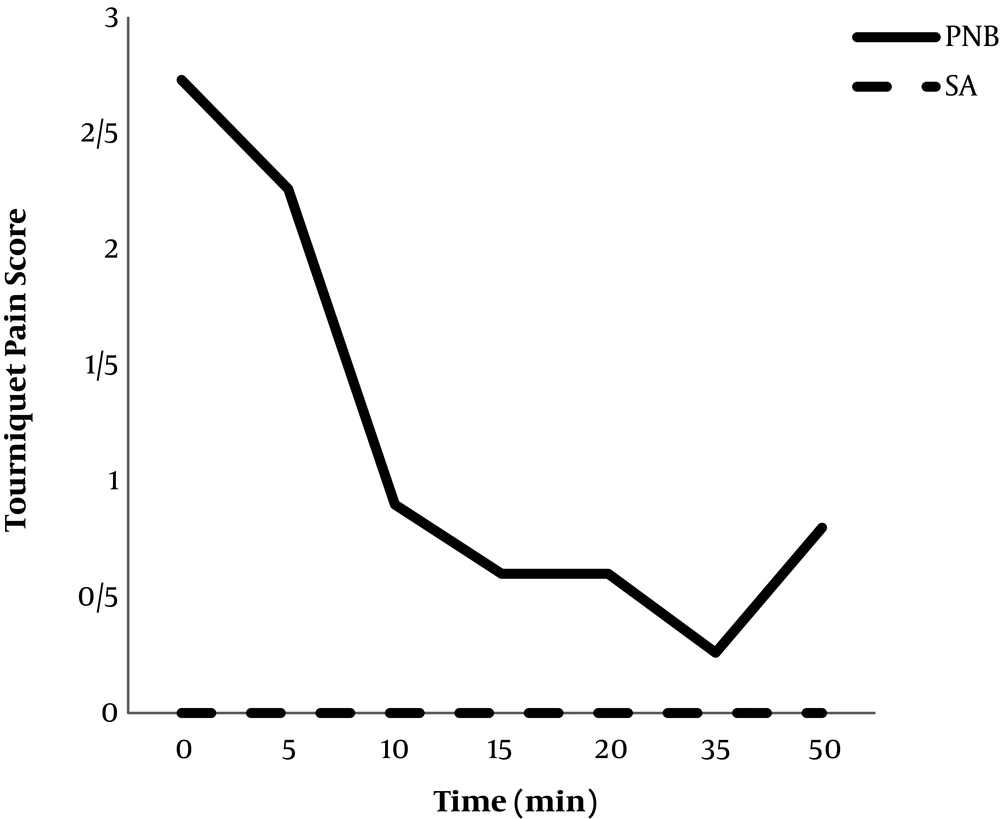
Sixty patients (30 patients in each group, 23 women and 37 men), aged 14 - 76 years were entered into the study. Patients’ characteristics in the PNB and SA groups were comparable (Table 1). The mean duration of block performance and anesthetic effect, the mean tourniquet pain scores after its inflation, and the total amount of fentanyl and ketamine administered during surgery were significantly higher in the PNB group compared with the SA group (Table 1 and Figure 1). The satisfaction score was similar in both groups, and patients rated it as “satisfied”. No serious complication was noted in patients throughout the surgery. Also, no patient needed general anesthesia during the operation.
| PNB Group (N = 30) | SA Group (N = 30) | P Value | |
|---|---|---|---|
| Gender (F:M) | 9:21 | 16:14 | > 0.05 |
| Age, y | 37.6 ± 13.6 (18-65) | 39.5 ± 16.8 (18-76) | 0.63 |
| Height, cm | 173.73 ± 11.49 | 169.23 ± 8.73 | 0.09 |
| BMI | 27.17 ± 3.88 | 25.74 ± 4.69 | 0.2 |
| ASA class (1:2) | 23:7 | 22:8 | 0.83 |
| Surgery length, min | 75.66 ± 12.26 | 61.66 ± 12.73 | 0.1 |
| Tourniquet inflation duration, min | 68.33 ± 14.62 | 53.16 ± 13.52 | 0.08 |
| Block performance time, min | 16.16 ± 2.4 | 9.33 ± 0.91 | < 0.001b |
| Anesthetic effect time, min | 11.83 ± 2.45 | 9.83 ± 0.91 | < 0.001b |
| Intraoperative fentanyl, µg | 103.33 ± 65.56 | 10 ± 3.51 | < 0.001b |
| Intraoperative ketamine, mg | 40 ± 7.2 | 0 | 0.005b |
| VRS of tourniquet pain (0 - 4) | 1.3 ± 0.5 | 0 | < 0.001b |
Abbreviations: ASA, American Society of Anesthesiologists physical status classification; F, female; M, male; PNB, peripheral nerve block; SA, spinal anesthesia; VRS, verbal rating scale.
aValues are expressed as mean ± SD and numbers.
bThere was a significant difference between the two groups (P < 0.05).
5. Discussion
The present study showed that compared with spinal anesthesia, combined ultrasound-guided femoral/LFCN block when performed with a popliteal block does not provide an adequate sensory block for tourniquet pain, and significantly more intravenous analgesics are required to reduce the pain. Time to perform the block and being ready for the operation were also significantly longer in the PNB patients than the SA group. However, patients’ satisfaction was similar in both groups. According to our results, combined blockade of FN and LFCN when supplemented with intravenous analgesics can improve thigh tourniquet tolerance in short to medium duration of foot or ankle surgical procedures. Patients with compromised cardiopulmonary function, the elderly or those, for whom performing spinal anesthesia is difficult, can benefit from this method.
There are several studies that compared different nerve blocks with spinal anesthesia in lower limb operations. In those studies, as in our research, longer duration of block performance and block effect time, as well as inadequate relief of tourniquet pain, were observed, which could be the limiting factors for the common use of PNB (13, 14). Similar to our findings, some other studies also concluded that peripheral nerve blocks in combination with additional sedoanalgesia are an alternative anesthesia method for tourniquet pain relief in lower extremity surgeries in patients at high risk for general or neuraxial anesthesia (8, 10, 14).
There may be some explanations for the results of the present study. The exact cause of tourniquet pain is not clear. Tourniquet pain is thought to be conducted by the unmyelinated C- fibers, which are responsible for slow pain and are more resistant to local anesthetics than the myelinated A-fibers transmitting fast pain. Administration of local anesthetic inhibits nerve conduction in both A and C fibers. When the concentration of the drug decreases, the C fibers may become unblocked before the A-fibers, resulting in the occurrence of tourniquet pain while the level of sensory anesthesia is adequate (15, 16). One possible explanation could be a faster reduction in lidocaine concentration around the peripheral nerves than in the cerebrospinal fluid, resulting in faster activation of C fibers and a greater incidence of tourniquet pain in comparison with spinal anesthesia (17). We used a total of 600 mg of 1.5% lidocaine with epinephrine, of which 15 mL and 5 mL were injected for the block of FN and LFCN, respectively. Another possible reason may be that this dose was not high enough for a dense and long C-fiber blockade, although it adequately blocked pinprick sensation. On the other hand, some may feel that the total dosage of lidocaine was high and could increase the risk of toxicity. However, no serious complication was seen in our patients. Likewise, previous studies used similar doses and found no systemic adverse effects (4, 8, 13, 14). However, further studies are needed to determine the appropriate dose of local anesthetics for tourniquet pain tolerance.
Blockade of the FN and the LFCN provides sensory anesthesia of the anteromedial and anterolateral thigh and keeps the posterior part of the thigh unaffected. This may be a reason for insufficient relief of tourniquet pain through the blockage of these nerves. Therefore, blockage of the posterior femoral cutaneous nerve (PFCN) might be necessary to tolerate thigh tourniquet. The proximal sciatic nerve supplies the posterior thigh, and its block have a high possibility of sensory block of the PFCN (18, 19). Alternatively, the PFCN can be blocked separately under ultrasound guidance (20). Therefore, the combination of proximal sciatic nerve block with FN and LFCN block may greatly suppress thigh pain after tourniquet inflation. In this regard, Spasiano et al. (21) compared spinal anesthesia with combined proximal sciatic and femoral blocks in arthroscopic knee surgery and reported comparable tourniquet pain scores and satisfaction in both techniques. In contrast, Fuzier et al. (5) showed that with the addition of a femoral block, the proximal approach of the sciatic nerve block, despite the sensory blockade of PFCN provides no better thigh tourniquet relief than the popliteal approach during foot surgery. Because of the controversies, more randomized, comparative studies are needed to investigate the role of the PFCN block in preventing tourniquet pain.
Of the limitations of our study were that the postoperative pain and analgesic requirements, as well as the duration of sensory and motor block were not assessed in the two groups, which was due to the shortage of trained staff in the perioperative period. However, it did not affect the goal of this study.
5.1. Conclusions
Spinal anesthesia is significantly more effective than the peripheral nerve block method in reducing thigh tourniquet pain during foot or ankle surgeries. However, when a combined ultrasound-guided femoral and lateral femoral cutaneous nerve block along with popliteal block is supplemented with intravenous analgesics, it can improve thigh tourniquet tolerance. Patients unsuitable for general or neuraxial anesthesia can benefit from this method.