1. Background
The rapid increase in the number and severity of critically ill patients with COVID-19 in early 2020 highlighted how quickly the health care systems should be ready to provide appropriate critical care. Almost five percent of COVID-19 patients require intensive care medicine admission, and most of them are complicated with acute respiratory distress syndrome (ARDS) (1). During this short time, the critical care community has gained valuable experiences regarding this disease; however, the mortality rate for ICU patients, especially mechanically ventilated ones, is still high. There are some nonspecific therapeutic agents for COVID-19 patients, but the antiviral efficacy of these drugs is not yet known (2). We now know that patients suffering from cytokine storm rapidly deteriorate and develop multi-organ failure. Therefore, early diagnosis and appropriate management of critically ill patients with cytokine storm and prompt initiation of immunomodulatory treatment may be beneficial. Therefore, routine monitoring of these patients with an H-score can help to discriminate patients with cytokine storm. There are some theories regarding the pathophysiology of ARDS caused by COVID-19 (3). Some believe in the role of iron that leads to inflammation of alveolar macrophages and toxicity with a possible positive effect of blood transfusion and convalescent plasma while using invasive mechanical ventilation with high PEEP can worsen the outcome (4). However, transfusion can increase pulmonary injury. Gattinoni et al. describe two types of H (high) and L (low) based on the elastance, right to left shunt, lung weight, and recruitability (5). They described that patients with H type respond well to high levels of PEEP. Actually, this hypoxemia is a specific syndrome with highly heterogeneous characteristics. Unlike SARS and MERS, the viral load in the respiratory secretion of COVID-19 patients peaks at the time of symptoms; thus, effective antiviral therapy should be started as soon as possible and, if given after 48 hours, may not be very effective. Recently, the results of a study showed that the most commonly used antiviral therapy in the world, hydroxychloroquine, is not effective against the coronavirus and even increases respiratory dependence.
2. Methods
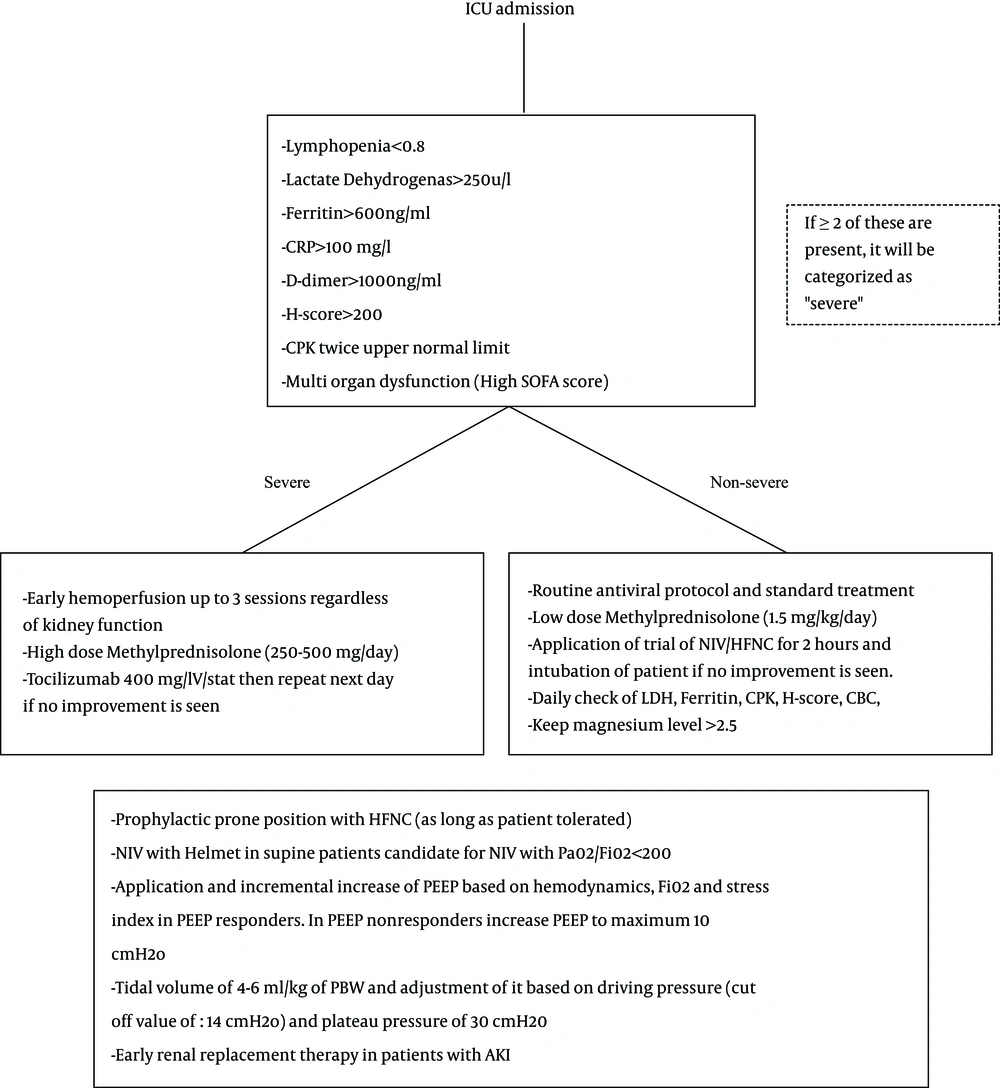
Our hospital is the largest university-affiliated hospital in the northwest of Iran, Imam Reza Hospital, TUOMS. We have been involved in the management of critically ill COVID-19 patients from almost February 20th, 2020. During this period, we have admitted more than 200 critically ill patients in our ICUs. After ICU admission, patients were divided into two groups based on clinical symptoms (fever, tachypnea and decreased level of consciousness), comorbidities (cardiovascular, kidney injury, diabetes, immunosuppression, and morbid obesity) and lab findings (ferritin, LDH, CPK, D-dimer, lymphopenia, CRP) and H-score. We assessed the H-score for our patients besides other severity markers for evaluation of the possibility of cytokine storm. The score consisted of known underlying immunosuppression, body temperature, hemophagocytic features in bone marrow aspirates, organomegaly, amount of cytopenia, ferritin, triglyceride, AST, and fibrinogen levels in COVID-19 patients. In this classification, we did not consider intubation or requiring NIV/HFNC for severity. All patients received standard treatment for critically ill patients. They received enteral nutrition in the first 24 hours of admission with the target of 25 kcal/kg and at least 1.5 g/kg protein unless in the existence of acute kidney injury (AKI). If patients did not tolerate enteral nutrition, we would start parenteral (total or supplemental) based on the patient’s requirement. We routinely ordered antiviral drugs (hydroxychloroquine and lopinavir/ritonavir), and empirical antimicrobial therapy and de-escalation based on microbial results. Electrolytes and especially magnesium, were checked routinely and magnesium was kept higher than 2.5 mg/dL to decrease the incidence of arrhythmia with treatment drugs. We did not routinely suppress the fever in our patients unless there were high grades of hyperthermia, presence of acute coronary syndrome, acute neurologic insult, or in pregnant women. Vitamin C was ordered in a medium dosage of 4 - 8 g/day except in the presence of AKI. For patients in the severe group, we considered corticosteroid or hemoperfusion or tocilizumab, individually. Intensive blood glucose management and stress ulcer prophylaxis was performed with high dose corticosteroid therapy. All patients under mechanical ventilation underwent lung-protective strategy (4 - 6 mL/kg PBW), which was adjusted based on driving pressure cut off value of 14. If the patient was PEEP responder, we increased PEEP based on the patient’s hemodynamic, Fio2, and stress index (SI) but if he/she was not PEEP responsive, we did not increase above 10 cmH2O. Stress index > 1 suggests over-distention (A decrease in compliance as the lungs are inflated); at the next step, we decreased the tidal volume and PEEP if the patient had a plateau pressure over 30 or driving pressure more than 14. If the stress index was > 1 and plateau pressure was < 30 or driving pressure < 14, tidal volume was unchanged while PEEP could be unchanged or decreased. If the stress index was < 1, it suggests tidal recruitment (an increase in compliance as the lungs are inflated); at the next step, we increased the PEEP without any change in tidal volume if the patient had a plateau pressure > 30 or driving pressure > 14. But if the patient had SI < 1 and the plateau pressure < 30 or driving pressure < 14, both tidal volume and PEEP were increased. We used prophylactic prone position in awake cooperate patients with Pao2/Fio2 < 200 and emphasized them to tolerate the position as long as they could. We used a helmet as a device of choice for patients scheduled for non-invasive ventilation. Respiratory adjunct therapy was performed for all patients and incentive spirometry for awake cooperative patients. We also performed early renal replacement therapy for our patients with AKI. The protocol is summarized in Figure 1. If the patient was in a cytokine storm, we performed hemoperfusion, administered tacilizumab or high dose corticosteroids. Actually, there was not any choice for using hemoperfusion or tocilizumab, and the selection was based on the availability. However, almost all of the patients with cytokine storm received methylprednisolone as a corticosteroid.
3. Results and Discussion
With this approach, we managed almost 200 critically ill COVID-19 patients in our center. During this period almost 60% of our patients underwent mechanical ventilation, 25% underwent non-invasive ventilation and 15% received supplementary oxygen via facial oxygen masks. Twenty-five percent of our patients developed acute kidney injury from whom 15% of them required renal replacement therapy during their management. Fifteen patients received hemoperfusion (Jafron hemoabsorber, HA330 Disposable Hemoperfusion Cartridge), 7 patients received tocilizumab and almost 25 received interferon. Hemoperfusion was combined with renal replacement therapy in four patients but it was exclusively performed in the remaining 11 patients. Seven of our patients with a history of hemoperfusion died and others survived. Early application of prone positioning (6) in non-intubated patients was performed in almost 10 patients, from which 20 % of them were intubated and expired. Prone positioning as a rescue therapy in severe intubated ARDS patients was not performed in our institute because of technical problems with its use. The overall mortality rate for our patients was almost 45% which was similar to other reported incidences in COVID-19 patients.
Finally, there are many unknown questions and puzzle pieces which should describe the clinical course of COVID-19 and its complications especially ARDS. Considering the absence of an effective and curative treatment, many management protocols have been introduced in the treatment of COVID-19 patients. However, it is too early to see any published results of strict clinical data. We provide the initial immediate surge response to allow every patient in need for an ICU bed to receive one. Till our knowledge is improved, the most important intervention in the treatment of critically ill patients with COVID-19 seems to be the level of standard care and appropriate and early diagnosis and treatment. This treatment should now be performed regardless of the reason which lies behind the pathophysiology of this disease which is yet unknown.