1. Background
In December 2019, the city of Wuhan in China experienced novel, unknown pneumonia, which later was diagnosed to be caused by a newly discovered virus, named as Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) or COVID-19 (1). A few months afterward, the World Health Organization (WHO) announced COVID-19 as a global pandemic on 12/03/2020 (2). The COVID-19 pandemic has overwhelmed all countries around the globe. The fast-spreading of this virus and the lack of knowledge about it have increased the fears and ideas about this vague enemy. Its lethality among the medical personnel and the high probability of getting infected put the medical personnel under stress and pressure.
It is hard to face a new virus with a lack of data and treatment. However, the pandemic is compulsory and has started in some countries and is coming soon in others. In Egypt, the pandemic has not started yet (till the time of this writing), but the stress and pressure have arrived in advance.
The ICU and anesthesia physicians are the frontline doctors who will deal early with the suspected or confirmed patients with the probability of experiencing psychological disturbances and mental health problems. Many previous studies that tested these issues (3-6) reported factors such as increased workload, lack of Personal Protection Equipment (PPE), lack of vaccine or treatment, social stigma, and high incidence of the spread of this disease, especially to their families, will contribute to the above-mentioned adverse mental and psychological effects.
2. Objectives
In this study, we examined the level of stress and the most worried fears and thoughts among the physicians in the anesthesia and ICU departments by designing a questioner and a specific scale.
3. Methods
After Institutional Ethics Committee approval, a questionnaire was designed and distributed to all the anesthesia and ICU physicians in Cairo university hospitals via social media links and official emails. The first paragraph was to obtain the consent of the physicians to participate in this survey. The participants were allowed to withdraw from the study whenever they needed it. The anonymity and confidentiality of data were observed. The survey was anonymous to ensure confidentiality. It was designed as a link in the Survey Monkey (7), so the researchers were blinded to the participants.
The questionnaire included information about age, sex, level of experience, 10 questions of Perceived Stress Scale (PSS-10), and questions designed to assess the causes of the stress related to the COVID-19 pandemic. The participants were supposed to answer all questions (Table 1).
| Mental stress in Anesthesia and Intensive Care Physicians During the COVID-19 Outbreak Survey |
|---|
| Dear Participant, Hope you are doing well during this stressful and challenging time. We are currently conducting a study, aiming to measure the degree of mental stress that you may perceive, working in the frontline during the COVID-19 outbreak. We would appreciate your help by filling in this survey. We are using a validated tool for measuring psychological stress, namely the Perceived Stress Scale (PSS). You are free to refuse participation in this survey. All responses will be anonymous. However, we will utilize the demographics data (age, gender, specialty, experience level, location of practice, and exposure to COVID-19 patients) to stratify the results. We thank every one of you for your cooperation and participation in this study. Stay safe. |
| 1. Your gender: M/F/ Prefer not to say |
| 2. Your age group: 25-34/35-44/45-54/55-64/65+ |
| 3. Your experience level: Registrar/ Consultant |
| 4. Your Speciality: Anaesthesia/ICU |
| 5. Exposure to COVID-19 patients: Not dealing with potential (symptomatic) or confirmed cases/ occasionally dealing with potential (symptomatic) or confirmed cases/ Regularly dealing with symptomatic or confirmed cases |
| 6. In the last month, how often have you been upset because of something that happened unexpectedly: Never/Almost never/sometimes/fairly often/very often |
| 7. In the last month, how often have you felt that you were unable to control the important things in your life? Never/Almost never/sometimes/fairly often/very often |
| 8. In the last month, how often have you felt nervous and stressed? Never/Almost never/sometimes/fairly often/very often |
| 9. In the last month, how often have you felt confident about your ability to handle your personal problems? Never/Almost never/sometimes/fairly often/very often |
| 10. In the last month, how often have you felt that things were going your way? Never/Almost never/sometimes/fairly often/very often |
| 11. In the last month, how often have you found that you could not cope with all the things that you had to do? Never/Almost never/sometimes/fairly often/very often |
| 12. In the last month, how often have you been able to control irritations in your life? Never/Almost never/sometimes/fairly often/very often |
| 13. In the last month, how often have you felt that you were on top of things? Never/Almost never/sometimes/fairly often/very often |
| 14. In the last month, how often have you been angered because of things that happened that were outside of your control? Never/Almost never/sometimes/fairly often/very often |
| 15. In the last month, how often have you felt difficulties were piling up so high that you could not overcome them? Never/Almost never/sometimes/fairly often/very often |
| 16. The main cause of stress: Please order the following from 1 to 10, with 1 being the most stressful and 10 the least. You can ignore any of these statements if they do not cause you any stress. |
| Lack of clear protocol on how to deal with COVID-19 cases/Lack of clear protocol on how to deal with unconfirmed/undiagnosed cases/Inadequate training on how to put on and take off PPE/Insufficient availability of PPE/The emotional stress of dealing with critically ill patients/Being overwhelmed by increased workload/Fear that I might contract COVID-19/Fear that I might transmit COVID-19 to the family and loved ones. DONE. |
The PSS-10 included 10 questions and allowed the assessment of the perceived stress of an individual. The questions were answered from 0 to 4 where 0 indicated never and 4 indicated always. The PSS scores are attained by reversing responses (4=0, 3=1, 2=2,1=3, 0=4) to the positively listed item, after that, adding all scale points. For PSS-10, a score of 13 is considered moderate, and a score of 20 or higher shows a high level of stress requiring lifestyle modification and learning stress reduction techniques (8).
3.1. Duration of the Study
The study was completed over one month from March 15, 2020, to April 15, 2020.
The sample size was estimated by the following formula (Slovin’s Formula): n = N [1 + N (e)2]-1 where n is the size of the sample, N is the population, and e is the variance of the sample (0.05). There are 351 anesthesia and ICU physicians in Cairo university hospitals, including all grades from registrars to senior consultants. Therefore, the sample size was 351 [1 + 351 (0.0025)]-1 =184 participants.
The study outcome was to assess the level of stress in participants using the PSS-10 and assess the possible causes of fears in their minds regarding the COVID-19 pandemic using the specific questions in the questionnaire.
3.2. Statistical Analysis
The IBM SPSS (20.0) program was used (Armonk, NY: IBM Corp) to analyze the data. The distribution of the data was tested by the Kolmogorov-Smirnov test. On the other hand, the chi-square test was used to compare the groups for variables of categories. Data with abnormal distribution were analyzed by the Mann-Whitney test. The significance level was set at 5%.
4. Results
A total of 193 physicians from the department of anesthesia and intensive care participated in the survey during the period from March 15, 2020, to April 15 2020, by using the Survey Monkey website link sent via official emails and different social media applications. We divided the participants according to the level of experience into two groups: Registrars (n = 101) and Consultants (n = 92) (Table 2).
| Question | Registrar (N = 101) | Consultant (N = 92) | P Value |
|---|---|---|---|
| What is your gender? | |||
| Male | 79 (78.2%) | 79 (85.9%) | 0.265 |
| Female | 20 (19.8%) | 13 (14.1%) | |
| Prefer not to say | 2 (2.0%) | 0 (0.0%) | |
| What is your age? | |||
| 25 to 34 | 42 (41.6%) | 2 (2.2%) | < 0.001a |
| 35 to 44 | 49 (48.5%) | 62 (67.4%) | 0.008a |
| 45 to 54 | 8 (7.9%) | 16 (17.4%) | 0.046a |
| 55 to 64 | 2 (2.0%) | 8 (8.7%) | 0.049a |
| 65 to 74 | 0 (0.0%) | 4 (4.3%) | 0.049a |
| 75 or older | 0 (0.0%) | 0 (0.0%) | - |
| Your specialty | |||
| Anesthesia | 94 (93.1%) | 86 (93.5%) | 0.910 |
| Intensive care | 7 (6.9%) | 6 (6.5%) | |
| Exposure to COVID-19 patients | |||
| Not dealing with potential | 32 (31.7%) | 52 (56.5%) | 0.001a |
| Occasionally dealing with potential cases | 55 (54.5%) | 38 (41.3%) | 0.068 |
| Regularly dealing with symptomatic cases | 14 (13.9%) | 2 (2.2%) | 0.003a |
aStatistically significant
The demographic parameters such as age, sex, specialty, and exposure to COVID-19 patients were comparable between the two groups, which were statistically significant (Table 2). Regarding the specialty, most of the participants were anesthetists (n = 180; 93.26%) and a minority of them were intensivists (n = 13; 6.735%) (both ICU and anesthesia physicians are working in one department with different rotation). Because of the low incidence of new cases of COVID-19 in Egypt, the number of participants who regularly dealt with symptomatic cases was 16 (16.1%), most of whom were registrars (n = 14; 13.9%).
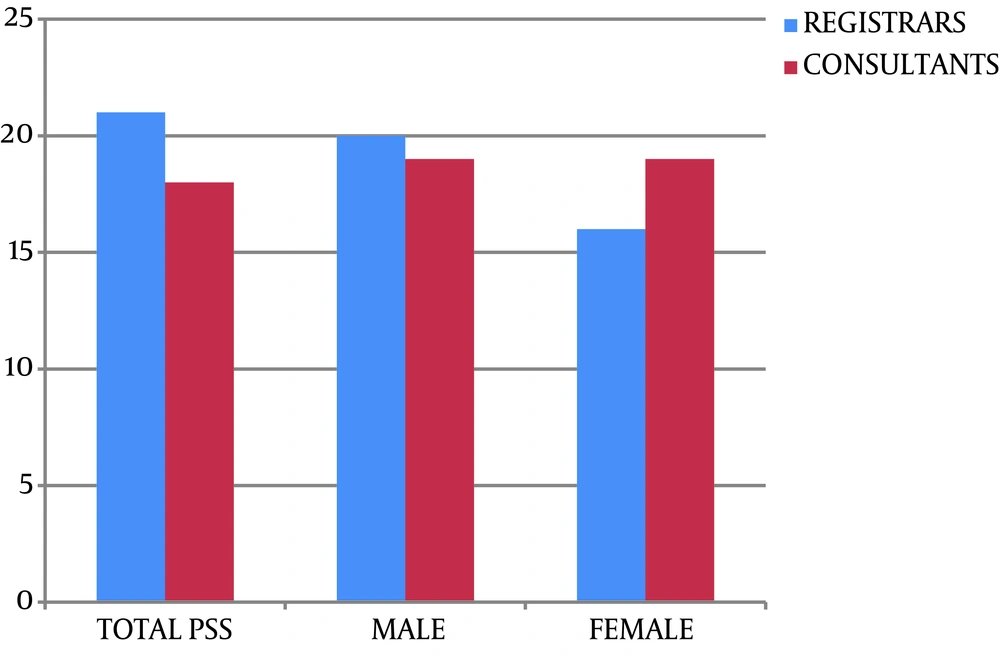
The PSS-10 median score was 21 in the registrar group and 18 in the consultant group, and this difference was considered significant (P = 0.03) (Figure 1). On the other hand, no differences have been noted regarding gender (P-value ≥ 0.05) (Figure 1).
Regarding questions designed to detect the causes of stress among the participants in the survey, (The leading cause of stress: Please order the following from 1 to 10, with 10 being the most stressful and 1 is the least. You can escape any of these statements if it does not cause you any stress).
The results were not statistically significant between the two groups, except for the question “Lack of a clear protocol on how to deal with unconfirmed/undiagnosed cases,” which was statistically significant with a p-value of 0.017. Furthermore, the other question was “Fear that I might contract COVID-19” with a p-value of 0.035 (Table 3).
| Registrar | Consultant | P Value | |
|---|---|---|---|
| Lack of a clear protocol on how to deal with COVID-19 cases | (n = 101) | (n = 90)a | |
| Mean ± SD | 6.6 ± 3.0 | 6.2 ± 2.6 | 0.194 |
| Median (min - max) | 7.0 (1.0 - 10.0) | 7.0 (1.0 - 10.0) | |
| Lack of a clear protocol on how to deal with unconfirmed/undiagnosed cases | (n = 101) | (n = 92) | |
| Mean ± SD | 6.7 ± 2.9 | 5.8 ± 2.7 | 0.017b |
| Median (min - max) | 7.0 (1.0 - 10.0) | 6.0 (1.0 - 10.0) | |
| Inadequate training on how to put on and take off PPE | (n = 101) | (n = 92) | |
| Mean ± SD | 5.8 ± 3.1 | 6.0 ± 2.6 | 0.816 |
| Median (min - max) | 6.0 (1.0 - 10.0) | 6.0 (1.0 - 10.0) | |
| Insufficient availability of PPE | (n = 99)a | (n = 88)a | |
| Mean ± SD | 6.3 ± 3.3 | 6.6 ± 3.3 | 0.663 |
| Median (min - max) | 7.0 (1.0 - 10.0) | 7.5 (1.0 - 10.0) | |
| Emotional stress of dealing with critically ill patients | (n = 101) | (n = 92) | |
| Mean ± SD | 6.0 ± 3.2 | 5.9 ± 3.1 | 0.763 |
| Median (min - max) | 6.0 (1.0 - 10.0) | 6.5 (1.0 - 10.0) | |
| Being overwhelmed by increased workload | (n = 99)a | (n = 90)a | |
| Mean ± SD | 5.0 ± 2.9 | 5.8 ± 3.0 | 0.081 |
| Median (min - max) | 5.0 (1.0 - 10.0) | 5.5 (1.0 - 10.0) | |
| Fear that I might contract COVID-19 | (n = 99)a | (n = 92)a | |
| Mean ± SD | 6.5 ± 3.2 | 7.6 ± 2.8 | 0.035b |
| Median (min - max) | 7.0 (1.0 - 10.0) | 9.0 (1.0 - 10.0) | |
| Fear that I might transmit COVID-19 to the family and loved ones | (n = 101) | (n = 90)a | |
| Mean ± SD | 8.0 ± 2.9 | 8.6 ± 2.2 | 0.618 |
| Median (min - max) | 10.0 (1.0 - 10.0) | 10.0 (1.0 - 10.0) |
aNo questions were neglected by the participants
bStatistically significant
5. Discussion
Our survey revealed a high prevalence of mental stress among anesthesia and intensive care physicians (registrars and consultants) treating suspected or confirmed patients with COVID-19 in Cairo University hospitals. Most of the participants were males and aged 26 to 45 years. The study revealed a noteworthy percentage of 65% of members engaging in high levels of psychological distress during this acute situation. In a similar study in Wuhan, China, recently published during this pandemic, 70% of healthcare workers reported psychological symptoms (9).
The psychological reaction of physicians to an epidemic of infectious viruses is complicated. The causes of agony consist of feelings of exposure or unavoidable and worries about the spreading of the disease to their families and colleagues (10). The point that COVID-19 is a transmissible disease among humans, concomitant with extraordinary morbidity, and is hypothetically fatal (11, 12) may increase the awareness of self-hazard. Likewise, the anticipated lack of supplies, personal protective equipment, and no clear protocols to manage the doubted and confirmed cases of COVID-19 add to the burdens and worries of physicians (13-17).
Our study confirmed these concepts, as the results revealed that most participants had fears that they might transmit the disease to their loved people and the lack of clear protocol on how to deal with COVID-19 cases, either suspected or confirmed, was annoying them, causing immense stress along with the insufficient availability of PPE.
The core message from this study was to understand the level of stress and the type of fears. Moreover, it focused on the most important causes of fears and subsequently the methods of handling. The first step on the way to relieve the stress is to remove its causes that can be achieved by proper knowledge and health education. The second step is to build up trust among health care providers, infection control personnel, authorities, administration staff, and patients. This can be achieved by frequent meetings and open discussion among all the previously mentioned panels.
5.1. Limitations
This study has a few limitations. First, despite Cairo university hospitals represent a major section of the medical community in Egypt, it is still limited in scope, restricting the implication of the results to other healthcare workers in other centers and regions of the country. Second, the study was carried out for one month. Because of the increasingly difficult situation, the mental health symptoms of healthcare workers could become more severe. Thus, the long-term psychological implications of this population deserve further investigations. Third, it did not distinguish pre-existing mental health symptoms and new symptoms. Furthermore, the study explored the stress among anesthesia and ICU specialty physicians who were in the frontline. Whereas, similar findings could be found across physicians of other medical specialties, as well. Finally, the article dealt with mental stress at the beginning of the COVID-19 pandemic. Hence, there must be further study and questionnaire in the middle and the end of the pandemic.
5.2. Conclusion
In this survey study of anesthesia and ICU physicians, the spreading of COVID-19 resulted in a lot of symptoms of mental stress. Healthcare workers’ protection is an essential element in public health procedures for combating the COVID-19 pandemic. Particular interventions to improve the mental health of healthcare providers who are dealing with COVID-19 have to be instantaneously applied.