1. Introduction
Discitis is a rare complication of the post spine procedure, representing 30.1% of all pyogenic discitis cases, and can be caused by either open or minimally invasive spine procedure (1). Early diagnosis is essential to prevent further complications, although it is very challenging. Treatment of discitis is bed rest and antibiotics administration from four weeks to six months. However, surgical intervention is required in some patients with progressive neurologic deficit (2, 3). Radiofrequency nucleoplasty is a procedure employing coblation technology to coagulate and ablate the intervertebral disc with a low-temperature (52°C) plasma field results in minimal collateral damage to adjacent tissue. Radiofrequency nucleoplasty is considerably successful in relieving low back pain (4-7), decreasing morbidity, and shortening the recovery time (8). The current study reported a case with discitis following radiofrequency nucleoplasty.
2. Case Presentation
2.1. History and Presentation
A 62-year-old male patient referred to the pain specialist with a chief complaint of 10 years of low back pain, gradually worsening for the last two years. The patient was a former member of the armed forces with a history of hard training. The pain started from the left part of the back; the buttock fascinating pain that went down to the medial part of the thigh to the calf and presented as a constant, sharp, burn-like sensation with paresthesia of the toe and exceeded by coughing and walking. At best, his pain score was 4/l0 based on the visual analogue scale (VAS) and 10/10 at its worst. He took diazepam and underwent a physiotherapy program; both were fruitless. He denied any bladder symptoms. The patient had hypertension and chronic kidney disease with routine dialysis twice a week.
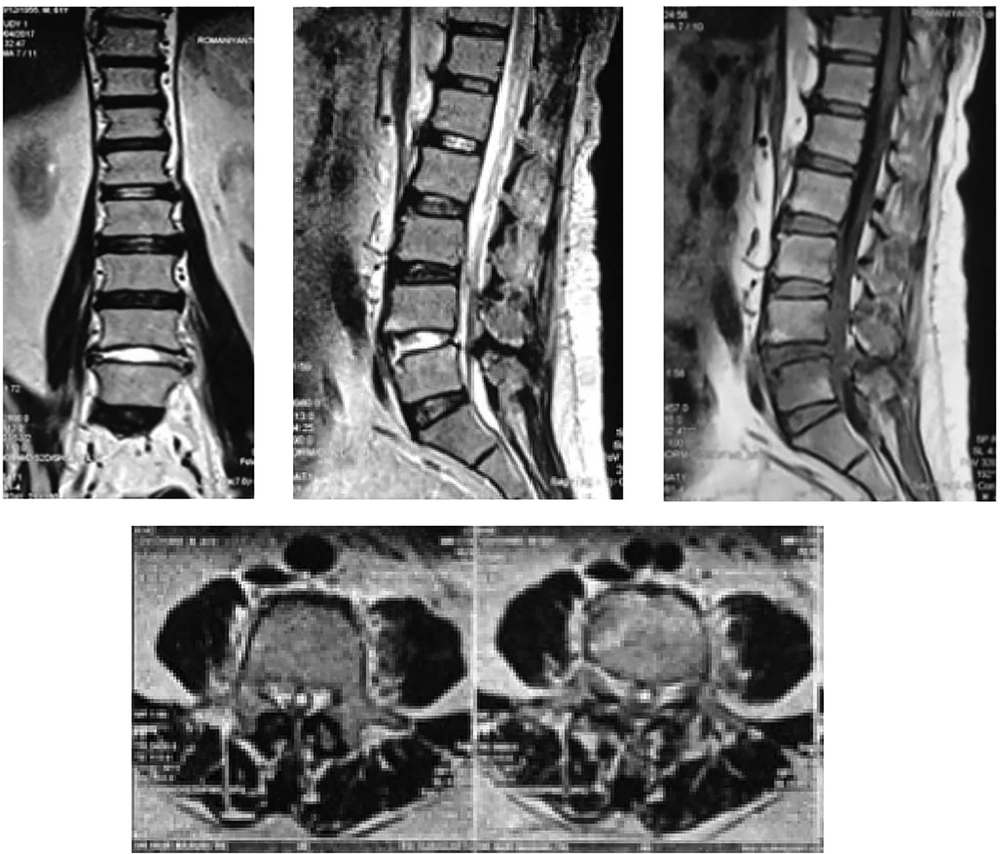
Physical examinations on admission showed lumbar lordosis and limited trunk movement, increased stuffiness in the bilateral lumbar paraspinal muscles, latissimus dorsi, and gluteal by palpation. There was hyperalgesia at approximately L4 - S1, bilateral lumbar paraspinal muscles, latissimus dorsi, gluteal, and posterior-superior iliac spines (PSISs). Physiological reflex was normal and pathological reflexes were negative on both lower extremities. The results of the straight leg raise test and manual lumbar distraction were positive. The results of laboratory tests, including hemoglobin, leukocyte, thrombocyte, hematocrit, natrium, potassium, chloride, and the prothrombin time/ partial thromboplastin time, were within the normal range. There were slight increases in urea and creatinine and decreases in calcium levels. MR (magnetic resonance) image of the thoracolumbar spine is shown in Figure 1.
Pain physician decided to perform lumbar medial branch block using radiofrequency and radiofrequency nucleoplasty of L4-L5 (Flextrode introducer kit, FLEX-K151320-5P, Cosman, USA). A motor stimulation at 2 Hz, sensory stimulation at 50 Hz, and lesioning at 67°C for 60 seconds were also conducted. His complaint disappeared immediately after the interventions.
Three days later, the patient felt pain in the same location before the intervention and weakness in the lower limbs. Then, he did not visit the pain specialist until unable to move his legs and complain of urinary and fecal incontinence three weeks after the interventions. The patient decided to check his condition with the pain specialist.
Physical examinations indicated the loss of sensory functions in the legs, and the motoric test showed an inability to lift legs. Muscle stretch reflexes were 0/0 in the bilateral knee jerk and bilateral Achilles tendon reflexes, while the Babinski sign on the lower extremities was negative. MRI of the lumbar spine was performed, and the results were hyperintensity at discus vertebra L4 and L5, suspicious discitis (Figure 2)
Laminectomy at L4 and L5 was performed, and an inflamed intervertebral disc was found; no pus or abscess was detected. The culture of the specimens had negative results. The patient recovered from the surgery, and after eight months, he could feel and lift legs, and urinary and fecal incontinence was also controlled. On the last physical examination, the patient reported pain on the left part of the back, prickling to the medial aspect of the thigh. The sensory and motor examinations noted a 5/5 disturbance in legs.
3. Discussion
Discitis is a potential complication that may occur after an intradiscal procedure. A review of side effects and complications of intradiscal procedures indicated only 30 cases (0.6%) of discitis in approximately 5000 disc procedures. A study on discography complications reported the discitis prevalence of less than 0.25% in patients undergoing the procedure (9, 10). To the best of the authors` knowledge, it was the first case of a discitis complication reported following a nucleoplasty radiofrequency.
There are various clinical findings of discitis; most are severe back pain at the affected levels. Reduced spinal range of motion, paraspinal muscle spasm, and tenderness on palpation are the early signs of discitis. Fever is reported in up to 50% of the cases. The reported case with a long history of radicular pain in the left lower extremity developed sudden paraplegia in paresis legs, and urinary and faecal incontinence, three weeks after radiofrequency nucleoplasty. This poor progression suggested the epidural space involvement caused by direct compression of the spinal cord by an obstructive osseous fragment or suppurative material (11).
As discitis is clinically suspected, MRI was the most reliable technique for early detection due to its high sensitivity (93%–96%) and specificity (92.5%–97%). Weighted images on T1 and T2 were also beneficial to see the irregular contour of vertebral endplates at a disc procedure level. The contrast was also added to visualize the expansion of discitis into the anterior epidural, psoas, and posterior paravertebral muscles. The discitis caused by infection is characterized by inflammation in epidural or paraspinal muscles, endplate erosion, disc fluid-signal intensity, and disc enhancement, according to MRI report (12, 13).
In the reported case, the most significant risk factors for discitis were diabetes and end-stage renal disease (ESRD). Previous studies showed that the most common discitis-related disease was diabetes mellitus in 18 patients (16.6%), followed by ESRD in 10 (9.25%) (14). A systematic review and other reports concluded that ESRD has a positive relationship with discitis through repeated vascular access (15, 16). Uremia in ESRD may alter immune status characterized by immunodepression and increased likelihood of infection, especially in those undergoing a spine procedural intervention, as observed in the reported case (17).
Discitis after an intradiscal procedure is caused by the invasion of bacterially-contaminated needles into the disc. Intervertebral discs are avascular structures nurtured through the annulus fibrosus depending on diffusion from capillary plexuses and vertebral endplates. The avascular disc structure makes it susceptible to bacterial inoculation during intradiscal procedures (18, 19). Spondylodiscitis is associated with a wide range of organisms; however, previous studies reported Staphylococcus aureus as a predominant pathogen, found in 28% of all positive cultures (14). It may be derived from the injection site, skin flora, needle, or medication contamination, even under sterile technique guidelines. Two recent meta-analyses compared the effectiveness of chlorhexidine-alcohol and povidone-iodine in skin preparation before surgical procedure and reported that chlorhexidine-alcohol was more effective than povidone-iodine (20, 21).
Radiofrequency nucleoplasty is categorized as a clean procedure with an infection risk of less than 2%, which might be increased by comorbidities. Application of antibiotic prophylaxis (AP) to prevent infections is not recommended for all procedures, especially the clean ones (22, 23). Cao et al., compared the patients given and not given AP in clean neurosurgery and observed no significant differences (24). An observational, randomized clinical trial by Estomba et al., showed that AP was unnecessary; the study included 204 patients undergoing clean head and neck surgeries (25). In the reported case, AP was not given before procedures. But it cannot be proven that the discitis was the outcome of APs absence. Further research on the administration of AP before intradiscal procedures is required.
The intravenous antimicrobial is almost an initial therapy. The duration of antibiotic therapy varies greatly. In a multicentre, observational, prospective study, the minimum course of antibiotic therapy ranged from 6 to 12 weeks, with an average duration of 14.7 weeks (10). In the reported case, the mean duration of intravenous antibiotic therapy was six weeks, followed by a further six weeks of oral administration. Surgery is usually performed for patients with progressive neurological deficit or intractable pain, spinal instability, and deformity due to significant endplate and vertebral destruction (26, 27).
3.1. Conclusion
Discitis is a common complication related to the intradiscal procedure. Early diagnosis of discitis is of great importance and challenging. The delay in diagnosis may lead to the development of neurological deficits. Heightened awareness and the proper use of MRI are essentials to elude diagnostic delays. Comprehensive treatment with bed rest, antimicrobial therapy, and sensible use of punctual intervention are essential for an optimal outcome.