1. Background
The novel coronavirus disease (COVID-19) due to severe acute respiratory coronavirus 2 (SARS-CoV-2) started in late 2019 with a global spread leading to a worldwide pandemic and an international health emergency (1, 2). Among many aspects of human life, this pandemic affected professional and emotional aspects of many people, including health care personnel; during this pandemic, there is always a potential chance that health care personnel shortage and physician burnout would happen; a major challenge that should be planned and managed (3). Iran was among the affected countries; facing a challenge due to the viral outbreak (4).
High-level intensive respiratory care quality, especially during the disease surge, is considered one of the bottlenecks in COVID-19 care; directly affecting COVID-19 attributed mortality rate (5-7). Anesthesiologists were considered one of the main cornerstones of critical care in patients with COVID-19 that many of them are affected by the disease or professional burnout leading to major concerns in delivering high-quality care with variable proposed solutions worldwide (3, 8-10).
More than five million people are under health care services by Shahid Beheshti University of Medical Sciences (SBMU), Tehran, Iran (11), including parts of the city and some of its suburbs. COVID-19 pandemic was a challenge mandating extraordinary care by Anesthesiology Department, SBMU. This included not only the academic medical centers but also the non-academic medical centers under the coverage of SBMU.
During the pandemic, SBMU had to seek the 3rd-year anesthesiology residents’ services as independent care, mainly in the suburb hospitals. Though senior anesthesiology residents have to pass one-month independent care in Iran, this experience was different in some aspects; due to COVID-19-related factors (8, 10). Attitudes of healthcare providers could demonstrate many aspects of a decision and would improve the decision-makers in the health system (12, 13); in other words, if the impact of a medical education process is going to be assessed appropriately, the attitudes and feedback from trainee are of utmost importance (13-15).
2. Objectives
This study was designed to assess the attitudes of 3rd-year anesthesiology residents toward an independent one-month-length clinical care course for patients with COVID-19; to find their attitudes and find potential opportunities from this threat in a developing country faced with a major threat.
3. Methods
The study was approved by Institutional Review Board (code: IR.SBMU.RETECH.REC.1399.664) Research Ethics Committee, Shahid Beheshti University of Medical Sciences, Tehran, Iran; besides, the requirement for written informed consent was waived by the IRB due to the study method.
In a cross-sectional descriptive-analytic attitude assessment study, using a Delphi method, a closed self-administered questionnaire was developed to assess the attitudes of 3rd-year clinical anesthesiology residents toward their professional experience during a one-month rotation serving patients with COVID-19 independently. To achieve the study sample size, a consensus method was used since the total target population was less than 20; i.e. all 3rd-year clinical anesthesiology residents were included.
After preparing the first draft of the questionnaire, the statements of the questionnaire were drafted and prepared on a 5-point Likert scale; then, the questionnaire was distributed among researchers and some other faculty members to increase face validity. The final questionnaire was an anonymous one with 29 closed answer questions added with an open-ended question about any other possible idea(s).
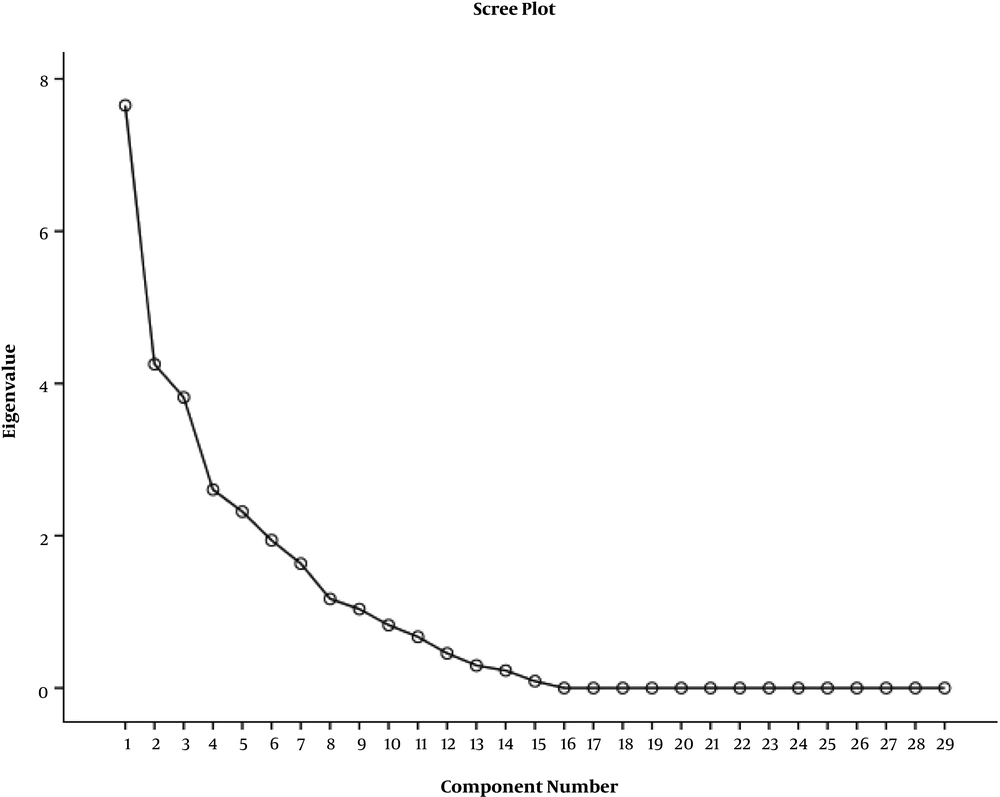
The study variables included the questionnaire items; which were quantitative ones; rated using the self-administered Likert scale. The age of the respondents and their gender were not included in the questionnaire to assure the anonymity of the replies since the sample size was 19. The results of the questionnaire responses were demonstrated and analyzed as a cumulative mean ± standard deviation (SD) for each question. Furthermore, Cronbach’s alpha was calculated to test the reliability of the questionnaire. Then, after calculating the eigenvalue for the questionnaire, the questions were categorized into seven factors using a factor analysis approach.
To support the residents, they had affiliated attending; available for telephone consult and support, in case they were faced with challenges in the decision-making process. In addition, the study was the result of a one-month rotation in SBMU; however, the residents were providing clinical care in different hospitals; though these hospitals had similar organizations and similar settings. Data entry and analysis were performed using SPSS (version 11.5; SPSS Inc, Chicago, IL, USA). To perform more advanced psychometric analysis, the eigenvalue and factor analysis were done.
4. Results
All 19 participants agreed to take part and respond to the questionnaire in an anonymous situation (n = 19). The reliability of the questionnaire was 0.678; i.e. Cronbach’s alpha = 0.678; for the whole questionnaire containing 29 closed statement questions; which suggested an appropriate level of reliability. The results of the 29 closed statement questions are demonstrated in Table 1 as the mean ± SD. Factor analysis resulted in an eigenvalue = 1 at 8 factors (Figure 1); however, after further analysis and based on the experiences of the research team, the factors were modified into seven factors indicated in Table 2 and Figure 1. Also, the full study questionnaire is summarized in Appendix 1 in Supplementary File.
| Question Number | Mean ± SD |
|---|---|
| Q1 | 4.47 ± 0.49 |
| Q2 | 2.01 ± 1.11 |
| Q3 | 3.92 ± 1.10 |
| Q4 | 2.95 ± 1.11 |
| Q5 | 4.15 ± 0.56 |
| Q6 | 4.53 ± 0.46 |
| Q7 | 1.58 ± 0.79 |
| Q8 | 3.05 ± 1.17 |
| Q9 | 3.00 ± 1.18 |
| Q10 | 1.26 ± 1.28 |
| Q11 | 3.94 ± 0.71 |
| Q12 | 3.78 ± 0.71 |
| Q13 | 3.95 ± 0.84 |
| Q14 | 3.88 ± 0.82 |
| Q15 | 3.79 ± 1.13 |
| Q16 | 2.12 ± 0.48 |
| Q17 | 3.96 ± 0.93 |
| Q18 | 3.74 ± 0.93 |
| Q19 | 3.95 ± 0.70 |
| Q20 | 4.05 ± 0.82 |
| Q21 | 3.98 ± 0.91 |
| Q22 | 3.67 ± 0.97 |
| Q23 | 2.58 ± 1.12 |
| Q24 | 4.00 ± 0.57 |
| Q25 | 4.21 ± 0.65 |
| Q26 | 2.95 ± 0.97 |
| Q27 | 3.89 ± 0.99 |
| Q28 | 2.89 ± 0.99 |
| Q29 | 1.67 ± 0.42 |
| Factor Number | Questions Categorized in the Factor | The Description of the Factor |
|---|---|---|
| Factor 1 | 1, 2, 7, 8, 9, 10, 18, 21 | Stress-related challenges during the course |
| Factor 2 | 3, 4, 5, 6, 23 | Stress-generating factors |
| Factor 3 | 15, 17, 22, 24 | Motivational factors to overcome stress |
| Factor 4 | 12, 13, 14, 16, 27, 28 | Self-regulated learning in OR and ICU care |
| Factor 5 | 11, 24, 25 | Self-esteem and satisfaction in clinical care |
| Factor 6 | 19, 20 | Disaster and crisis management |
| Factor 7 | 29 | Ethical aspects of clinical care |
5. Discussion
The current study demonstrated the role of an independent clinical rotation on different aspects of education and professional tasks of the 3rd year clinical anesthesiology residents based on their attitudes. This study showed that such a rotation, though maybe stress-provoking, could lead to some positive results and career-related improvements.
Iran is an eastern country with an ancient history of anesthesia (16). Throughout centuries, Iranian physicians have experienced a wide range of crisis management, including but not limited to earthquakes and war scenes (17, 18). However, the experiences gained in the COVID-19 pandemic were somewhat different, especially considering the global and national situation (4, 19).
Stress-related challenges are among the leading factors affecting the performance of healthcare and are due to several different issues such as occupational and/or infectious hazards, faulty health care process during epidemics, financial-related issues, and many others (3, 10, 20). Factor 1 demonstrated the stress-related items of the questionnaire; while nearly the majority of the anesthesiology residents had experienced the stress before going to the rotation. However, nearly all of them had been stress-free at the end of the rotation with varying degrees of stress relief throughout the one month; some were stress-free on the first day; while the others were stress-free in the middle of the last parts of the rotation. These findings support previous studies regarding the degree of stress during the COVID-19 pandemic in health care professionals (3, 10, 20, 21), demonstrating the rapid waning trend of the stress and burnout in the respondents’ experiences, possibly due to a multitude of factors. One of them could be the role of motivational factors, independence in delivering clinical care, and self-regulated learning that has been discussed in the next paragraphs.
Stress-generating factors were mainly related to the effects of entering a new work setting, which had not been experienced before, the fear of occupational hazards for the resident and his/her family and the challenges in working independently and the potential lack of sufficient indirect supervision (13, 22); these could be dealt with to manage stress and improve the professional efficiency (factor 2). Possibly, there would be more contributing items related to stress generation (10, 23); however, the residents did not mention any more items in the open question at the end of the survey.
Motivational factors were also important in the anesthesiology residents’ professional career, not only in fulfilling their duties but also in motivating them to overcome the stresses (factor 3). In a prominently motivational item, the majority of the respondents declared their readiness to take part in a similar professional experience on any future occasion that there would be any necessity in the future (question 17). Besides, the motivational factors led to the improvement in core clinical competencies of the clinical anesthesiology residents, including but not limited to professionalism, practice-based learning, and improvement, interpersonal and communication skills, and leadership capacities, based on the Accreditation Council for Graduate Medical Education (ACGME) core competency model (24-26). The role of motivational factors and affective domains in improving ACGME core competencies has been previously confirmed; which is consistent with our findings (27-29).
Self-regulated learning is one of the most important strategies for the “life-long professional development of medical education”; mainly due to the very rapid development of medical knowledge (30, 31). This rapid development is possibly the most prominent in such events as the COVID-19 pandemic (32, 33). The results of factor 4 demonstrated the prominent role of this “one-month clinical rotation” on self-regulated learning of clinical anesthesiology residents regarding OR and ICU care (Tables 1 and 2). In similar studies, it has been demonstrated that creating goal-directed structures could improve the personal and professional goals of senior students, leading to improvements in their professional achievements, which were similar to our findings regarding the effects of this one-month rotation on goal-directed learning in an independent clinical experience (34-36).
Self-esteem and satisfaction in clinical care were strongly improved, though care of patients with COVID-19 was considered a difficult clinical task based on the attitudes of the respondents to items in factor 5.
Disaster and crisis management was another prominent aspect of the COVID-19 pandemic, which was addressed in this questionnaire (factor 6), and the respondents declared their positive views regarding their role in COVID-19 crisis management (37, 38). These positive feedbacks did not just pertain to the current situation; instead, could affect the clinical residents to be more experienced for similar episodes of disaster and crisis management based on their attitudes. However, mental preparedness in disaster and crisis management is one of the cornerstones of the whole process of disaster management (37).
Ethical aspects of clinical care were the last factor that included just one question in our analysis and demonstrated that the residents did feel happy if they were in the situation and place of the caregivers. This issue should be considered an ethical approach because neglecting such an issue may deteriorate the global clinical function of the caregivers (39, 40).
5.1. Study Limitations
All the residents were 3rd-year anesthesiology residents who were at the same level; however, we had not compared them in terms of quality of practice, ability to make rational decisions, performance under pressure, and stress management in critical situations before starting the one-month COVID-19 rotation. For stress assessment, we did not use a standard guideline, which is a study drawback. The study would result in better external validity with reasonable and extensile findings if we could perform the research in a larger group of residents; this is suggested to be considered in similar future studies.
5.2. Conclusions
This one-month period could improve the competencies of the 3rd year clinical anesthesiology residents based on their viewpoints. Since the COVID-19 pandemic is ongoing health and social problem worldwide, 3rd-year anesthesiology residents (possibly other senior anesthesiology residents) could help the health system to recover health care delivery faults regarding manpower; this is a promising point, especially regarding preparedness during disaster and crisis, particularly in COVID-19 pandemic. Also, there were many constructive results for the clinical anesthesiology residents regarding their training and clinical service delivery.