1. Background
Spinal anesthesia is the most common method for a cesarean section at the current time (1-4). Hypotension is the most common complication of spinal anesthesia that occurs with a 30-60% incidence (5-10). Hypotension following spinal anesthesia is more common in pregnant women, which is related partly to the cephalad dissemination of topical analgesics in subarachnoid space and partly to the pressure imposed on aortocaval by the uterus of the pregnant woman (11-14).
Spinal anesthesia is done in the sitting and lateral positions, each of which has advantages and disadvantages (15, 16). Spinal anesthesia in pregnant women is easier in the sitting position due to the obesity and unclear landmarks but keeping the sitting position is very difficult for some patients (like those who received sedatives, emergency patients, multiple pregnancies, umbilical cord prolapse, and restless patients). In these cases, placing the patient in the lateral position is more suitable. Therefore, it is important to know how the patient's hemodynamic status changes after spinal anesthesia in the lateral position (16, 17).
Sympathectomy caused by spinal anesthesia, along with intensifying the peripheral blood accumulation caused by gravity, leads to considerable hypotension in the sitting position (15, 18). Hypotension creates problems for the mother and fetus, including vomiting, nausea, and dizziness in the mother and acidemia in the fetus (19-21). According to the above explanation, in theory, spinal anesthesia in the lateral position may be associated with less hypotension. Various studies have been conducted in this regard with different results about the incidence of hypotension and onset time of anesthesia in the sitting and lateral positions for the cesarean section (16, 17).
2. Objectives
This randomized study was conducted to compare the effect of spinal anesthesia in the sitting and lateral positions on the onset time of sensory block and hemodynamic condition in the cesarean section.
3. Methods
3.1. Study Population
This clinical trial was conducted after approval by the Ethics Committee of Hamadan University of Medical Sciences (IR.UMSHA.REC.1397.414 and IRCT 20120915010841N13) and obtaining written informed consent of patients in Fatemieh Hospital, Hamadan. Data collection tools included a researcher-made questionnaire in agreement with the research goals and variables. A convenience sampling method was used to form a sample of 106 patients (53 patients in each group). Patients were selected from among cesarean section candidates under spinal anesthesia who met the inclusion criteria. The inclusion criteria were 18-45-years-old, ASA class 1 or 2, not suffering from diabetes, hypertension, cardiac diseases, kidney diseases, eclampsia, pre-eclampsia, and spinal anesthesia contraindications (increased ICP, shock, coagulation problems, and anemia). The exclusion criteria were lack of consent to participate in the study, an emergency cesarean, multiple pregnancies, and failed spinal anesthesia.
3.2. Study Design
The sample size was calculated with a 0.05 alpha, 0.8 power, 34% P1, and 56% P2 (incidence of hypotension in spinal anesthesia in the sitting and lateral positions based on ref. No. 28). Finally, a total of 106 women were included in two groups, including 53 subjects in the sitting position (group S) and 53 subjects in the lateral position (group L). Patients were divided randomly into two groups. Randomization was carried out by block randomization using quadruple blocks. We choose a block at random, and the first four treatments were allocated according to the block. Then, a new block was chosen at random, and the next four treatments were allocated. We kept going until the required sample size was collected. To blind the study, an anesthesia resident performed spinal anesthesia in the sitting and lateral positions (according to randomization), and an anesthesiologist who was unaware of the randomization and classification of the groups collected information.
In all patients, 10 ml/kg Ringer solution was injected by a peripheral venous catheter no.18 after entering the operation room, and systolic and diastolic blood pressures, mean arterial pressure, heart rate, and initial SpO2 of patients were measured by a non-invasive monitoring system (Saadat, Novin S1800 model, Iran). Then, patients in groups S and L underwent spinal anesthesia with a 25 gauge Quincke needle (Mekon Medical Devices Co. Shanghai, China) at the L3-L4 space in the midline in the sitting and left lateral positions. After Cerebrospinal Fluid (CSF) aspiration, 10 mg hyperbaric bupivacaine 0.5% (2 mL, AstraZeneca, Austria) with 2.5 µg Sufentanil (Sufiject Aburaihan Co., Iran) was injected into the subarachnoid space, and immediately, the patient was placed in the supine position. Then, systolic and diastolic blood pressures, Mean Arterial Pressure (MAP), Heart Rate (HR), and SpO2 were recorded in both groups every two minutes until 10 minutes (minutes 2, 4, 6, 8, and 10), followed by every five minutes until 30 minutes (minutes 15, 20, 25, and 30) and every 10 minutes until 60 minutes (minutes 40, 50, and 60), by a nurse of anesthesia.
The sensory block was evaluated with a pinprick in each minute, and the time of beginning the sensory block (time to reach T6 sensory level) was recorded in the questionnaire. The quality of sensory-motor block in minutes 5 and 10 after spinal anesthesia, ephedrine and atropine doses, nausea and vomiting, and Apgar score of the newborn (minutes 1 and 5) were evaluated and recorded in the questionnaire. After the operation, the satisfaction of the patient was asked (in percent) and recorded. Hypotension was defined as systolic blood pressure lower than 90 mmHg, and 10 mg ephedrine was used to treat it. Bradycardia was defined as a heart rate lower than 60 per minute and treated with 0.5 mg atropine. The Bromage score was used to evaluate the quality of the motor block, and the following scale was used for the quality of sensory block: Painless: excellent, Mild tolerable pain: good, Moderate pain requiring sedatives: acceptable, and Severe pain requiring general anesthesia: poor. On the Bromage scale, 0 = the patient could raise the legs, 1 = the patient could flex the knees, 2 = the patient could move only toes, and 3 = the patient could not move the legs.
The classification of patients based on their physical condition was done according to the guidelines of the American Society of Anesthesiologists (ASA) from class 1 to class 6. A pinprick was used to determine the sensory block by a needle. The satisfaction of patients was determined based on 0 to 100 scores, as follows: < 80%: not satisfied, 80-90%: satisfied, and > 90%: very satisfied.
3.3. Statistical Analysis
Data obtained from completed questionnaires were entered into SPSS-16 software and analyzed. The qualitative data were described as ratios and percentages. An independent t-test was used to compare the mean of systolic and diastolic blood pressures, MAP, HR, and SpO2 in both groups. Repeated-measures analysis of variance was used to compare between different times of measurement. A P value of less than 0.05 was considered statistically significant.
4. Results
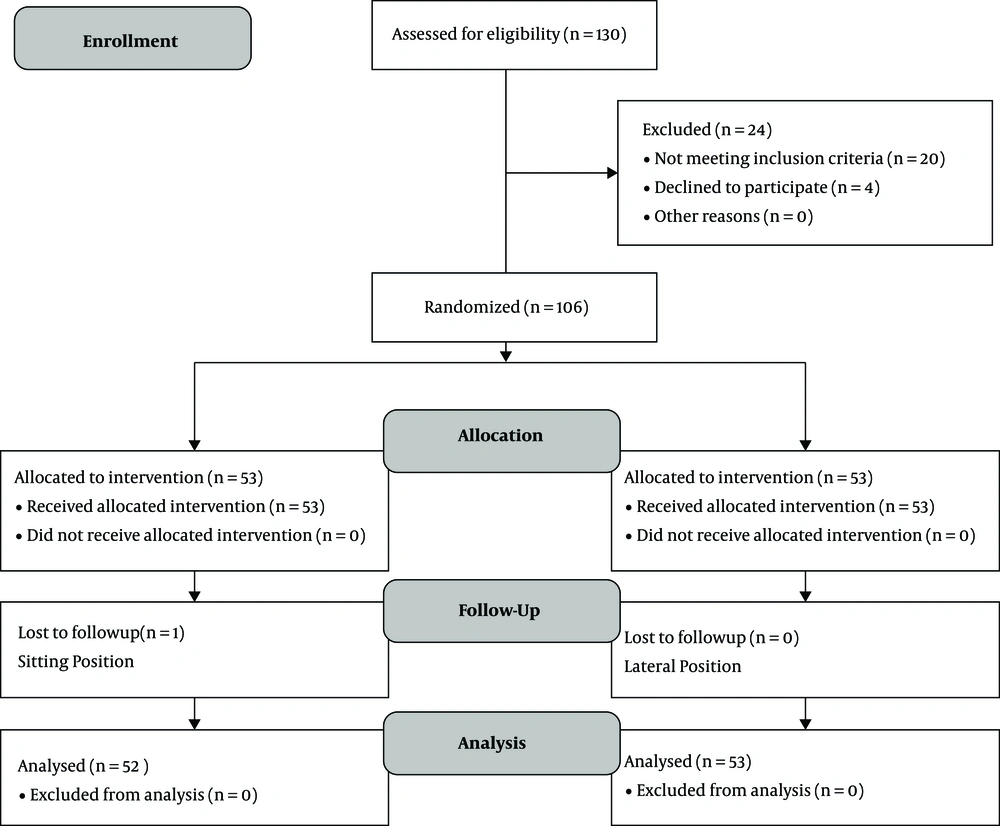
In this research, 106 women, including 53 women in group S (spinal anesthesia in the sitting position) and 53 women in group L (spinal anesthesia in the left lateral position) were studied. One woman was excluded from group S due to failure in spinal anesthesia and repeated spinal anesthesia. Thus, 105 patients in group S (n = 52) and group L (n = 53) were studied (Figure 1).
The mean ages of women in spinal anesthesia in the sitting and lateral positions were 31.00 ± 5.013 and 30.28 ± 6.86, respectively. There was no statistically significant difference between the groups in age.
According to Table 1, mean systolic and diastolic blood pressures and MAP in minutes 6 and 8 after spinal anesthesia were significantly lower in patients in the sitting position than in patients in the lateral position (P < 0.05). Based on Table 2, the mean SpO2 in minutes 6 and 8 after spinal anesthesia was significantly lower in patients in the sitting position than in patients in the lateral position (P < 0.05). Hence, the mean heart rate in both sitting and lateral positions 60 minutes after spinal anesthesia showed no significant difference. In minutes 6 and 8 after spinal anesthesia, the frequency of hypotension in patients under the cesarean section with spinal anesthesia in the sitting position was significantly higher than that in patients in the lateral position (P < 0.05). Regarding Table 3, in patients under spinal anesthesia in the lateral position, the mean onset time of sensory block (time to reach the sensory level of T6) was significantly lower (P < 0.001), and the mean motor block score in minute 5 was higher (P = 0.04) when compared to patients in the sitting position. There was no statistically significant difference between the two groups in the motor block score in minute 10.
| Measurement Time | Systolic Blood Pressure (mmHg) | Diastolic Blood Pressure (mmHg) | MAP (mmHg) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| S Group, Mean ± SD | L Group, Mean ± SD | P Value | S Group, Mean ± SD | L Group, Mean ± SD | P Value | S Group, Mean ± SD | L Group, Mean ± SD | P Value | |
| Before spinal anesthesia | 121.87 ± 10.82 | 125.30 ± 11.79 | 0.123 | 75.51 ± 11.26 | 78.98 ± 09.98 | 0.096 | 89.83 ± 11.10 | 93.56 ± 08.90 | 0.059 |
| After spinal anesthesia | 119.65 ± 13.72 | 120.32 ± 14.08 | 0.806 | 71.77 ± 14.82 | 71.92 ± 14.53 | 0.957 | 87.08 ± 14.01 | 86.09 ± 14.48 | 0.726 |
| Minute 2 | 105.44 ± 18.18 | 102.55 ± 18.39 | 0.419 | 61.60 ± 16.58 | 61.92 ± 16.36 | 0.919 | 74.73 ± 16.26 | 75.32 ± 15.77 | 0.851 |
| Minute 4 | 96.44 ± 17.45 | 94.68 ± 17.50 | 0.919 | 56.46 ± 16.21 | 57.23 ± 13.56 | 0.794 | 68.48 ± 15.70 | 68.79 ± 13.93 | 0.915 |
| Minute 6 | 93.83 ± 16.57 | 102.24 ± 17.04 | 0.012a | 52.50 ± 11. 70 | 59.72 ± 14.46 | 0.006a | 65.83 ± 15.40 | 72.00 ± 16.64 | 0.022a |
| Minute 8 | 100.58 ± 17.65 | 109.08 ± 14.20 | 0.008a | 55.65 ± 15.07 | 61.94 ± 13. 72 | 0.027a | 69.94 ± 15.40 | 76.72 ± 13.70 | 0.019a |
| Minute 10 | 108.79 ± 14.09 | 109.26 ± 12.08 | 0.853 | 60.21 ± 14.50 | 60.04 ± 10.79 | 0.945 | 75.00 ± 15.29 | 75.47 ± 10.69 | 0.855 |
| Minute 15 | 109.35 ± 14.34 | 110.81 ± 13.06 | 0.585 | 59.36 ± 11.84 | 59.72 ± 12.31 | 0.882 | 75.77 ± 13.34 | 76.04 ± 12.52 | 0.915 |
| Minute 20 | 109.09 ± 14.80 | 109.49 ± 11.97 | 0.881 | 57.67 ± 12.27 | 58.23 ± 09.22 | 0.794 | 73.44 ± 12.04 | 74.08 ± 09.29 | 0.763 |
| Minute 25 | 107.69 ± 15.37 | 106.85 ± 08.50 | 0.728 | 56.31 ± 10.35 | 56.62 ± 09.07 | 0.869 | 72.94 ± 13.15 | 71.96 ± 08.73 | 0.653 |
| Minute 30 | 109.46 ± 12.56 | 107.08 ± 09.69 | 0.278 | 56.63 ± 11. 18 | 56.23 ± 08.62 | 0.834 | 73. 73 ± 11.58 | 71. 92 ± 09.22 | 0.378 |
| Minute 40 | 109.04 ± 11.05 | 108.54 ± 08.72 | 0.798 | 56.67 ± 09.55 | 57.19 ± 07.09 | 0.754 | 72.88 ± 09.49 | 72.90 ± 07.32 | 0.991 |
| Minute 50 | 108.53 ± 09.44 | 108.37 ± 08.32 | 0.917 | 56.88 ± 08. 94 | 57.40 ± 06.89 | 0.741 | 71.47 ± 13.09 | 73.27 ± 06.99 | 0.384 |
| Minute 60 | 108.76 ± 07.82 | 108.98 ± 08.15 | 0.888 | 57.16 ± 07.64 | 59.71 ± 07.09 | 0.085 | 73.33 ± 08.10 | 75.33 ± 06.57 | 0.131 |
Comparison of Systolic, Diastolic, and Mean Arterial Pressure in Sitting and Lateral Groups Based on Measurement Time
| Measurement Time | SpO2 (%) | Heart Rate (Per Minute) | Hypotension (Number of Patients) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| S Group, Mean ± SD | L Group, Mean ± SD | P Value | S Group, Mean ± SD | L Group, Mean ± SD | P Value | S Group (n) | L Group (n) | P Value | |
| Before spinal anesthesia | 97.02 ± 1.27 | 97.64 ± 1.29 | 0.121 | 93.51 ± 16.42 | 94.63 ± 14.84 | 0.713 | ̱ | ̱ | ̱ |
| After spinal anesthesia | 97.43 ± 1.39 | 97.83 ± 1.28 | 0.131 | 95.54 ± 17.51 | 100.13 ± 16.17 | 0.165 | 1 (1.9) | 0 (0) | 0.495 |
| Minute 2 | 97.67 ± 1.39 | 98.04 ± 1.34 | 0.17 | 94.40 ± 24.97 | 93.72 ± 20.08 | 0.877 | 11 (21.2) | 17 (32.1) | 0.206 |
| Minute 4 | 97.78 ± 1.38 | 98.19 ± 1.32 | 0.129 | 9.261 ± 22.38 | 94.98 ± 22.58 | 0.591 | 26 (50) | 25 (47.2) | 0.772 |
| Minute 6 | 97.69 ± 1.59 | 98.32 ± 1.25 | 0.026a | 92.04 ± 24.32 | 95.60 ± 19.84 | 0.412 | 30 (57.7) | 13 (24.5) | 0.001a |
| Minute 8 | 97.63 ± 1.52 | 98.36 ± 1.16 | 0.007a | 95.83 ± 22.70 | 98.02 ± 18.60 | 0.589 | 19 (36.5) | 3 (5.7) | 0.001a |
| Minute 10 | 97.67 ± 1.53 | 98.23 ± 1.44 | 0.059 | 98.90 ± 17.15 | 97.47 ± 19.69 | 0.692 | 4 (7.7) | 2 (3.8) | 0.387 |
| Minute 15 | 97.83 ± 1.41 | 98.23 ± 1.34 | 0.137 | 100.27 ± 20.16 | 98.47 ± 17.56 | 0.627 | 3 (5.8) | 0 (0) | 0.118 |
| Minute 20 | 97.79 ± 1.36 | 98.23 ± 1.37 | 0.103 | 99.52 ± 19.84 | 99.11 ± 15.89 | 0.908 | 5 (9.6) | 0 (0) | 0.027a |
| Minute 25 | 97.79 ± 1.44 | 98.24 ± 1.33 | 0.093 | 101.23 ± 16.57 | 98.34 ± 14.62 | 0.345 | 4 (7.7) | 1 (1.9) | 0.205 |
| Minute 30 | 97.85 ± 1.42 | 98.23 ± 1.39 | 0.169 | 100.09 ± 17.76 | 98.79 ± 13.70 | 0.674 | 3 (5.8) | 1 (1.9) | 0.363 |
| Minute 40 | 97.90 ± 1.33 | 98.17 ± 1.44 | 0.324 | 100.36 ± 14.05 | 97.81 ± 14.53 | 0.364 | 1 (1.9) | 0 (0) | 1 |
| Minute 50 | 97.90 ± 1.33 | 98.23 ± 1.32 | 0.211 | 99.04 ± 13.23 | 96.09 ± 11.68 | 0.234 | 0 (0) | 0 (0) | 0.211 |
| Minute 60 | 98.04 ± 1.17 | 98.19 ± 1.34 | 98.19 ± 1.34 | 96.14 ± 11.07 | 93.85 ± 11.85 | 0.317 | 0 (0) | 0 (0) | 0.559 |
Comparison of SpO2, Heart Rate, and Hypotension in Sitting and Lateral groups Based on Measurement Time
| Variable | Sitting | Lateral | P Value |
|---|---|---|---|
| Onset of sensory block | 4.54 ± 2.12 | 1.30 ± 0.43 | < 0.001 |
| Motor block in minute 5 | 2.82 ± 0.52 | 2.98 ± 0.14 | 0.044 |
| Motor block in minute 10 | 2.90 ± 0.36 | 3.00 ± 0.00 | 0.058 |
Comparison of Onset of Sensory Block and Motor Block Score in Minutes 5 and 10 in Sitting and Lateral groups
According to Table 4, the mean ephedrine dose in patients under spinal anesthesia in the sitting position (11.59 ± 10.99) was significantly higher than that in patients in the lateral position (16.92 ± 11.94) (P = 0.010). There was no statistically significant difference between the two groups in terms of atropine dosage. There was also no significant difference in patients under spinal anesthesia in the sitting and lateral positions in terms of the frequency of nausea and vomiting, the maximum height of sensory block, and the mean time of returning to the T10 sensory level.
| Variable | Sitting | Lateral | P Value |
|---|---|---|---|
| Ephedrine | 16.92 ± 11.94 | 11.51 ± 10.99 | 0.010 |
| Atropine | 0.134 ± 0.10 | 0.153 ± 0.15 | 0. 467 |
Comparison of Ephedrine and Atropine Doses in Sitting and Lateral Groups
The mean Apgar score of the newborn in minutes one and five in the sitting and lateral positions was similar, and there was no significant difference (8.90 ± 0.36 in minute one compared to 9.88 ± 0.38 in minute 5). The satisfaction of women under spinal anesthesia in the lateral position was significantly higher than in the sitting position (P = 0.001). There was no significant difference between the two groups in terms of sensory and motor block quality, and both groups were the same.
5. Discussion
This study aimed at comparing the effect of spinal anesthesia in the sitting and lateral positions on the onset time of the sensory block and hemodynamic condition in C/S. In the current study, mean systolic and diastolic blood pressures, Mean Arterial Pressure (MAP), and SpO2 of patients under spinal anesthesia in the sitting position in minutes 6 and 8 after anesthesia were significantly lower than those of patients in the lateral position. The onset time of the sensory block was lower in the lateral position than in the sitting position.
Satisfaction with spinal anesthesia in the lateral position was significantly higher than that in the sitting position, but there was no statistically significant difference between the groups in terms of heart rate, quality of sensory and motor block, the maximum height of the sensory block, mean atropine and ephedrine doses, frequency of nausea and vomiting, and mean Apgar score in minutes 1 and 5.
The study by Muhammad et al. (22), which was performed on 130 pregnant women undergoing cesarean sections under spinal anesthesia using hyperbaric bupivacaine in the sitting and lateral positions, showed that the occurrence of hypotension in the lateral position was significantly less frequent than that in the sitting position (30.7% vs. 52.3%). The findings of this study about the incidence of hypotension in minutes 6 and 8 after spinal anesthesia are consistent with the results of Muhammad et al. study.
In Ortiz-Goez et al. study (23) of 252 pregnant women candidates for elective cesarean sections under spinal anesthesia in three positions of sitting and lateral (right and left sides), the incidence of hypotension was 50.7% in the sitting position, 60% in the lateral position (left side), and 69.2% in the lateral position (right side). There was no difference between the three groups regarding the incidence of hypotension and the need to use vasopressin (ephedrine or phenylephrine). In the current study, the mean ephedrine dosage in women under spinal anesthesia in the sitting position was significantly higher than that in women in the lateral position.
A randomized clinical trial conducted by Atashkhooei et al. (24) about the effect of women’s positions during spinal anesthesia in the cesarean section on hemodynamic condition showed that there was no statistically significant difference between both groups, as the current study and hypotension was significantly lower in the lateral position than in the sitting position. The study by Chevuri et al. (25) on 40 pregnant women candidates for elective cesarean sections under spinal anesthesia in the sitting and lateral positions indicated that the onset time of the sensory block in the sitting position group in minutes 1 and 5 had a delay when compared to the lateral position group, but there was no significant difference in the quality and level of the sensory block between both groups. There was also no significant difference in hypotension incidence and satisfaction between both groups. Consistent with Chevuri et al. study (25), the onset time of the sensory block in the lateral position was lower than that in the sitting position in our study, but the satisfaction of women in this group was also higher than that of women in the sitting position.
In a study conducted by Inglis et al. (26) on 40 pregnant women candidates for cesarean sections under spinal anesthesia in the lateral and sitting positions, the sensory block up to T6 developed faster in the lateral group than in the sitting group. The maximum block height, motor block, and hemodynamic condition in both groups showed no difference. Consistent with the Inglis et al. study, the sensory block up to T6 formed faster in the lateral position than in the sitting position in our study. Contrary to our study, in a study conducted by Xu et al. (27), there was no significant difference in hypotension incidence and mean arterial pressure reduction between pregnant women candidates for elective cesarean sections under spinal anesthesia in the sitting and lateral positions. Consistent with Obasuyi et al, study (28), hypotension occurred less frequently in the lateral than the sitting position but the onset of hypotension was similar between the two groups.
In Shahzad et al. study (16) of 70 patients older than 60 years (male and female) who were candidates for lower abdomen and pelvis surgery under spinal anesthesia in the sitting and lateral (right) positions, the two groups were similar in the heart rate, systolic and diastolic blood pressures 20 minutes after spinal anesthesia, but contrary to our study, the onset time of anesthesia was faster in the sitting position group. Patients felt more comfortable in the lateral position and were more satisfied.
Hallworth et al. (29), in a study of the effect of baricity and position of the patient on the dissemination of bupivacaine on 150 pregnant women candidates for elective cesarean sections under spinal anesthesia in the sitting and lateral positions showed that in the lateral position, Trendelenburg positioning did not affect the sensory block when compared to the sitting position. In our study, the mean onset time of the sensory block in the lateral position was significantly lower and satisfaction was significantly higher than those in the sitting position.
Manouchehrian et al. (30) studied the effect of hemodynamic changes from the lateral position (left side) to the sitting position before spinal anesthesia on hypotension incidence during surgery in 63 patients who were candidates for cesarean sections under spinal anesthesia. This study showed that systolic blood pressure in the lateral position was lower than that in the sitting position. The increased range of changes in systolic blood pressure from the lateral to sitting position before performing spinal anesthesia showed higher hypotension during the cesarean section that could act as a predictor for hypotension after spinal anesthesia. In this study, contrary to our study, systolic blood pressure in the lateral position before spinal anesthesia was lower than that in the sitting position.
The strengths of the present study included the sufficient sample size, evaluation made by the researcher (evaluation was not dependent on patient's response), and accurate monitoring of the patient's hemodynamics. The limitations of this study included the lack of cooperation of some patients in establishing the correct position or participating in the study.
5.1. Conclusion
Cesarean sections under spinal anesthesia in the lateral position lead to a more rapid sensory and motor block, reduced ephedrine consumption, and enhanced satisfaction of women when compared to spinal anesthesia in the sitting position.