1. Background
Coronavirus disease 2019 (COVID-19), the disease caused by a strain of the coronavirus family, was first identified in Wuhan, China, in December 2019. It rapidly spread to most countries all over the world. There have been more than 116 million laboratory-confirmed cases and more than 2.5 million deaths caused by the COVID-19 pandemic (1).
COVID-19 is a multisystem inflammatory disease and has a wide spectrum of severity, ranging from mild to severe and critical illness. Patients may experience fever, cough, headache, diarrhea, or serious complications such as cytokine storm, acute respiratory distress syndrome, respiratory failure, sepsis, etc. (2-6). In severe cases when respiratory distress is not sufficiently treated by oxygen alone, treatment may proceed to mechanical ventilation in patients experiencing hypoxemia or increased work of breathing (7-9).
According to a review article, 14 - 32% of infected patients develop a critical illness, and 29-89% of patients with COVID-19 require mechanical ventilation support (10). Although critically ill patients with COVID-19 are not the majority of cases, they require more sophisticated care and are at higher risk of death (11). Moreover, in the middle of a pandemic, health care systems face various challenges of which limited availability of resources is important because this limitation can impose a lot of stress on healthcare workers (12).
Early detection of factors that can predict the need for mechanical ventilation can be helpful in several respects; it gives a better understanding of the situation and helps with better management and resource allocation. It also underlines the patients likely to develop unfavorable outcomes and provides opportunities for early interventions in this high-risk group of patients.
2. Objectives
We aimed to identify the factors which can be early predictors of the need for mechanical ventilation in the course of the disease and develop a multivariable model to predict the need for mechanical ventilation during hospitalization.
3. Methods
In this single-center retrospective cohort study, we enrolled 681 patients with COVID-19 admitted to Sina Hospital, Tehran University of Medical Sciences, from February 20 to May 29, 2020. The protocol of this study complied with the Declaration of Helsinki was approved by the Tehran University of medical sciences (IR.TUMS.VCR.REC.1399.005). All included patients were over 18 years of age with suspected COVID-19 symptoms. The diagnosis of COVID-19 was based on a positive result using Real-time polymerase-chain-reaction (RT-PCR) detection for a routine oropharyngeal swab or endotracheal sample specimens. We also enrolled some patients according to the WHO's interim guidance and Iranian national committee of COVID-19 into our study (13, 14), including patients with ground-glass opacity (GGO) alone or GGO accompanied by consolidation in chest computed tomography (CT), along with the history compatible with COVID-19. The algorithm of patient care for individuals presenting with respiratory symptoms to Sina Hospital emergency department has been published before (15).
Patients' demographics, clinical information (history and physical examination), laboratory values, radiologic findings, and outcomes regarding mechanical ventilation were recruited from Sina Hospital COVID-19 Registry (SHCo-19R) (15).
3.1. Study Outcomes
The outcome in this study was the need for mechanical ventilation, which was decided upon after consultation with respiratory specialists on an individualized basis for each patient.
3.2. Statistical Analysis
We expressed descriptive data as median (Inter-Quartile Range) for continuous variables and number (percentage) for categorical variables. Means of continuous variables were compared using independent group t-tests. Proportions for categorical variables were compared using the chi-square test. Univariable and multivariable analyses to identify factors associated with the need for mechanical ventilation from COVID-19 were performed by the multivariable logistic regression modeling. Considering the total number of mechanical ventilation (n = 74) in our study, variables were chosen for the multivariate model based on univariable analysis (P < 0.05). The odds ratio (OR) along with the 95% CI were reported. In multivariable analysis, only six variables were statistically significant that were included in the study model. Other significant variables in univariate analysis were excluded due to collinearity or lack of sufficient data in most cases. For risk stratifying and developing a risk score, the final logistic regression model was used as the method previously described by Sullivan et al. (16). In this regard, all study variables that were significant in the multivariable logistic regression model were considered categorical binary variables (even continuous variables based on the best cut-off value for each variable with the optimal sensitivity and specificity by analyzing the area under the receiver operating characteristic (ROC) curve). For all variables structured as the categorical pattern, the distance between a variable and its base (reference) category in regression coefficient units was equal to the size of the coefficient. To obtain final scores for each risk factor, we needed the constant of the scoring system that corresponded to one point in the risk score system. The point value for each risk factor was calculated by dividing the distance of each risk factor from the base category in regression coefficient units by this constant. The total risk score was obtained by adding up the points for all significant risk factors. The predicted risk associated with each risk score was recalibrated by multiplying it by the ratio of the observed mechanical ventilation rate and was finally rescored as low, moderate, and high risk according to the quartile of the percentage of predicted risk. All statistical analyses were performed using SPSS version 22.0 software (IBM, Armonk, New York), and P < 0.05 was considered statistically significant.
4. Results
A total of 681 confirmed patients with COVID-19 were included in this study. Baseline characteristics and laboratory findings on admission are presented in appendix 1 and 2, respectively. Of the total number of patients, 74 (10.9%) patients needed mechanical ventilation during hospitalization, whereas 607 patients (89.1%) did not. Patients who required mechanical ventilation were significantly older than patients who did not. The median age in the mechanical ventilation and non-mechanical ventilation group were 68.58 ± 14.6 and 56.06 ± 16 years, respectively.
Mechanical ventilation and non-mechanical ventilation groups were significantly different considering respiratory rate on admission, arterial oxygen saturation on admission, white blood cell count, red cell distribution width (RDW), urea, potassium, calcium, phosphorus, magnesium, lactate dehydrogenase, erythrocyte sedimentation rate, C-reactive protein, creatine phosphokinase, aspartate aminotransferase, alanine aminotransferase, ferritin, troponin, and bicarbonate.
Also, there was a significant difference between the two groups considering the history of hypertension, diabetes mellitus, cardiovascular disease, malignancy, lung disease, and cerebrovascular accident. Moreover, patients requiring mechanical ventilation more commonly experienced myalgia and were taking metformin, beta-blockers, and aspirin in comparison to the non-mechanical ventilation group. In contrast, the difference between mechanical ventilation and non-mechanical ventilation groups was not significant in terms of gender, history of transplantation, chronic kidney disease, and CT scan findings.
Multivariate logistic analysis revealed that age (OR, 1.049; 95% CI: 1.008-1.091; P = 0.02), history of diabetes mellitus (OR, 3.216; 95% CI: 1.134 - 9.120; P = 0.028), respiratory rate on admission (OR, 1.051; 95% CI: 1.005 - 1.100; P = 0.031), oxygen saturation on admission (OR, 0.928; 95% CI: 0.872 - 0.989; P = 0.021), CRP (OR, 1.013; 95% CI: 1.001 - 1.024; P = 0.032) and HCO3-level (OR, 0.886; 95% CI: 0.790 - 0.995; P = 0.04) were risk factors for mechanical ventilation during hospitalization (Table 1).
| Coefficient | P-Value (Multivariate) | Odds Ratio (OR) | 95%CI for OR | ||
|---|---|---|---|---|---|
| Lower | Upper | ||||
| Age | 0.047 | 0.020a | 1.049 | 1.008 | 1.091 |
| Gender | - 0.495 | 0.379 | 0.610 | 0.202 | 1.838 |
| Hypertension | - 0.223 | 0.698 | 0.800 | 0.259 | 2.468 |
| Diabetes mellitus | 1.168 | 0.028a | 3.216 | 1.134 | 9.120 |
| Cardiac disease | - 0.998 | 0.098 | 0.369 | 0.113 | 1.200 |
| Lung disease | - 0.885 | 0.242 | 0.413 | 0.094 | 1.819 |
| Respiratory Rate | 0.050 | 0.031a | 1.051 | 1.005 | 1.100 |
| SpO2 | - 0.074 | 0.021a | 0.928 | 0.872 | 0.989 |
| W.B.C | 0.045 | 0.421 | 1.046 | 0.937 | 1.168 |
| Potassium | 0.081 | 0.853 | 1.085 | 0.457 | 2.575 |
| ESR | - 0.014 | 0.147 | 0.986 | 0.968 | 1.005 |
| CRP | 0.013 | 0.032a | 1.013 | 1.001 | 1.024 |
| HCO3- | - 0.121 | 0.040a | 0.886 | 0.790 | 0.995 |
| Constant | 3.949 | 0.320 | 51.861 | ||
Abbreviations: SpO2, peripheral capillary oxygen saturation; WBC, white blood count; ESR, erythrocyte sedimentation rate; CRP, C-reactive protein; HCO3, bicarbonate.
a Statistically significant P-values.
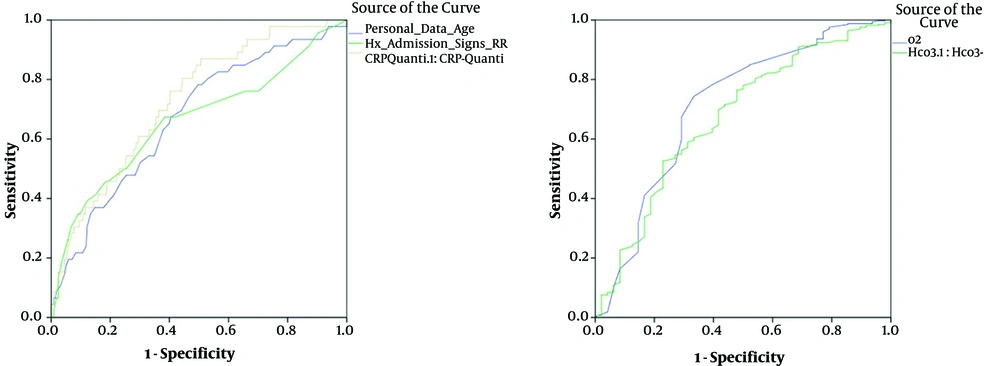
To categorize five continuous variables of age, CRP, HCO3- level, respiratory rate, and oxygen saturation, the area under ROC curve (AUC) was analyzed, yielding the best cut-off values of 55 years for age, 18/min for respiratory rate, 22 mEq/L for HCO3- level, 65 mg/L for CRP, and oxygen saturation less than 85% (Figure 1). The results of ROC analyses showing AUC ≥ 0.650 are outlined in Table 2.
| Parameter | AUC | Lower Limit | Upper Limit | P-Value | Cut-Off | Sensitivity | Specificity |
|---|---|---|---|---|---|---|---|
| Age | 0.670 | 0.587 | 0.753 | < 0.001 | 55 | 80.4% | 53.3% |
| RR | 0.660 | 0.565 | 0.755 | < 0.001 | 18 | 76.1% | 65.7% |
| SpO2 | 0.711 | 0.623 | 0.799 | < 0.001 | 85 | 78.2% | 60.4% |
| CRP | 0.726 | 0.653 | 0.799 | < 0.001 | 65 | 76.1% | 59.8% |
| HCO3- | 0.672 | 0.586 | 0.757 | < 0.001 | 22 | 77.9% | 50.0% |
Abbreviations: RR, respiratory rate; SpO2, peripheral capillary oxygen saturation; CRP, c-reactive protein; HCO3, bicarbonate; AUC, area under ROC curve.
4.1. Construction of a Scoring Model
The risk score included the following parameters on admission: age > 55, a history of diabetes mellitus, a respiratory rate > 18/minute, oxygen saturation < 85%, CRP > 65 mg/L, and HCO3- < 22 mEq/L. The point scores for the obtained risk parameters in the logistic regression analysis are summarized in Table 3.
| Parameter | Risk Score |
|---|---|
| History of diabetes mellitus | |
| Positive | 2 |
| Negative | 1 |
| Decreased oxygen saturation | |
| < 85% | 3 |
| ≥ 85% | 1 |
| Age, year | |
| > 55 | 4 |
| ≤ 55 | 1 |
| Respiratory rate, per minute | |
| > 18 | 4 |
| ≤ 18 | 1 |
| Raised CRP on admission, mg/L | |
| > 65 | 6 |
| ≤ 65 | 1 |
| HCO3-, mEq/L | |
| < 22 | 2 |
| ≥ 22 | 1 |
| Total risk score | 21 |
The total risk score was calculated to be 21, and each risk parameter gets one point if it is not presented to the patient. There are six risk parameters. Thus, the minimum risk score will be 6 for individuals with no pointed risk factors and 21 for individuals older than 55 years, with a positive history of diabetes, with the symptom of tachypnea and decreased HCO3-level and raised CRP on admission. Finally, a total risk score of less than 10, between 10 to 15, and higher than 15 was considered low, moderate, and high risk for mechanical ventilation due to COVID-19, respectively.
5. Discussion
This single-center study analyzed demographic, clinical, laboratory, and radiological characteristics of patients with COVID-19 admitted to Sina Hospital, Tehran, to retrospectively develop a risk score model for predicting the need for mechanical ventilation during hospitalization.
In this retrospective cohort study, 10.9% of patients required mechanical ventilation during hospitalization, while 89.1% did not. We found that patients requiring mechanical ventilation were of advanced age, had more comorbidities (including diabetes mellitus, hypertension, lung diseases, cardiovascular diseases, cerebrovascular accident, and malignancies), and more clinical and laboratory abnormalities.
In the midst of the COVID-19 pandemic, medical resources, including mechanical ventilators, face a significant shortage. According to the challenge of resource scarcity, it is crucial to have a model upon which decisions about resource allocation can be made. Developing a hospital-based risk score can provide clinicians with a valuable tool to stratify the risk of requiring mechanical ventilation during hospitalization.
Using six variables that are either available at hospital admission or can be obtained within the first hours of admission, we developed a clinical risk score to estimate the patient's risk of requiring mechanical ventilation during hospitalization. Age, history of diabetes mellitus, respiratory rate, oxygen saturation, hs-CRP, and bicarbonate level were included in the risk score.
Our findings were compatible with the previous studies, which have shown that advanced age and comorbidities can put the patients at higher risk for developing severe illness and poor prognosis. (2, 17-19) Among comorbidities, diabetes mellitus happened to have the most powerful correlation with the need for mechanical ventilation in our study, which was consistent with previous studies. (20-23)
According to the statistical analysis of the data on admission, we found that fasting blood glucose and Hb.A1c were not significantly different in mechanical ventilation and non-mechanical ventilation groups. Based on these findings, we hypothesize that the diabetes mellitus itself, rather than whether the blood glucose is controlled, can affect the course of the disease. Further studies are warranted to test this hypothesis.
In line with previous studies, we found higher CRP and respiratory rate, and lower oxygen saturation are associated with poor clinical outcomes regarding the need for mechanical ventilation. In fact, CRP is an acute-phase reactant and a marker of inflammation that has been associated with disease progression in MERS, H1N1 influenza, and recently COVID-19. (18, 24-30).
To the best of our knowledge, the relationship of bicarbonate and disease outcome regarding mechanical ventilation in patients with COVID-19 has not been thoroughly studied based on the review of recent literature. In our study, patients who required mechanical ventilation had significantly lower bicarbonate levels on admission. Given that the pH on admission was not significantly different in mechanical ventilation and non-mechanical ventilation groups, we think that the precise amount of serum bicarbonate can be valuable in clinical settings.
Using the risk score, the clinicians can easily categorize patients into low-, moderate-, and high-risk groups. Considering that the risk score is not the only tool in decision making, it can be used to expedite and optimize decisions in the management of patients with COVID-19.
5.1. Conclusions
This study identified the clinical factors that predict the need for mechanical ventilation in adult patients with COVID-19. Based on the findings, as mentioned earlier, we developed a risk score to stratify the risk and predict the need for mechanical ventilation in hospitalized patients with COVID-19. This model, including age, history of diabetes mellitus, respiratory rate, oxygen saturation, hs-CRP, and bicarbonate, can provide the clinicians with an evidence-based tool that can facilitate and support their decision-making in managing patients with COVID-19.
5.2. Limitation
There were several limitations to this study. This single-center study had a modest sample size. Since the data used for developing the risk score were solely obtained from one country, the results' generalizability may be potentially limited. A prospective study seems necessary to validate and confirm the reliability of the risk score.