1. Context
As a result of its rapid global spread, the World Health Organization (WHO) declared coronavirus disease 2019 (COVID-19) as a pandemic on March 11, 2020 (1). To date, there is no known medication or immunomodulatory treatment for COVID-19. Therefore, in order to control the symptoms and protect multi-organ functions, supportive therapy is the priority in the management of critically ill patients (2).
Similar to the prior coronavirus epidemics of severe acute respiratory syndrome (SARS) and Middle East respiratory syndrome (MERS), COVID-19 is a nosocomial infection. According to the Chinese Center for Disease Control and Prevention, healthcare workers account for 3.8% of all COVID-19 cases, with 14.8 percent of these cases being severe or critical (3). Aerosol-generating procedures such as noninvasive ventilation (NIV), a high-flow nasal cannula (HFNC), bag-mask ventilation, and intubation are of particularly high risk in spreading the virus, putting healthcare workers at risk of coronavirus contamination (4). Utilizing appropriate respiratory protection, gloves, face shield, clothing, and paying attention to avoid self-contamination are among the main actions to keep the healthcare workers safe (5).
Hypoxic respiratory failure is expected in nearly 19 percent of COVID-19 patients. In approximately 14 percent of cases, oxygen therapy will be required as a result of a severe infection, and 5 percent will require mechanical ventilation and intensive care unit (ICU) (6). According to the latest information from Wuhan and northern Italy, at least 10 percent of patients admitted to the ICU required emergency tracheal intubation due to profound and unexpected hypoxia (7). Acute respiratory distress syndrome (ARDS) was observed in severe COVID-19 patients treated with mechanical ventilation. The mortality rate associated with ARDS due to other causes ranges from 40 to 60 percent; however, limited information is available to make a reliable conclusion regarding the prognosis of COVID-19 patients who need mechanical ventilation (8).
Accordingly, this review study aimed to collect information from dozens of research studies in order to summarize new guidelines and proper airway management in adult and pediatric COVID-19 patients.
2. Evidence Acquisition
This study aimed to collect essential information on practical recommendations for airway management of adult and pediatric patients with COVID-19, as well as to demonstrate the efficacy and benefits of previous methods in airway management.
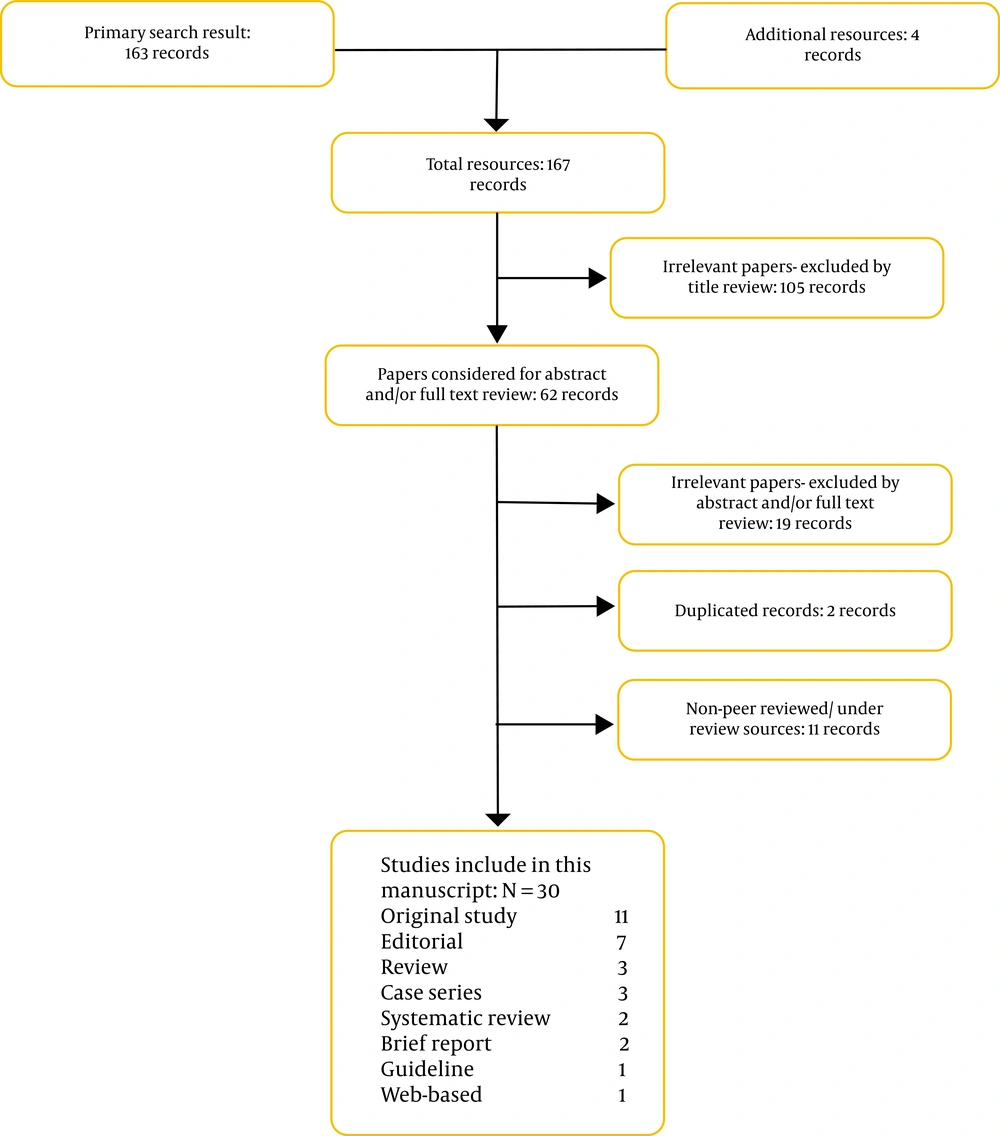
Different techniques for keeping healthcare workers safe during airway management of adult and pediatric patients with COVID-19 were collected by the authors. In this manuscript, we reviewed the published articles and guidelines from the beginning of the pandemic. To do so, the databases including PubMed, MEDLINE, MEDLINE In-Process, and Google Scholar were searched. No date and language restrictions were considered. Information was collected in original research investigations, case series, review articles, correspondence, etc. (Figure 1). The following keywords were used: (1) ‘epidemiology of COVID-19’, (2) ‘hospital care’, (3) ‘signs and symptoms of patients with COVID-19’, (4) ‘airway management for COVID-19 infected patients’, (5) ‘airway management in pediatric patients with COVID-19’, (6) ‘critically ill COVID-19 infected patients’, (7) ‘ICU care for COVID-19 patients’, and (8) ‘safety of healthcare workers fronting COVID-19 patients’. Similar articles, pre-published articles which were not in press, and the articles with unrelated contents in abstract and body were excluded.
2.1. Analysis
The search strategy resulted in 167 articles and guidelines. The irrelevant papers by title review (105) were excluded leaving 62 articles. Then, 30 articles and guidelines were selected for further analysis, including 11 original studies, 7 editorials, 3 review articles, 3 case series, 2 systematic reviews, 2 brief reports, 1 guideline, and 1 web-based study (Figure 1). The remaining 32 articles were excluded due to the following reasons: irrelevant abstracts or full-text review (19 articles), duplicate records (2 articles), and non-peer reviewed/under review sources (11 articles). The characteristics of all the included studies are shown in Figure 1.
3. Results
3.1. Safety of Healthcare Workers During Airway Management
Droplets and fomites are the primary way of COVID-19 transmission. Droplet transmission is resulted from close contact or caused by contamination of fomites (9, 10). COVID-19 is a high-consequence infectious disease that puts healthcare workers and the healthcare system at risk (9). Furthermore, overseeing the patients with severe COVID-19 and conducting aerosol-producing procedures in patients put healthcare workers at an increased risk of infection. Aside from the personal health risks to the infected healthcare workers, the disease and quarantine periods can reduce the existing resources for managing patients at times of high demand.
Throughout the airway management process, enhanced droplet/airborne personal protective equipment (PPE) should be provided to the healthcare workers. A proper airway evaluation prior to airway intervention is of vital importance. Awake intubation should be avoided for patients with normal airway; in addition, modified rapid sequence induction is strongly suggested in these patients. Sufficient muscle relaxant should be ensured before intubation. Proper preparation of airway equipment and detailed intubation plans should be made before airway management in patients with difficult airway (4).
Aerosol-producing procedures, like noninvasive ventilation (NIV), high flow nasal cannula (HFNC), bag-mask ventilation, and intubation, are high-risk procedures (11). In the study by Cheung et al., using NIV or HFNC was not recommended before the patient was cleared of COVID-19. In their work, the following items were among the most important recommendations: (1) endotracheal intubation to be performed by an expert (mainly early intubation for patients with deteriorating pulmonary disease; (2) avoidance of bag mask ventilation until it is needed; (3) optimizing preoxygenation using non-aerosol-generating procedures; and (4) while inserting the endotracheal tube, the cuff is needed to be inflated immediately for no leakage (12).
Hand hygiene, airborne precautions, and the use of PPE should be considered by all medical personnel who treat patients suspected of having COVID-19. The aerosol-producing methods are needed to be done in airborne infection isolation rooms (12). After intubation, double gloving may provide additional protection and reduce the spread of the virus via fomite contamination to the surrounding devices (13).
Healthcare providers should share their knowledge with each other in order to improve the treatment of COVID-19 cases. Orser shared new suggestions regarding self-protection for intubation of suspected or diagnosed COVID-19 cases (Box 1) (5).
| Recommendations |
|---|
| Keep personal protection a priority. |
| Before and after all procedures, hand hygiene should be practiced. |
| Items to wear: fit-tested N95 respirator, face protector such as a shield, gown, and gloves. |
| During patient intubation, the number of healthcare workers in the room should be limited. |
| Intubation should be done by the most experienced available anesthetist. |
| Items to be pre-checked: standard. |
| monitoring, intravenous access, instruments, drugs, ventilator, and suction. |
| Unless specifically indicated, awake fiberoptic intubation should be avoided. Atomized local anesthetic might aerosolize the virus. Using a glidescope or similar device should be considered. |
| Have a plan for rapid sequence induction (RSI), which may need to be adjusted. In case of requiring manual ventilation, small tidal volumes should be applied. |
| To avoid manual ventilation of patient’s lungs and the potential spread of virus from airways, 5 minutes of pre-oxygenation with 100 percent oxygen and RSI techniques should be employed. |
| Make sure that a high efficiency hydrophobic filter is placed between facemask and breathing circuit or between facemask and a self-inflating ventilation bag (e.g., a Laerdal bag). |
| Intubate and ensure the correct position of the tracheal tube. |
| Mechanical ventilation should be instituted, and patient should be stabilized, as appropriate. |
| All airway equipment must be cleaned and disinfected, and hospital policies must be the guideline. |
| After removing protective equipment, touching hair or face should be avoided unless hands are washed. |
| Most anesthesiologists would consider wearing a protective item, such as head covers; however, the use of such items is not yet standardized. |
| For providing rapid feedback to policy makers, it is essential to have an appropriate communication system. |
In addition to an accurate environment and the use of PPE, many modules are available to improve immunity in COVID-19 patients through novel airway management. The virus can be transmitted via intubation (aerosol-based transmission), especially when clinicians are close to the patient’s airway. Fang et al. established a novel, cost-effective, and convenient protection tent to supply a protective barrier between doctors and patients. They believed that this newly designed tent could provide a significantly safer environment for healthcare workers while managing the airway (14).
PPE with positive pressure protective hood is one of the techniques studied for the protection of healthcare workers. In the study by Cai et al., the result of oropharyngeal swab virus nucleic acid was negative in all the participant clinicians with the PPE with positive pressure protective hood (no fever or respiratory symptoms were reported), which could increase the protection of healthcare workers from the virus exposure (15).
In addition to their physical well-being, healthcare workers’ mental health should be prioritized. In the study by Ali et al., 65 percent of anesthesia and ICU physicians who were taking care of patients with COVID-19 had high levels of psychological distress. Similar results were published in a recent study in Wuhan, China, in which 70 percent of healthcare workers had suffered from psychological symptoms (16). One of the major contributors to healthcare workers’ mental stress is the fear of transmitting the disease to their loved ones, as well as a lack of clear protocols for dealing with COVID-19 cases and lack of availability and access to proper PPE (16). One of the other major factors that can cause mental stress in healthcare workers is the lack of human resources. In this regard, Dabbagh et al. suggested that one month of independent work could improve the capabilities of third-year anesthesiology residents. As a result, third-year anesthesiology residents may be able to help the health system recover human resources (17).
3.2. Adults Airway Management in Patients with COVID-19
The main components of COVID-19 management are homeostasis management and the initiation of respiratory support. The role of antiviral medications in the treatment of COVID-19 is unclear. As a result, patients should be isolated with supportive care, and vital signs should be monitored (3).
The most common clinical symptoms of COVID-19 cases are acute hypoxemic respiratory failure (AHRF) caused by bilateral pulmonary infiltrates, which leads to ARDS requiring invasive ventilator support (18). Happy hypoxemia (also referred to as silent hypoxemia), the clinical manifestation in which the patient is awake, calm, and responsive with severe hypoxemia with no evidence of dyspnea and with almost normal lung compliance, is caused by COVID-19; however, the patient’s condition could deteriorate rapidly and without warning. The main step to reverse the hypoxemia is increasing FiO2, which can be done by providing O2 through utilizing a simple nasal prong or facemask (up to 5 - 6 L/minute and up to 10 - 15 L/minute in case of prolonged period of desaturation) (19). Applying prone position can improve ventilation to posterior zones of lung, which leads to improved ventilation-perfusion mismatch (6). High flow rates with nasal oxygen, in turn, result in increased FiO2. For opening the collapsed airways and alveoli, tight-fitting full-face mask, continuous positive airway pressure (CPAP), or helmet can be used to apply continuous positive airway pressure. Therefore, the decision to intubate should be based not only on hypoxemia but also on respiratory distress and fatigue (19).
Intubation and invasive ventilation support are needed in approximately 3.2 percent of COVID-19 cases. These methods are more important than high-flow oxygen treatment and bilevel positive airway pressure (PAP) ventilation in cases of AHRF (both acute and chronic) to increase transpulmonary pressure, open collapsed alveoli, refine oxygenation, reduce oxygen debt, and provide a better opportunity for lung healing (20). Moreover, avoiding the use of advanced respiratory support, in particular noninvasive ventilation and high flow oxygen, can decrease the spread of droplets and infection of clinicians. Radovanovic et al. stated that using a CPAP through a helmet is an effective way for the recruitment of diseased alveolar units and improvement of hypoxemia (18).
For patients with normal airway, the corrected rapid sequence induction using mask ventilation prior to intubation, combined with video-laryngoscopy, has provided rapid tracheal intubation and has been universally successful. A tracheal intubation technique based on rapid sequence induction provided the following benefits in COVID-19 patients: (1) reducing the risk of pulmonary aspiration of stomach contents; (2) facilitating rapid intubation for improving oxygenation and ventilation for making hypoxemia better; and (3) minimizing the time of exposure to patients leading to a reduction in whole exposure to coronavirus (4, 21).
In some recent studies, flexible fiberoptic bronchoscopy was studied in both awake and under general anesthesia patients with COVID-19. The results showed that, compared to mask preoxygenation, less hypoxemia is observed while using high-flow nasal cannula oxygen (HFNO) through flexible fiberoptic bronchoscopic intubation under general anesthesia (21). Moreover, HFNO offers a more rapid intubation length and limited risk of desaturation in tries at fiberoptic tracheal intubation than preoxygenation using facemask ventilation in critically ill patients with COVID-19 pneumonia. HFNO is potentially advantageous in rapid sequence induction and intubation of severe COVID-19 cases. Although HFNO is recommended during intubation for preventing exacerbation of hypoxemia, generally, the use of HFNO is not recommended since it may generate droplets and aerosol (4, 12). Fiberoptic bronchoscopy decreases tracheal intubation-related coughing leading to the spread of the virus. Nonetheless, using neuromuscular blocking agents reduces coughing and increases the probability of intubation success with laryngoscopy (4, 22, 23).
The most appropriate timing for intubation in severe cases is not well-known and might depend on the condition of patients (19). However, according to recent studies, tracheal intubation should be performed in the early stages of illness, whenever possible, to avoid performing the procedure in the presence of severe hypoxemia, which may aid in lowering total mortality in COVID-19 patients. According to Yao et al., tracheal intubation in the early stages of COVID-19 helps to reduce the risk of cardiovascular collapse (during anesthesia and intubation) and lower the risk of pneumothorax. Additionally, large-volume ventilation and the use of hypoxemia-correcting maneuvers immediately after tracheal intubation should be avoided (4, 21).
In patients with maxillofacial trauma, ventilation with a mask and endotracheal intubation may be difficult, in which instability of the cervical spine and airway bleeding could aggravate the condition. Bilateral mandibular fractures can significantly obstruct the airway, preventing fiberoptic bronchoscopy or direct laryngoscopy from being performed. As a result, tracheostomy under local anesthesia is a relatively safe and feasible method. For minimizing the spread of virus, the following preventive strategies should be given consideration: (1) an appropriate depth of anesthesia (prevent coughing); (2) not performing positive pressure and stopping mechanical ventilation immediately before entering the endotracheal tube; (3) reducing the use of suctions during the procedure; and (4) preferring cuffed non-fenestrated tracheostomy tubes (24).
Rahimzadeh et al. discovered a novel finding in terms of intubation length: patients with higher respiratory rates on admission required a longer period of intubation. The respiratory rate and the score of chest CT involvement can be considered as a prognostic factor for estimating the length of intubation and establishing the severity of the illness (2).
3.3. Pediatric Airway Management in Patients with COVID-19
Children of all ages and both genders were sensitive to COVID-19; especially, those who had a history of close contact with an infected person or were in an environment that was suffering from a cluster of COVID-19 outbreak (3). Compared to adults, children with COVID-19 had less severe clinical manifestations; however, as the disease progressed, shortness of breath, cyanosis, restlessness, fatigue, lethargy, and poor feeding, as well as signs of systemic toxicity, could be manifested (3). Nonetheless, young children, mainly infants, were susceptible to COVID-19 (25). While the majority of pediatric patients had a mild or moderate form of COVID-19, the high percentage of asymptomatic infected children highlights the difficulty in identifying pediatric patients who lack clear epidemiological information, which can lead to a dangerous situation in community-acquired infections. In China, the virus transmission without symptoms from children to clinicians was experienced as a serious hazard; viral loads in asymptomatic infants were reported for up to 16 days (26, 27).
Due to the risk of viral exposure to the healthcare workers, several common pre-COVID-19 procedures, such as using mask for general anesthesia for stressful children or transferring children to the operating room, are not desirable. In the midst of the COVID-19 pandemic, the Pediatric Difficult Intubation Collaborative (PeDI-C) developed a number of consensus guidelines for various aspects of pediatric anesthesia care (Box 2). PeDI-C classified difficult airway management methods as following: video laryngoscopy and then fiberoptic intubation by a supraglottic airway device; video laryngoscopy in combination with fiberoptic bronchoscopy; and freehand fiberoptic. In addition, oral fiberoptic intubation was favored against nasal fiberoptic intubation, and it diminished passive oxygenation as tolerated (26).
| Guidlines |
|---|
| Anxiolytic medications administration. |
| Intravenous anesthetic inductions. |
| Video laryngoscope-used tracheal intubation. |
| Cuffed tracheal tubes. |
| Using in-line suction catheters. |
| Performing airway procedures in negative pressure rooms. |
| Allocating sufficient time between surgeries for cleaning of the operating room and air filtration. |
| Transporting mechanically ventilated children with COVID-19 with a ventilator with viral filters on the patient side. |
| COVID-19 patients, in early or recovery phase as well as those under investigation, bypassing the post anesthesia care unit and directly being transferred to the inpatient ward. |
| Using appropriate PPE while performing aerosol-generating procedures in asymptomatic and suspected children. |
4. Discussion
According to data from some European countries, the mortality rate of COVID-19 exceeds one percent, with a fatality rate of 61.5 percent in severe patients, particularly those who were mechanically ventilated (28). In most of the patients, the symptoms are mild, like cough, fever, fatigue, myalgia, and dyspnea; however, the severity of symptoms is different. For instance, in some severe cases, it may lead to respiratory failure or the need for ICU admission for advanced ventilator support. Since there is limited knowledge about the management of COVID-19, it is especially important to broaden learning and information gathering regarding this clinical threat.
Tracheal intubation for invasive mechanical ventilation has been the primary treatment for hypoxemia. Additionally, early intubation should be taken into consideration for patients with deteriorating respiratory condition. Moreover, fiberoptic bronchoscopic tracheal intubation following rapid-sequence induction for COVID-19 cases can lead to a reduction in the risk of viral spread. Video laryngoscopy is suggested not only for healthcare personnel protection but also to allow successful first attempt intubation, thus keeping away potential tracheal trauma and deteriorating respiratory failure (12, 22, 29). According to recent research, HFNO via fiberoptic bronchoscopic intubation is more effective and immune-boosting than standard mask oxygenation in severe COVID-19 cases. All aerosol-generating procedures, including HFNO, noninvasive ventilation, bag-mask ventilation, and intubation, should be performed in an airborne infection isolation room (12, 22).
For pediatric airway management, PeDI-C developed consensus instructions regarding numerous features of pediatric anesthesia care amid the COVID-19 pandemic (26).
5. Conclusions
Physical and mental health of healthcare workers should be considered as a priority during the COVID-19 pandemic. For the physical safety of healthcare workers, hand hygiene, airborne precautions, donning of PPE (and providing adequate amount of PPE) should be considered along with providing proper circumstances for learning and utilizing new methods of protecting themselves against virus contamination. Healthcare workers should be aware of the aerosol-producing methods and the safer alternative methods.
During the pandemic, when choosing an airway management method for COVID-19 patients, not only the patients’ condition, but also the safety of that method for healthcare workers should be considered. As a result, invasive mechanical ventilation in the early stages of the disease is preferred because it spreads less virus.
Finally, standard care and appropriate and early diagnosis and treatment appear to be the most important step in the treatment of critically ill patients with COVID-19 (30).