1. Background
Cardiac surgery is increasing due to coronary artery diseases, the most common cause of death in the Iranian population (1). Patients routinely require arterial or central venous catheters after cardiac surgery to accurately monitor systemic blood pressure, regular blood sampling, medication administration, and intravenous nutrition in the intensive care unit (2-6). These lines (arterial or central venous catheters) remain in place for several days after cardiac surgery, which may result in catheter occlusion (7). Blockade of these catheters can lead to pulmonary embolism and increased morbidity after surgery (8). Catheter locking solutions are appropriate for preventing catheter occlusion (9). In this method, when a catheter is not in use, a fluid (often heparin or normal saline) is injected into the catheter until the subsequent use. Heparin is a sulfated polysaccharide utilized as a clinical anticoagulant (10). Subsequently, it helps to prevent the occlusion of arterial and central venous catheters (2). However, heparin can reduce platelet number and induce thrombocytopenia, bleeding, and allergic reactions (11). Recently, we observed that there were no significant differences between heparinized saline (HS) and normal saline (NS) solutions in preventing the catheter occlusion of arterial and central venous pressure (12). Several studies have confirmed our findings (13, 14). However, the answer to this question is controversial, whether NS solution catheters are a suitable replacement for the HS catheters? Accordingly, to answer this question, this study aimed to investigate the effect of the heparinized and saline solutions of arterial and central venous catheters on complete blood count (CBC) after cardiac surgery.
2. Objectives
The present study compares the effect of heparinized normal saline solution with normal saline solution in central arterial and venous catheters on CBC after heart surgery.
3. Methods
The present double-blind study was registered and approved by the Ethics Committee in Biotechnology Research of Rajai Heart Center of Tehran (RHC.AC.IR.REC.1394.44). In this research, 100 patients with an arterial catheter and central venous pressure monitoring catheter were selected based on the previous studies and after fulfilling the inclusion (18 < age < 65, undergoing coronary artery bypass graft surgery, EF > 40%) and exclusion (dissatisfaction) criteria. The inclusion and exclusion criteria were the same as in our previous study (12). The detailed chart for the selection process is given in Figure 1. Patients were randomized by online randomizer software into two groups, with 50 patients in each group. Group A received heparinized catheters (1 unit/cc normal saline and continuous infusion rates of 3 mL/h under the pressure of 300 mmHg), and group B received normal saline solution catheters. Complete blood count included red blood cell (RBC) count, platelet count, hemoglobin, hematocrit, white blood cells (WBC) differential count, prothrombin time (PT), partial thromboplastin time (PTT), and international normalized ratio (INR) were evaluated in all patients before surgery on the first and second days after surgery. Statistical analysis was performed by the SPSS software version 25.0 (SPSS Inc., Chicago, IL, USA). A t-test was used to compare the means of numerical data. In this test, P-value < 0.05 shows a significant difference in the mean of samples between the two groups, which has 95% confidence.
4. Results
According to the inclusion and exclusion criteria, 100 patients were enrolled and were randomly divided into groups A and B. In this study, patients in groups A and B were studied for age, gender, hypertension, diabetes, and hyperlipidemia before cardiac surgery (Table 1). There were no significant differences in mean age (P = 0.064), gender (P = 0.677), hypertension (P = 0.683), diabetes (P = 0.334), and hyperlipidemia (P = 0.826) between groups A and B. The frequency of the internal jugular catheter was 58% and 54%, and a subclavian catheter was 42% and 44% in groups A and B, respectively. There was no significant difference between the central venous catheter placement (P = 0.84) in groups A and B.
| Variables | Heparinized Saline (%) | Normal Saline (%) | P-Value |
|---|---|---|---|
| Age (y) | |||
| < 40 | 4 (8) | 2 (4) | |
| 40 - 49 | 7 (14) | 4 (8) | |
| 50 - 59 | 17 (34) | 15 (30) | |
| 60 - 69 | 17 (34) | 15 (30) | |
| > 70 | 5 (10) | 14 (28) | |
| Mean ± SD | 56.12 ± 30.32 | 60.12 ± 88.13 | 0.064 |
| Gender | 0.677 | ||
| Female | 31(62) | 33 (66) | |
| Male | 19 (38) | 17 (34) | |
| Hypertension | 0.683 | ||
| Yes | 19 (38) | 31 (62) | |
| No | 29 (58) | 19 (38) | |
| Diabetes | 0.334 | ||
| Yes | 21 (49) | 9 (18) | |
| No | 13 (26) | 41 (82) | |
| Hyperlipidemia | 0.826 | ||
| Yes | 15 (30) | 14 (28) | |
| No | 35 (70) | 36 (72) |
Table 2 shows no significant differences between the CBC, RBC, platelet, hemoglobin, hematocrit, WBC, basophils, monocytes, lymphocytes, PT, PTT, and INR of the A and B groups. CBC analysis showed a decrease in the mean of RBC, hemoglobin, and hematocrit in both groups over time (before the operation to the last day of hospitalization). There were significant differences between RBC (P = 0.0001), hemoglobin (P = 0.0001), and hematocrit (P = 0.0001) on the last day of hospitalization and the day before surgery in group A. However, there were no significant differences in group B.
| Variables | Before | P-Value | First Day | P-Value | Last Day | P-Value | |||
|---|---|---|---|---|---|---|---|---|---|
| Heparinized Saline | Normal Saline | Heparinized Saline | Normal Saline | Heparinized Saline | Normal Saline | ||||
| Platelet | 23420 ± 72108.34 | 21406 ± 63943.66 | 0.146 | 22506 ± 84471.69 | 22312 ± 68291.28 | 0.917 | 221710 ± 83678.81 | 22616 ± 67004.22 | 0.770 |
| Red blood cell | 4.55 ± 0.63 | 4.67 ± 1.46 | 0.596 | 4.30 ± 0.75 | 4.30 ± 0.80 | 0.956 | 4.30 ± 0.73 | 4.33 ± 0.65 | 0.830 |
| Hemoglobin | 13.31 ± 1.72 | 13.69 ± 4.14 | 0.547 | 12.28 ± 2.03 | 12.23 ± 2.13 | 0.906 | 11.73 ± 2.80 | 12.31 ± 1.72 | 0.216 |
| Hematocrit | 8564.20 ± 4468.21 | 42.22 ± 5.27 | 0.442 | 36.05 ± 7.50 | 36.33 ± 6.00 | 0.835 | 35.51 ± 7.43 | 36.59 ± 5.52 | 0.412 |
| White blood cells | 8564.20 ± 4468.21 | 8314.40 ± 2353.90 | 0.732 | 8440.40 ± 3054.83 | 8708.20 ± 22309.83 | 0.628 | 8362.20 ± 2699.16 | 10997.49 ± 14906.24 | 0.222 |
| Basophil | 65.86 ± 10.79 | 63.77 ± 13.55 | 0.343 | 65.31 ± 18.31 | 64.71 ± 15.60 | 0.861 | 66.56 ± 16.90 | 65.31 ± 13.68 | 0.685 |
| Monocyte | 8.43 ± 5.05 | 9.69 ± 7.89 | 0.449 | 13.02 ± 17.90 | 9.38 ± 8.49 | 0.198 | 10.64 ± 12.46 | 8.50 ± 3.28 | 0.243 |
| Lymphocyte | 27.24 ± 9.33 | 25.78 ± 9.94 | 0.399 | 25.82 ± 12.79 | 24.25 ± 9.82 | 0.492 | 24.34 ± 10.73 | 24.30 ± 9.27 | 0.986 |
| Prothrombin time | 15.00 ± 2.76 | 15.89 ± 3.64 | 0.171 | 16.17 ± 3.72 | 16.04 ± 3.44 | 0.850 | 16.57 ± 4.40 | 16.00 ± 3.06 | 0.456 |
| Partial thromboplastin time | 33.53 ± 7.23 | 31.28 ± 9.68 | 0.190 | 37.21 ± 9.16 | 34.47 ± 9.86 | 0.154 | 37.11 ± 11.30 | 34.72 ± 9.43 | 0.253 |
| International normalized ratio | 1.36 ± 0.34 | 1.38 ± 0.42 | 0.749 | 1.54 ± 0.56 | 1.50 ± 0.49 | 0.718 | 2.37 ± 3.46 | 1.50 ± 0.43 | 0.085 |
a Values are expressed as mean ± SD.
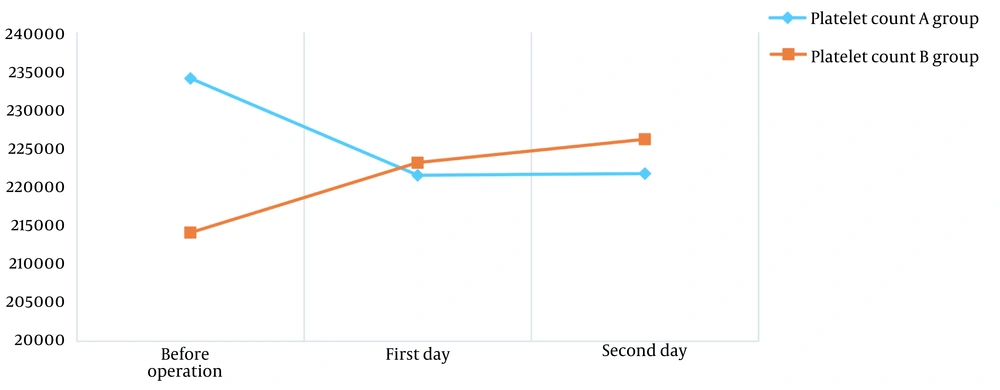
The mean platelet count in groups A and B decreased (P = 0.027) and augmented (P = 0.049) significantly during the study, respectively (Figure 2).
White blood cells, basophil, and monocyte rose, while lymphocyte diminished over time. However, there were no significant differences between WBC (P = 0.923), basophil (P = 0.833), monocyte (P = 0.147), and lymphocyte (P = 0.076) means before the operation and the last day of hospitalization in the A group and WBC (P = 0.252), basophil (P = 0.787), monocyte (P = 0.556), and lymphocyte (P = 0.609) means in the B group.
The means of PT, PTT, and INR were also compared before operation and the last day of hospitalization in groups A and B. All these three variables increased over time in both groups. The increase was more severe in the A group compared to the B group. Comparison of PT, PTT, and INR means over time showed no significant differences between PT (P = 0.814), PTT (P = 0.798), and INR (P = 0.066) means before the operation and the last day of hospitalization in the A group and PT (P = 0.695) and INR (P = 0.656) means in group B. However, there was a significant difference between PTT (P = 0.001) levels on the last day of hospitalization compared to the day before surgery in the B group.
5. Discussion
In cardiac surgery, central venous catheters are widely utilized to monitor central venous pressure and administer fluids, blood products, and medications (15-18). A prolonged period of catheter use may result in catheter occlusion, leading to thrombosis and bloodstream infection (19, 20). Catheter locking by HS and NS solutions can prevent catheter occlusion and maintain cannula patency. The previous studies showed no differences between NS and HS solutions in maintaining the patency of central venous catheters (12, 13, 21). Most previous studies aimed to analyze the efficacy of NS versus HS in maintaining the patency of central venous catheters. Some studies showed NS to be safe and feasible for preventing cannula occlusion (22). On the other hand, HS has known risk factors, including bleeding, allergic reactions, and low platelet count (23). In the present study, no significant differences were observed in terms of CBC, PT, PTT, and INR between patients who received NS and HS solutions. However, comparing CBC before the operation with the last day of hospitalization showed a significant decrease in the RBC, hemoglobin, and hematocrit of patients who received HS. However, in patients who received NS, RBC, hemoglobin, and hematocrit reductions were not significant. This finding may explain the higher bleeding rate in patients who received HS compared to NS. Bleeding is the main side effect of heparin (24). The comparison of platelet count did not show a significant difference between the patients of the two groups in the present study. Del Cotillo et al. compared HS with NS and did not find significant differences in platelet count (25). However, in the current research, postoperative platelet count significantly reduced relative to cardiac surgery in patients who received HS, while it significantly increased in patients who received NS. Decreased platelet count can lead to thrombocytopenia, one of the heparin side effects (11). Ivert et al. compared platelet changes over time (4 - 6 days, one month, and three months after cardiac surgery) by whole-blood flow cytometry in 54 men (26). Their results indicated that platelet count significantly enhanced in the first month after the operation (26). This finding confirms our observed platelet count changes in patients who received NS. Similar to previous studies (25, 27, 28), we found that PTT significantly rose after surgery compared to before surgery in patients who received NS. Accordingly, it can be concluded that NS solution catheters have fewer side effects than HS and can be a suitable replacement for HS catheters.