1. Background
During the last years, there has been an increasing need to perform reform in the content and practice of residency programs (1-3). In the current era of medical education reform, graduate medical education is one of the most influential factors affecting the quality and outcome of care (4, 5). A continuous reform plan is mandated if the improved quality of education is desired. Besides, competitiveness in admission to anesthesiology residency is affected by the quality of medical education and the reform process (6-8).
Department of Anesthesiology and Critical Care (DACC) in Shahid Beheshti University of Medical Sciences (SBMU) is among the eldest academic departments in the School of Medicine (9). Currently, 68 faculty members in this department cover four main categories in the training programs: medical students in their clerkship course and internship course; PhD program students; anesthesiology residency program with 90 clinical anesthesiology residents (year 1 to year 4; CA-1 to CA-4); Six subspecialty fellowship programs (Cardiac anesthesiology, pediatric anesthesiology, pain management, critical care medicine, neuroanesthesia, and regional anesthesia) with a total of 10 fellow candidates.
2. Objectives
In this study, we assessed the effects of the Medical Education Reform program (MERP; September 2016-September 2020) on education and research indices in the residency program, DACC, SBMU; the residency reform was the main part of MERP in SBMU, DACC.
3. Methods
The MERP, DACC, SBMU program was designed and implemented from September 2016 to September 2020, using national successful reform program models in medical education (10-15), targeting both trainees and trainers (faculty members) using the following approaches:
1) Assessment of educational reform area through identifying existing strengths, weaknesses, threats, and opportunities;
2) Discussing opportunities with stakeholders to seek support;
3) Assembling a competent team with a shared understanding of purposes and responsibilities;
4) Selecting and prioritizing reform alternatives;
5) Empowering involved groups in reform;
6) Implementation of reform;
7) Communicating reform process and results with stakeholders;
8) Monitoring and evaluating the reform process and the outcomes.
For performing the above approaches, the main steps were as follows:
1) The initial design of the program within the Executive Council of the Department, consisting of the heads of DACC, SBMU Anesthesiology Wards, and Vice Chairs for Educational Affairs and Research Affairs; this council is the decision-making body of the department.
2) Creating a topic-related steering committee, including a focal point facilitating the workflow of the committee, accompanied by some committee members, usually from faculty members of DACC. In some cases, other technical or consulting people were added. These committees had to develop their roadmap with a defined timetable for assessment, feedback, and reporting the results.
3) The preliminary study included a situation analysis of DACC, a comparative study of pioneer countries, and an adjustment process to define the attainable goals.
4) DACC has defined a global strategic plan 4 years ago. Based on the new challenges and opportunities, this strategic plan was revised and updated.
5) This process was followed by defining main topics for areas of reform activities. These topics were flexible, and changes were possible based on the new situations. The annual meeting of all faculty members was held to report and collaborate in an open environment for all members of the faculty.
6) Continued supervision by auditing bodies of the SBMU, both to improve their contribution and to increase their support.
7) Continued documentation of the whole process.
Areas of reform: the academic staff in clinical departments of medical schools are clinician-educators who are expected to have 4 areas of activities (16-18):
1) Education;
2) Research;
3) Services;
4) Personal and professional development.
However, using the above logic, the reform process was mainly defined in 2 major fields: Education and Research, which included the two other areas.
Based on the above-mentioned process, outcome measures in education and research were determined, and their results were assessed, using the models in previous studies and also based on the results of one or more previous research findings in the same research environment (1, 19-22), leading to nine education indices and three research indices:
Education Indices:
Passing comprehensive exams (23, 26-29);
Assessment methods (24, 28, 29);
Professionalism in medical education (28, 32);
Integration in education (31, 33-35);
Crisis management (32);
Competency-based medical education (study in progress).
Research Indices:
Targeted research activities (31, 33, 36);
Innovation in research approaches (33, 34, 37).
Increasing the impact of research (35, 38-41).
For the measurement of each index, the related research was assessed; the outcome was defined, and the effects of each intervention were summarized in Tables 1-3.
| Modality | Intervention | Affected Domain | Outcome | Reference |
|---|---|---|---|---|
| Teaching method | Integrating interactive teaching to the traditional didactic method | The satisfaction of the trainee | Increased trainee satisfaction | (23-25) |
| Passing comprehensive exams | 1) Mentorship; 2) programmed assessments; 3) modified models of assessment; 4) inventing novel models | Improved results in the National Board Exam | Increased RAPR | (23, 26-29) |
| Mentorship | 1) Trainee satisfaction; 2) theoretical, clinical, and professional achievement of the trainee | Improvements in all 3 fields | (26, 27) | |
| Assessment methods | 1) Empowerment of the faculty; 2) inventing novel models | A shift from summative assessment to formative assessment | 1) Improvement in the trainee satisfaction; 2) improvement in the assessment methods | (24, 28, 29) |
| Faculty development | A comprehensive faculty development program for 24 weeks | The attitudes of the faculty regarding the faculty development program | 1) Positive attitudes of faculty members towards the program; 2) holding a well-designed multilateral academic teamwork, thriving ethical, educational, managerial, and research-related capacities | (30, 31) |
| Professionalism in medical education | Simulation for patient management; simulated patient scenario and role-playing | Professionalism in the trainee | Simulated patient scenario and role-playing are appropriate objective surrogates for OSCE in the assessment of professionalism in the trainee | (28, 32) |
| Integration in education | Integrating basic and clinical sciences | Teamwork for translational academic activities in anesthesiology | 1) Improved cooperation for integration; 2) increased interdisciplinary academic output | (31, 33-35) |
| Crisis management | Independent practice of the residents in COVID-19 crisis | Improved competencies of the third-year clinical anesthesiology residents; including stress management, self-regulated learning, self-esteem and satisfaction in clinical care, disaster and crisis management, and motivational factors | (32) | |
| Competency-based medical education | 1) Introducing the idea to the faculty; 2) creating the culture; 3) developing 14 EPA's | Clinical outcome of medical education (in progress) | In progress | Study in progress |
Abbreviations: EPA, Entrustable professional activity; RAPR, relative annual pass rate = pass rate of SBMU anesthesiology residents/pass rate of the National Board of Anesthesiology.
| Modality | Intervention | Affected domain | Outcome | Reference |
|---|---|---|---|---|
| Targeted research activities | Defining research priorities; defining research fields of interest; defining research teams | Field of interest in research; specialized research process | Improved quality of research; novelty in research areas; publishing in high-impact journals | (31, 33, 36) |
| Innovation in research approaches | Collaboration with basic and clinical departments; integrated thesis and dissertations of clinical anesthesiology residents (CA s); translational research | Quality of research | More in-depth research; translational research articles; improved outcome; group research | (33, 34, 37) |
| Increasing the impact of research | Improving the capacity of faculty and CA’s in publication | Publication of research results | High-impact articles; international books | (35, 38-41) |
| Textbook Title | Publisher | Year | |
|---|---|---|---|
| Dabbagh et al. (38) | Postoperative critical care for adult cardiac surgical patients | Springer International Publishing | 2018 |
| Dabbagh et al. (40) | Congenital heart disease in pediatric and adult patients; anesthetic and perioperative management. | Springer International Publishing | 2017 |
| Dabbagh (35) | Personalized medicine in anesthesia, pain, and perioperative medicine. | Springer International Publishing | 2021 |
4. Results
The results of the study demonstrated improved outcomes regarding the study indices; these topics are mentioned here; however, a full list is mentioned in Tables 1-3.
Educational indices: these indices had significantly improved results: teaching method, passing comprehensive exams, mentorship, assessment methods, faculty development, professionalism in medical education, integration in education, and crisis management; however, the results of outcomes in competency-based medical education are underway and not complete yet. The detailed results are addressed in Table 1.
Research indices: the following research indices had also significant results: “targeted research activities, innovation in research approaches, and increasing the impact of research”. Part of the results is demonstrated in Tables 2 and 3.
5. Discussion
The results of the current study demonstrated that the reform project (MERP) in the Anesthesiology Department has led to tangible outcomes, based on education and research indices within a moderate time interval.
Anesthesiology has been practiced in ancient Iran (Persian Empire) throughout the millennia and referenced by numerous anecdotes, like Shahnameh, the texts of Avicenna, etc. (42-45). Perhaps, the eldest mentioned quote for anesthesia is found in ophthalmic prosthesis related to 3rd Millennium BC in Shahr-e Sukhteh (Burnt City) (43, 46). Besides, Gondishapur School of Medicine and Gondishapur Teaching Hospital were among the eldest academic medical centers worldwide; providing anesthesia care in 309 AD - 379 AD (47). With modern anesthesia practice, the picture is quite different. Introduced by Jakob Eduard Polak in the 1850s (48), anesthesiology and its subspecialties are well developed throughout the country in more than 50 medical schools (49).
The results of this study demonstrated that the 4-year reform project could reach significant results in nearly all study indices.
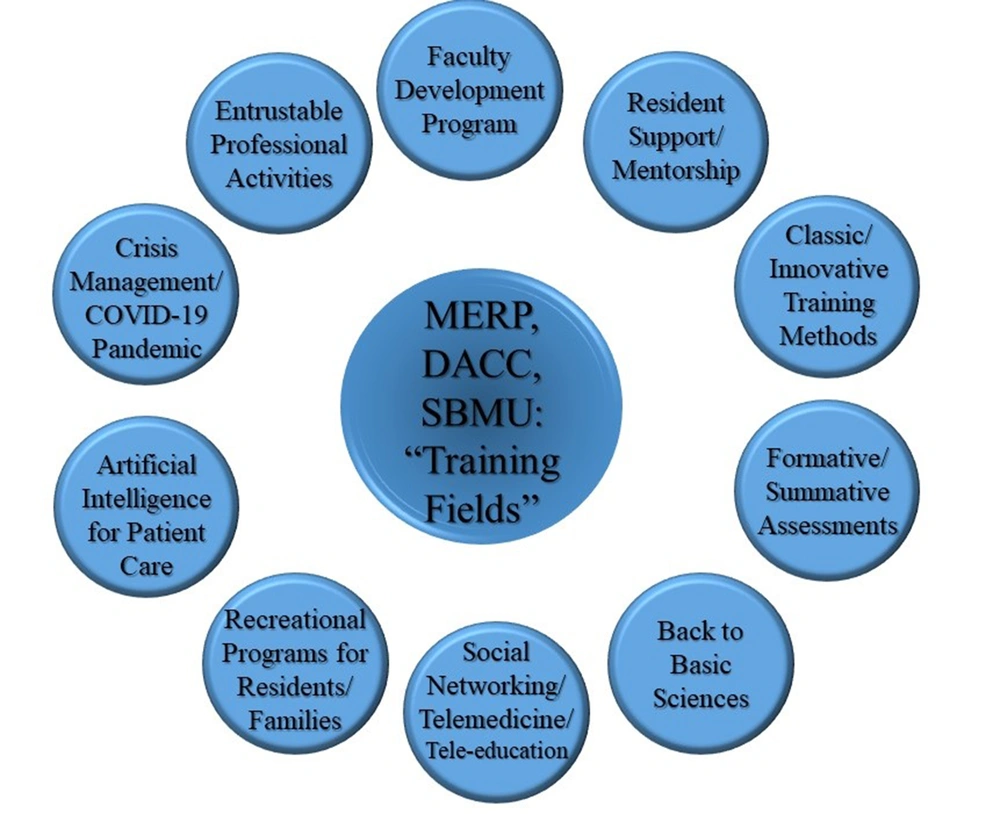
Educational indices: according to the study results, the improvements in the educational indices were significant in nearly all fields; which were in concordance with similar studies in other academic settings (Figure 1). Regarding teaching methods (Didactic vs. Interactive methods), the blended approach (including didactic teaching courses, small group learning, targeted Problem-Based Learning approach, role-playing for residents in simulated case scenarios, tele-education teaching sessions, and other methods used to improve the quality of education and trainee satisfaction showed comparable results with other similar studies in academic settings (23, 25, 28).
Regarding the assessment methods (formative/summative), the significant results obtained after the shift in assessment methods was comparable with other similar academic studies, highlighting the shift from “traditional annual intradepartmental assessment approaches” to a “blended formative and summative model covering the 6 core competencies of the American College of Graduate Medical Education (ACGME)”. Especially, considering the persistent analysis and standard direct perpetual feedbacks to the trainees followed by the assessment process, complementary results demonstrated the unignorable role for developing a scientific approach to formative and summative assessment of clinical anesthesiology residents (CAs), including training workshops, which were held by the DACC for faculty members (26-28, 50, 51). Various assessment methods were applied with their specific applications; however, they are not limited to the following methods (24, 26, 28, 29, 51, 52):
Multiple-choice question workshops;
Role-playing and other simulation methods;
Repeated objective structured clinical exams (R-OSCE);
Direct observation of procedural skills (DOPS);
Internet-based assessment and evaluation of residents.
The results of our study regarding resident support and mentorship programs led to objective improvements in the performance of anesthesiology residents; however, these objective improvements in the residents’ outcome were recorded after junior faculty members passed the Faculty Development programs (FDP), including trainee support techniques (26, 27). This finding was in concordance with the majority of findings in great academic centers (53, 54). The impressive results of our study regarding the effects of the FDP on the junior faculty members, demonstrated that FDPs are a long-term investment in the viability of the department program, especially if the FDP is focused on junior faculty members; a finding compatible with worldwide experiences (30, 55, 56).
Anesthesiology and perioperative medicine cannot be survived without considering the new aspects of medicine, including the current novel OMICS approache used in personalized medicine; the coined name “anesthesiomics” would possibly make more sense in near future (57). This approach is part of the larger approach “back to basic sciences” (34, 37). Our results demonstrated the improved outcomes of this approach in the clinical training of both anesthesiology residents and junior faculty members (23, 30), a finding in concordance with other similar studies (58, 59).
The results of this study demonstrated the role of social networking/application of telemedicine/tele-education in the outcomes of anesthesiology resident education, including social networking, as an approach both in the education of CAs and for supporting them (especially the use of WhatsApp® and Instagram® apps) and also, the role of telemedicine/tele-education as an alternative educational method both before and during the COVID-19 pandemic (25, 60); the latter aspect was specially dealt with during the final period of the study alongside with international experiences. These outcomes are in favor of other similar studies (61-64).
The results of this study regarding the crisis management/COVID-19 Pandemic demonstrated the role of curricular reform plans in these fields with a significant impact on the viewpoints of CA’s (27, 32, 65).
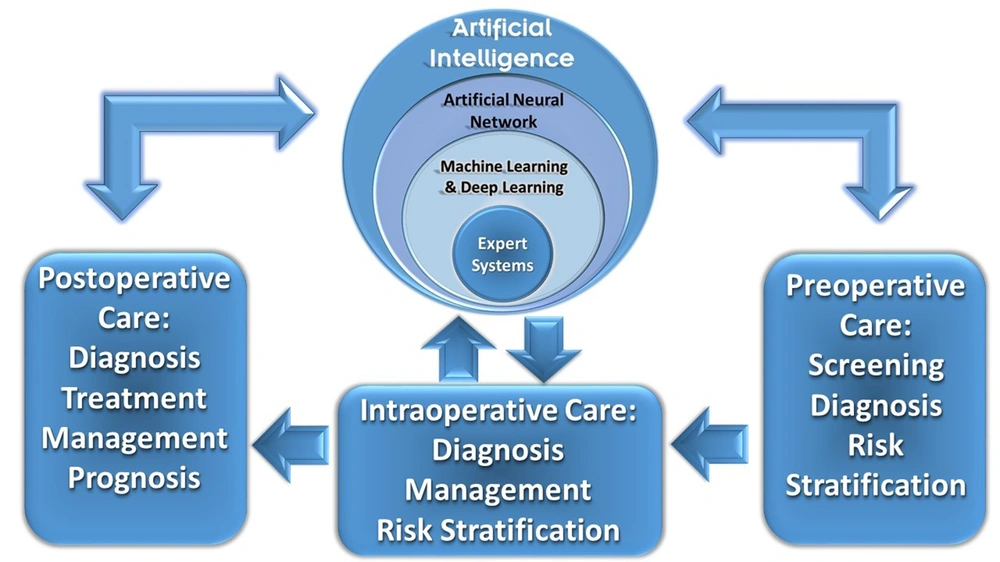
Education outcomes to be assessed in future studies: some important items could be mentioned as the defects of this study, including the role of artificial intelligence (AI) for patient care, the effect of Recreational programs for residents/families, and Entrustable professional activities (EPA) on the outcome of anesthesiology residents’ education. Although these were among the list of interventions in MERP, DACC, SBMU, there has been no assessment regarding their roles yet (66-70); for example, in DACC, SBMU, an inventory AI project has been just proposed with a multicenter future approach; named SAMAB-DACC® (the word SAMAB, is the Persian acronym for Patient Management system and was developed for DACC) (Figure 2) (31).
Patient flowchart in SAMAB-DACC platform with continuous AI interactions (31)
Research indices: the main three strategies used to boost the efficacy, quality, and quantity of research indices were:
1) Targeted research activities;
2) Innovation in research approaches;
3) Increasing the impact of research.
Regarding the first outcome measures (targeted research activities), the study results demonstrated significantly improved indices (i.e. defining research priorities, defining research fields of interest, and defining research teams; Table 2), which were in concordance with similar studies; these indices denote that there has been improved definition for “Field of interest in research” associated with “Specialized research process”, resulting in “Improved quality of research”, “Novelty in research areas” and “Publishing in high-impact journals” (36, 71, 72).
Regarding the second outcome (innovation in research approaches), the study demonstrated significantly improved indices (i.e. collaboration with basic and clinical departments, integrated thesis and dissertations of CAs, and translational research; Table 2); these results are in line with many similar studies on “research innovation” (33, 34, 37, 73-75).
Regarding the third outcome (i.e. increasing the impact of research), The improved indices, including the capacity of faculty and CAs in the publication were in concordance with other similar studies (Table 3) (76-78). The Anesthesiology Research Center, SBMU, in collaboration with DACC, SBMU, and several international colleagues have published an interdisciplinary journal titled: “Journal of Cellular and Molecular Anesthesia” (available at: https://journals.sbmu.ac.ir/jcma/). The journal has been indexed in Scopus, reaching an H index of 5 for 2019 and a Q3 ranking in SCImago Journal Rank portal (scimagojr.com). Besides, several international books have been published through international collaborators, some of which are presented in Table 3 (35, 38-40). The second edition of one of these books in 2018 is worthy of a special mention (39, 41).
5.1. Conclusions
Academic development and reform plans are integral parts of medical education. However, they need painstaking plans and continuous efforts to create improvements. Often, the management period is not durable and these reforms require meticulous care to sustain. However, realistic viewpoints, long-term planning, training, practicing teamwork, and continuous monitoring, and feedback would help reach these ideal goals. Altogether, the faraway viewpoints are promising.
Based on the experiences of DACC, SBMU regarding clinical anesthesiology residency, often the management period is not durable, and these reforms require meticulous care to sustain.