1. Background
Airway management in patients undergoing general anesthesia is a set of actions that result in the creation of a safe and secure airway for ventilation. Failure in airway management and hypoxia can lead to irreversible brain damages within only a few minutes (1, 2).
The prevalence of obesity is rising worldwide, and this is a challenge for specialists in various fields of medicine. There is an inverse correlation between body weight and pharyngeal space (3). This association is significant because excess fat in morbid obesity can influence the pharyngeal spaces, and thus, significantly change laryngoscopic grade (4). Overall, airway management in obese patients can pose numerous challenges as these patients are at a higher risk for difficult airway than normal patients (5). In fact, patients with morbid obesity have excess fat in the mouth, neck, pharynx, thorax, breast, and abdomen, making access to the airway more problematic in various anesthesia situations such as intubation, tracheostomy, or mask ventilation as compared to normal subjects (6, 7). In most studies, an increase in neck circumference was associated with difficult intubation, and a neck circumference over 60 cm was linked with a 35% likelihood of difficult intubation (8). Hence, the possibility of difficult intubation and problems with difficult airways in these patients should be considered, and a solution should be provided. In dealing with difficult airways, assistive devices such as fiberoptic bronchoscope and video-laryngoscope may be used in either awake or anesthetized patients (9, 10). The visibility of the airway and the related structures is imperative for successful intubation (11).
A principal factor leading to difficult intubation is inadequate view during laryngoscopy, and in this regard, improved laryngoscopic view promotes the likelihood of successful intubation, decreases the number of laryngoscopic attempts, and reduces the need for other facilities to manage the airway. Proper positioning before the induction of anesthesia is a key step in successful intubation (12). Numerous studies have emphasized the significance of head and neck positioning, which can have a significant impact on successful intubation and reduce tracheal injury and post-intubation complications (13, 14).
The supine position is not well tolerated in patients with morbid obesity, and fat behind the neck and shoulder girdle makes the head extension position unsuccessful. So much so that the use of the usual 8-cm pillow for intubation is not sufficient and efficient (15, 16). In these cases, the ramped position is more efficient than the sniffing position during laryngoscopy (17). The ramped position can improve glottis view, and thus, facilitate intubation and ventilation in both obese and non-obese conditions (18). This position can be created by using special pre-prepared devices or placing blankets and pillow under the trunk and head of the patient and positioning the body relative to the bed so that the external meatus of the ear and sternum are in a horizontal line (19). Achieving this position is very important, but the strategy can cause problems when the patient is in the position during surgery or even during recovery. Additionally, creating a ramped position with blankets and pillow is time consuming, and using pre-made instruments such as rapid airway management positioner (RAMP), Oxford Head Elevating Laryngoscopy Pillow, and Troop Elevation Pillow is costly (20). Therefore, it seems that finding a simple alternative method that can create a condition similar to the proposed standard conditions in laryngoscopic view provides a suitable solution for the intubation of patients with morbid obesity or patients requiring intubation, especially in emergency situations.
2. Objectives
In this regard, we decided to facilitate the mentioned situation by proposing a new condition with a hand-made device for the positioning of patients with morbid obesity for laryngoscopy and intubation, and due to the structural similarity of this condition with the standard RAMP, we named it the new modified RAMP.
3. Methods
This randomized, single-blind clinical trial was performed among patients who were candidates for bariatric surgery (i.e., gastric bypass surgery, sleeve surgery, or banding) referred to Rasoul Akram Hospital in Tehran in 2020. The inclusion criteria comprised of being aged 18 to 70 years, body mass index (BMI) higher than 35 kg/m2, and being a candidate for bariatric surgery. According to the formula provided by Dixon (21) and first-degree error of 5% and 90% test power, assuming mean 201 and 156 and standard deviation of 56 and 70 for DSP, the sample size was calculated at 42 for each group.
In this regard, patients with a history of difficult intubation, inability to bring the lower jaw forward, short neck, thyromental distance less than 65 mm, restriction of neck movement due to deformity or other problems, facial or neck malformations, and those with the history of ischemic disease, asthma, chronic obstructive pulmonary disease (COPD), or other pulmonary diseases, addiction, obstructive sleep apnea, and Mallampati score greater than 3 were excluded from the trial.
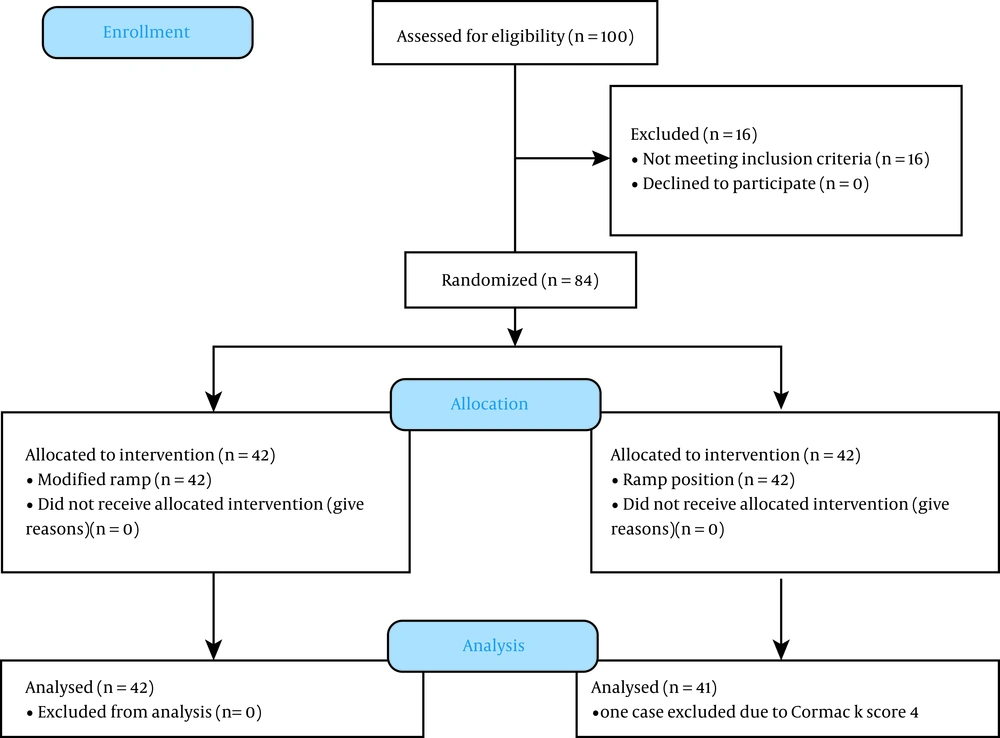
The study protocol was approved by the Ethics Committee of Iran University of Medical Sciences, and it was registered on the Iranian Registry of Clinical Trials website (IRCT20170109031852N5). All the patients provided written consent prior to enrollment. Eighty-four patients were randomly divided (by block randomization method) into the two groups of ramp and modified ramp position (Figure 1).
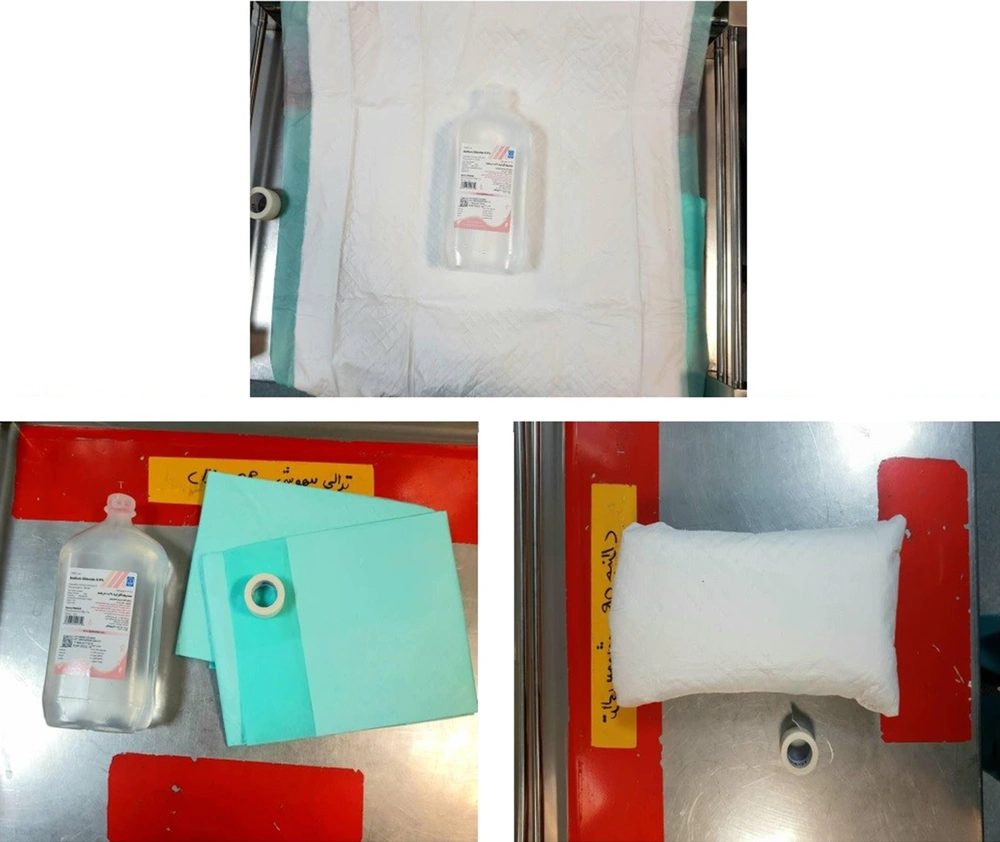
After entering the operating room, intravenous cannulation, and infusion of 5 cc/kg Ringer's crystalloid solution (22), standard monitoring (ECG-POM-NIBP-EtCO2) was established. Then, the patients were placed in their random respective groups. Also, BIS monitoring was established for all the patients, and the BIS number was read and recorded at the time of intubation. In the ramp group, patients were placed in the standard ramp position with the special cloth and towels, and in this case, the bed was in a completely neutral position and had a zero-degree angle with the horizon. In the modified ramp group, for ease, availability, cheapness, and rapid embedding, a one-liter normal saline plastic container in the shape of a rectangular cube with the dimensions of 20 × 12 × 6 cm covered by a double-layer cotton protective sheet was used (Figure 2). The device was placed between the two scapula, at the same time, the bed was set at a 30-degree angle to the horizon (inverted Trendlenberg), and the patient's head was in a neutral position. By placing a pillow under the head, it was also given a height of 8 cm. After the stabilization of patients in the relevant positions, all the patients were premedicated by fentanyl (3 mcg/kg) based on lean body mass (LBM) and midazolam (0.02 mg/kg) based on total body weight (TBW).
For the induction of anesthesia, sodium thiopental (5 mg/kg) based on TBW, succinylcholine (1.5 mg/kg) based on TBW, and lidocaine bolus (1.5 mg/kg) based on IBW were injected for induction. For all the patients, after losing consciousness, oral airway was inserted, and jaw thrust was performed. Following intubation, all the patients received sevoflurane (2%) and cisatracurium (0.03 mg/kg) based on TBW every 30 minutes and fentanyl (50 mcg) every 40 minutes as maintenance. Forty-five seconds after the induction of anesthesia, laryngoscopy was performed by Macintosh blade number 4 and intubated with armored tube supplied by introducer. The patients' laryngoscopic grade was recorded according to the Cormack criteria in both groups at the time of intubation. The patients' ventilation was also evaluated qualitatively and quantitatively by the provider. The following scoring was used to evaluate ventilation before intubation due to the inaccuracy of ETCO2 during mask ventilation and the indirect effect of ventilation on oxygenation. 0: for weak ventilation, O2 saturation less than 90% and/or creating more than 45 cm H2O for ventilation (in these cases, the mask will be taken with both hands); 1: for moderate ventilation (O2 saturation 90% to 95% and/or creating 35 to 45 cmH2O for ventilation), and 2: for easily ventilation (O2 saturation higher than 95% and/or creating 30 to 35 cmH2O for ventilation).
With respect to intubation, the following items were considered and recorded: (1) the number of attempts for successful intubation, (2) duration of intubation (time required for intubation from the time of mask removal from the patient's face to the end of intubation and the appearance of a capnograph wave), (3) saturation rate at the end of intubation, and 4- applying BURP (backward, upward, and rightward pressure) maneuver for intubation. Bispectral index (BIS) was also recorded in the two groups at the time of successful intubation. The Mallampati score of all the patients was recorded before the operation in a sitting position, and in the case of inability to ventilate the patient, laryngoscopy was performed immediately, and in case of inability to intubate, the difficult airway protocol was followed.
All the laryngoscopies were performed by an assistant with at least two years of clinical experience (3rd year of residency). After intubation, the assistant announced the patient’s Cormack score. In addition to recording the demographic information of patients in the required checklist, weight, height, BMI, underlying diseases, and neck circumference from the thyroid cartilage were measured, and data related to ventilation and intubation were also recorded.
In this study, the maximum allowable laryngoscopic attempts (before entering the difficult airway algorithm and using assistance) was considered two times for each patient, and the maximum time for the completion of the laryngoscopic attempt was considered 60 seconds or reducing arterial oxygen saturation below 90%. In this case, with the first unsuccessful laryngoscopy attempt, the patient was ventilated for 10 to 20 seconds until the arterial oxygen saturation reached more than 98%, and then the second laryngoscopic attempt was made. If the second attempt failed or oxygen saturation dropped despite ventilation, difficult airway algorithm was employed.
To analyze the data, SPSS version 25 was used. To describe the data, descriptive statistics, including frequency and percentages (for categorical variables) and mean and standard deviation (for quantitative variables), were used. To examine the hypotheses, the chi-squared test (or Fisher’s exact test if required) was used to compare the categorical parameters, and the Mann-Whitney U test or t-test was used to compare the quantitative parameters.
4. Results
Comparing baseline characteristics and clinical history of patients in the two groups, ramp and modified ramp position (Table 1) indicated no significant differences in gender, mean age, history of underlying disorders (i.e., hypertension, diabetes mellitus, or hypothyroidism), and anthropometric parameters. With regard to scoring considered for ventilation and the number of attempts for laryngoscopy (Table 2), we did not find any differences between the two groups, that is, neither group experienced difficult ventilation, while easy ventilation was reported in 83.3% and 88.1% of the cases in the ramp and modified ramp position groups, respectively (P = 0.533). Also, double attempt for laryngoscopy was recorded in 2.4% and 7.3% of the cases in the ramp and modified ramp position groups, respectively (P = 0.533). Only 21.4% and 26.8% of patients in the ramp and modified ramp position groups, respectively, required maneuver for intubation (P = 0.565). One case in the modified ramp group (a man with BMI of 42.6 kg/m2, neck circumference of 43 cm, TM distance of 65 mm, the Mallampati score of 3, and the Cormack score of 4 with history of hypertension) required difficult airway algorithm. The case was quickly intubated with fiberoptic due to proper and easy ventilation. We found no difference between the two groups in the mean time for intubation (P = 0.385) and arterial oxygen saturation on intubation (P = 0.631; Table 1). The study showed no difference in BIS score during intubation between the ramp and modified ramp groups (41.21 ± 8.04 vs. 41.63 ± 7.99, P = 0.816). As shown in Table 2, comparing the Mallampati score and the Cormack score also indicated no difference between the two groups.
| Item | Ramp Group | Modified Ramp Group | P Value |
|---|---|---|---|
| Clinical history, No. (%) | |||
| History of diabetes | 6 (14.3) | 3 (7.1) | 0.123 |
| History of hypothyroidism | 4 (9.5) | 3 (7.1) | 0.786 |
| History of hypertension | 1 (2.4) | 5 (11.9) | 0.089 |
| Female sex, No. (%) | 38 (90.5) | 39 (92.9) | 0.998 |
| Age subgroups, No. (%) | 0.254 | ||
| 20 to 30 years | 12 (28.6) | 9 (21.4) | |
| 31 to 40 years | 15 (35.7) | 10 (23.8) | |
| 41 to 55 years | 15 (35.7) | 23 (54.8) | |
| Mean age, y | 36.95 ± 9.33 | 40.45 ± 9.90 | 0.099 |
| Mean weight, kg | 120.10 ± 12.40 | 115.63 ± 14.61 | 0.055 |
| Mean height, cm | 162.71 ± 9.44 | 160.73 ± 8.47 | 0.185 |
| Mean body mass index, kg/m2 | 45.46 ± 4.30 | 45.15 ± 5.54 | 0.274 |
| Mean ideal body weight, kg | 55.71 ± 9.05 | 53.69 ± 8.00 | 0.156 |
| Mean neck circumference, cm | 43.61 ± 4.64 | 41.11 ± 4.78 | 0.085 |
Baseline Characteristics and Clinical History of Patients in the Two Groups
| Item | Ramp Group | Modified Ramp Group | P-Value |
|---|---|---|---|
| Ventilation score | 0.533 | ||
| Weak | 0 (0.0) | 0 (0.0) | |
| Moderate | 7 (16.7) | 5 (11.9) | |
| Easy | 35 (83.3) | 37 (88.1) | |
| Number of laryngoscopic attempts | 0.533 | ||
| One | 41 (97.6) | 38 (90.2) | |
| Two | 1 (2.4) | 3 (7.3) | |
| Requiring maneuver | 9 (21.4) | 11 (26.8) | 0.565 |
| Mean time for intubation | 21.30 ± 6.27 | 22.67 ± 7.63 | 0.385 |
| Oxygen saturation on intubation | 97.21 ± 1.85 | 97.39 ± 1.94 | 0.631 |
| BIS score during intubation | 41.21 ± 8.04 | 41.63 ± 7.99 | 0.816 |
| Grade of laryngoscopy | 0.192 | ||
| 1 | 24 (57.1) | 17 (40.5) | |
| 2 | 9 (21.4) | 15 (35.7) | |
| 3 | 9 (21.4) | 9 (21.4) | |
| 4 | 0 (0.0) | 1 (2.3) | |
| Mallampati score | 0.361 | ||
| 1 | 6 (14.3) | 3 (7.1) | |
| 2 | 27 (64.3) | 26 (61.9) | |
| 3 | 9 (21.4) | 13 (31.0) | |
| 4 | 0 (0.0) | 0 (0.0) |
Comparison of Ventilation and Intubation Parameters in the Two Groups
5. Discussion
According to our findings, modified ramp condition was not significantly different as compared to the standard ramp condition in terms of all the intubation and ventilation-related parameters; thus, it can be a good alternative to the standard condition. Based on a review of the literature, this study was the first study to modify the position of the standard ramp and to compare the laryngoscopic grade in the pointed modified condition. In obese patients, increased chest wall fat, especially in the back, increases the posterior anterior diameter of the chest. As a result, it is difficult to use the usual sniffing position in these patients. Due to the high chest to head ratio in obese patients, when lying in the supine position, the head is in a lower position than the chest (23); this problem is solved in both ramp and the modified ramp conditions.
Collins et al. were first to describe the advantages of ramp over sniffing (24). Later studies have shown that ramp position is superior to sniffing in non-obese patients as well as patients with difficult airway. Lee et al., by studying expected difficult airway patients in 2015, concluded that by using ramped position along with good clinical experience, it is easily possible to achieve a proper laryngeal view and success endotracheal intubation (25). However, Semler et al., in contrast to other articles, reported in favor of sniffing and concluded that ramps did not significantly improve oxygenation compared to sniffing. They stated that it might also make it difficult to see the glottis and increase the number of laryngoscopic attempts (17). This inconsistency may be contributed to study design, in the majority of trials, patients were intubated by experienced anesthesiologists on OR beds, while in that study, patients were intubated on ICU beds and by less experienced operators.
Sanaie et al., in 2017, by studying 70 female patients with BMI ≥ 35 during laryngoscopy in ramp position, declared that manual caudal and downward displacement of adipose tissue have a significant impact on the improvement of laryngoscopic view in morbid obese patients (26).
Hasanin et al. in 2020 designed a new pillow to elevate shoulders similar to our study and extend head to the most possible range. They conducted a trial on 60 obese patients scheduled for general anaesthesia and compared ease of laryngoscopy and ventilation in the two groups, and concluded that their pillow facilitates intubation and ventilation in comparison with ramp position. Albeit the need for the insertion of oral airway was marked as difficult ventilation compared to our study design (23). Elevating shoulders and extending the head, according to Hasanin et al. and our study, seems to be the basic rule in airway management in obese patients.
According to the different results, it seems that further studies on the position of patients for intubation are needed.
Faster decline in arterial oxygen saturation in obese patients, along with the higher prevalence of restrictive lung disease, make such patients less tolerant for delayed intubation; therefore, safer and faster intubation plays a prominent role in airway management of these patients (27). The criteria for the possibility of difficult mask ventilation include history of snoring, obstructive sleep apnea, age over 55 years, male sex, beard, BMI over 30 kg/m2, and Mallampati 3 or more (28-30). The possibility of difficult intubation and potential airway management problems must be considered, and preparation should be made for it. High neck circumference and high Mallampati score are some of the most critical parameters in preoperative assessment and reliable predictors of problematic intubation in morbidly obese patients (15).
Obese patients are exposed to both difficult ventilation and intubation. In our study, patients with a history of sleep apnea or snoring and Mallampati score more than 3 were not included in the study.
Due to the lack of access to prefabricated ramps and their high cost, as well as the time-consumingness and the need to change the construction of ramps with the sheets and towels in the operating room, the use of other available methods, while being cheap and easy-to-use, can facilitate the airway management of obese patients. In the absence of prefabricated ramps for proper placement in the ramp position, there is a need for multiple trials and errors in the number and manner of placing towels and sheets in the operating room. It requires the patient to be positioned several times, and the removal of these towels from under the intubated patients can be very dangerous to the patients and even operating room personnel (31).
In our trial, there was no difference in intubation time and the time required for intubation between the ramp and modified ramp conditions. In a 2008 study, Rao et al. found that the position of the ramp and the position of raising the head by 25 degrees by changing the position of the surgical bed for the intubation of obese patients had similar results in terms of laryngoscopic quality and intubation time, which was similar to our finding (31).
In 2012, Lebowitz et al. (32), after studying the laryngoscopic view of 189 obese patients in both ramp and sniff positions, concluded shoulder and head elevation by any means that brings the patient's sternum onto the horizontal plane of the external auditory meatus maintains or improves laryngoscopic view significantly. In our study, patient’s shoulders position was similar to their study.
The advantages of the proposed modified ramp position are quick. And easy construction, cheap and available equipment, the use of the surgical bed itself for positioning, and the possibility of easy removal of the cushion from under the patient safely after intubation. This makes it easier for the patient to return to the supine and neutral position for surgery or any other intervention.
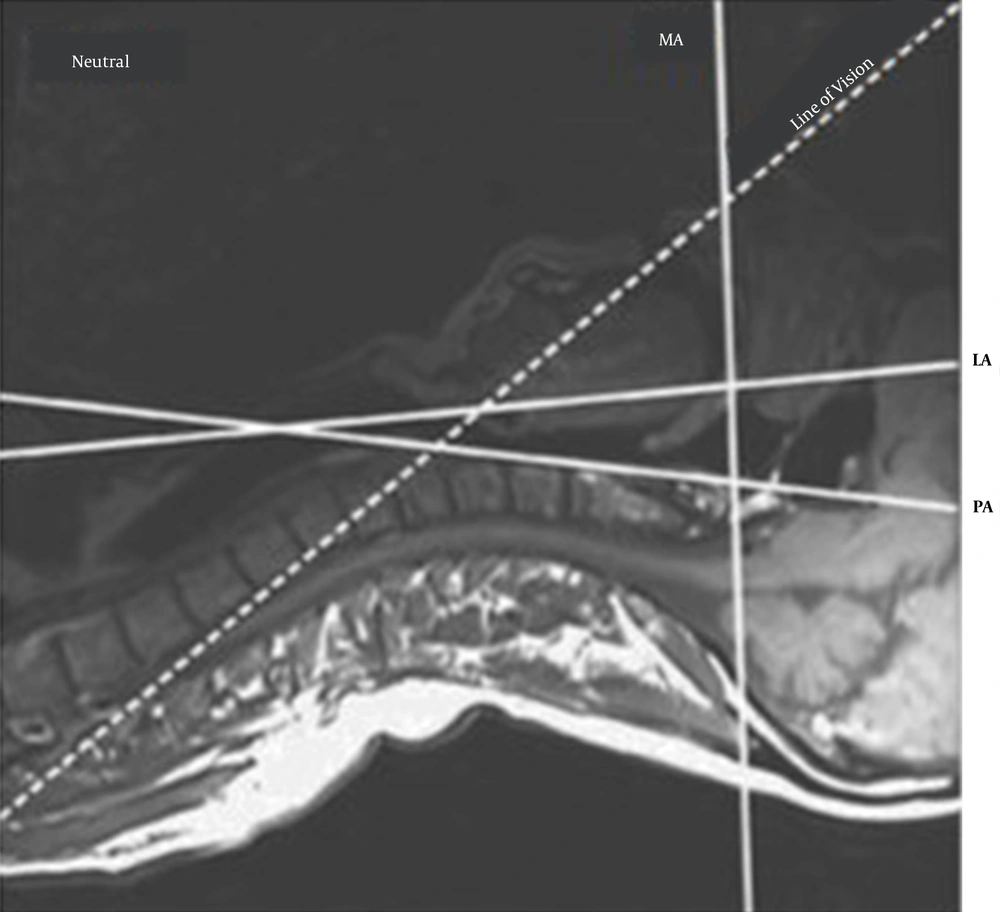
Successful intubation requires the alignment of the three airway axes, namely the mouth, the throat, and the larynx (33). An important step in this direction and successful intubation of the trachea is the proper position and placement of the head and neck in relation to the trunk and chest. The theory of three-axis alignment was proposed by Bannister (34), which is one of the most widely used and accepted theories in this field. In studies by Greenland et al. (35, 36), which focused on airway examination under MRI, the mouth axis was defined as a line parallel to the hard palate, the pharynx axis was defined as a line parallel to the anterior edge of the second vertebral axis, and the larynx axis was defined a line of cricoid cartilage and glottis (Figure 3). Neck extension is difficult in obese people, but it is very critical for intubation. However, in our presented modified position, this maneuver could be easily accessible. We created a passive neck extension by placing the patient in a position of head elevation with the aid of a bed positioning, which by itself is a factor in improving ventilation and laryngoscopy as stated by Rao et al. (31) and Dixon et al. (21), along with creating a flexion in the atlantoaxial joint by an 8-cm pillow under the patient's head, as in the sniff position. Then, we placed a cushion (which is easily prepared with a 1-lit normal saline intravenous container) between the patient's scapula before induction of anesthesia. Unlike other studies, which focused only on moving the head and neck on the proximal portion of the axis described, in our experiment, the cushion located between the patient's shoulders changed the distal axis of the larynx and pharynx and moved the axis upwards in the vertical plane, which provided greater alignment, and consequently, a suitable view for intubation.
Due to the lack of significant differences in intubation time between the two groups, short preparation time, and available equipment, the use of the modified ramp position is a good alternative to the ramp position. Our results also showed that the difference in mean oxygen saturation during intubation between the two groups of ramps and modified ramps was not statistically significant. This indicates proper ventilation and preoxygenation in the modified ramp position.
However, our study had some potential limitations. First, we could not blind the anesthesiologist for intubation. Second, the study was performed on patients with stable and elective hemodynamic state. Finally, the lack of access to TOF monitoring was another limitation.
5.1. Conclusions
It seems that there is no significant difference between the ramp and modified ramp strategies in any of the intubation and ventilation parameters, and thus, the modified condition can be a suitable, fast, and available alternative for the intubation of obese patients. It is recommended that the study be performed in critically-ill patients outside the operating room.