1. Background
Acute respiratory distress syndrome (ARDS), which is characterized by rapidly progressing shortening of breathing, severe hypoxemia, and bilateral pulmonary infiltration, along with the absence of left atrial hypertension, is associated with underlying conditions such as sepsis, pneumonia, the trauma of the airway, and aspiration of gastric content (1). It is classified as mild (PaO2/FiO2: 200 - 300), moderate (PaO2/FiO2: 100 - 200), and severe (PaO2/FiO2 < 100) (1). Mechanical ventilation for more than two days is the other cause of ARDS in patients who are admitted to the intensive care unit (ICU) (2). Studies have shown that patients who wean off later from mechanical ventilation have a higher rate of ventilator-associated pneumonia (VAP), lung damage, and mortality, which impose more costs on the health system (3-11). The presence of fibrin mesh in the air sac and fibrin accumulation in pulmonary capillaries and venules demonstrate an inflammatory process, which leads to ARDS development (12-14). Fibrin deposition will result in pulmonary shunt (ventilation-perfusion mismatch) and pulmonary fibrosis (15-17).
Heparin is widely used as an anti-thrombotic medication, while it has anti-inflammatory effects. It has been shown that the administration of heparin helps the nitric oxide release from the endothelium, mucus tenacity reduction, and systemic inflammatory pathways inhibition (18-20). It is shown that nebulized heparin targets the deposition of fibrin in the lungs (21). In patients with acute lung injury and related conditions, nebulized heparin reduces the dead space of the lungs, (17, 22-25). A recent randomized clinical trial showed that nebulized heparin was effective in reducing the development of new ARDS in patients who were admitted to the ICU and were on invasive ventilation (21).
2. Objectives
As there is little evidence regarding this issue, we designed this randomized clinical trial to investigate the effects of nebulized heparin and inhaled sterile water on weaning off the intubated ARDS patients admitted to the ICU in Iran.
3. Methods
This double-blind randomized clinical trial was conducted in Golestan and Imam Khomeini hospitals of Ahvaz University of Medical Sciences between April and July 2020. The study had been approved by a local ethics committee, and the protocol was registered in IRCT (IRCT code: IRCT20190506043492N4). The relatives of the eligible patients were asked to fill the informed consent forms, as the patients could not.
3.1. Inclusion Criteria
We enrolled patients aged 18 to 60 years on mechanical ventilation for more than 48 hours, with the respiratory index (PaO2/ FiO2) of < 200, PEEP > 5 cmHg in the ventilator setting, and bilateral pulmonary infiltration in CXR.
3.2. Exclusion Criteria
They included an unwillingness to participate, heparin sensitivity [history of heparin-induced thrombocytopenia (HIT)], receiving a therapeutic dose of heparin, enoxaparin, or warfarin, uncontrolled bleeding, history of intracranial hemorrhage in the past 12 months, abnormal PTT, NR, or coagulopathy disorder, and underlying heart or lung disorders.
3.3. Randomization
Using a computer for simple random number generation, an expert nurse randomly assigned patients into two groups. Group one received the intervention (nebulized heparin 5000 u/BD for a week), and group two (control group) received nebulized sterile water (2 cc/BD for a week).
3.4. Blinding
Both patients and the physician were blinded to the study. They did not know group assignments. The person who injected medication (heparin/water) into the nebulizer did not know if the syringe contained heparin or sterile water. The syringe was prepared with another anesthesiologist and labeled 1 or 2. The person taking blood samples for coagulation enzymes lab tests did not know the type of intervention. Also, the statistical analyzer was unaware of the type of the group.
3.5. Intervention
Patients in the intervention group, in addition to routine care, received 5,000 units of nebulized heparin (DarooPakhsh Iran Company) every 12 hours via the nebulizer, which was connected to the tracheal tube from one side and to the ventilator from the other side. The control group received 2 cc of sterile water in the form of inhalation via the nebulizer every 12 hours. The common treatment for ARDS included antibiotic therapy, nutritional support, electrolyte balance, and positive end expiratory pressure (PEEP) levels in the ventilator setting based on the patient's condition. All treatments were supervised by an intensivist according to the ARDS protocol.
The respiratory index (PaO2/FiO2), pulmonary shunt percentage [measured by arterial blood gases (ABG)], tidal volume, minute ventilation, admission duration in the ICU, and days of mechanical ventilation required were recorded for each patient for one week. In this study, PaO2 and pulmonary shunt were measured by ABG.
FIo2: measured by ventilator-TV (tidal volume): 4 - 5cc per kg, also measred by ventilator
MV (minute ventilation:): TV * RR (respirstory rate) RR: measured by ventilator
3.6. Statistical Analysis
We used SPSS version 22 software (SPSS Inc., Chicago, IL, USA) to analyze the collected data. Qualitative data and frequencies were compared using the chi-square test. As the distribution of data was normal, the independent samples t-test and repeated-measures ANOVA were used for comparing continuous variables. A P value of less than 0.05 was considered significant.
4. Results
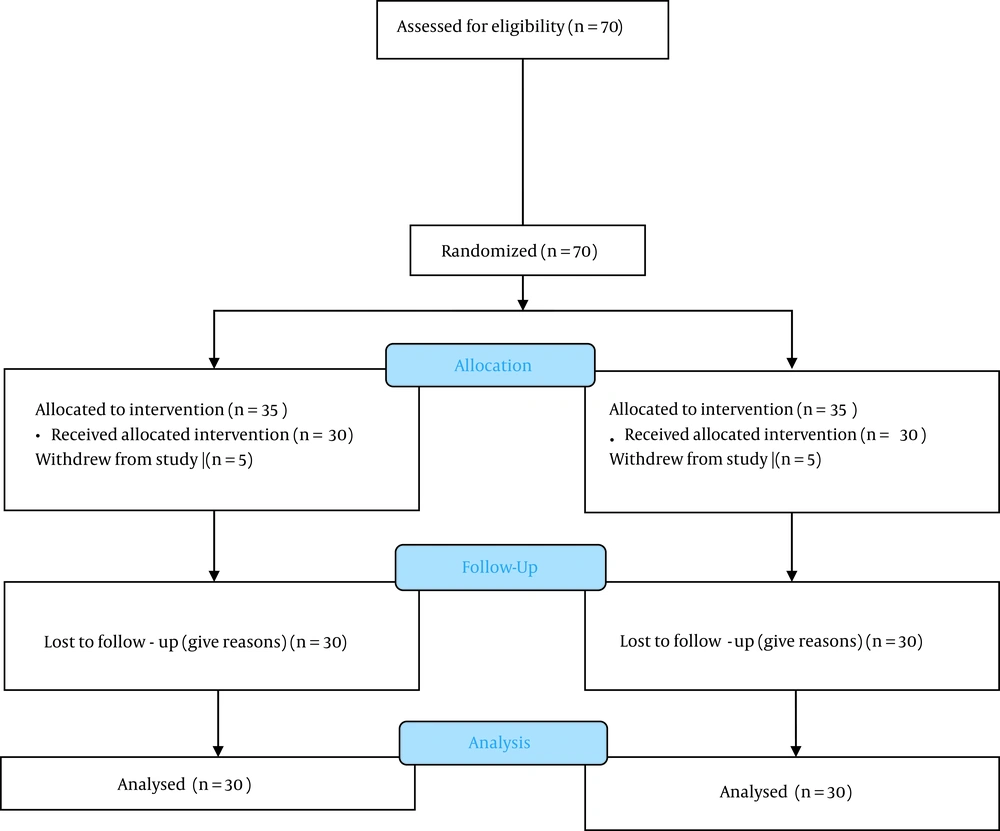
Seventy patients were randomized. Five patients from each group withdrew before the study began. Finally, 30 patients in each group were analyzed (Figure 1).
There was no significant difference regarding age and sex between the two groups, while the duration of ICU admission and the days of mechanical ventilation required were significantly higher in the control group (Table 1).
| Variables | Intervention Group | Control Group | P Value |
|---|---|---|---|
| Age (y) | 49.87 ± 18.288 | 56.40 ± 14.940 | 0.1 |
| Sex; No. (%) | |||
| Male | 26 (86.6) | 18 (60) | |
| Female | 4 (13.33) | 12 (40) | |
| Duration of ICU admission | 12.67 ± 3.198 | 16.17 ± 2.984 | < 0.001 |
| Days of mechanical ventilation required | 7.00 ± 2.259 | 10.80 ± 2.631 | < 0.001 |
There was no significant difference regarding the mean respiratory index (PaO2/FiO2) on the first four days, while it increased significantly in the intervention group on the fifth day (Table 2).
| Days | Intervention | Control | P-Value |
|---|---|---|---|
| Day 1 | 148.47± 41.591 | 153.70 ± 42.063 | 0.630 |
| Day 2 | 153.00 ± 36.456 | 153.83 ± 40.304 | 0.933 |
| Day 3 | 159.17 ± 38.328 | 152.20 ± 38.664 | 0.486 |
| Day 4 | 169.87 ± 46.853 | 150.03 ± 37.067 | 0.066 |
| Day 5 | 190.67 ± 67.865 | 151.50 ± 37.256 | 0.007 |
| Day 6 | 187.17 ± 49.574 | 145.57 ± 38.162 | 0.001 |
| Day 7 | 193.63 ± 51.582 | 144.83 ± 40.093 | < 0.001 |
The mean tidal volume was not significantly different on the first day, while there was a significant difference between the two groups after the first day (Table 3).
| Day | Intervention | Control | P-Value |
|---|---|---|---|
| Day 1 | 416.67 ± 19.711 | 440.67 ± 48.773 | 0.726 |
| Day 2 | 404.07 ± 71.165 | 439.00 ± 45.664 | < 0.001 |
| Day 3 | 416.67 ± 19.711 | 439.00 ± 45.664 | < 0.001 |
| Day 4 | 416.67 ± 19.711 | 439.00 ± 45.664 | < 0.001 |
| Day 5 | 416.67 ± 19.711 | 439.00 ± 45.664 | < 0.001 |
| Day 6 | 416.67 ± 19.711 | 439.00 ± 45.664 | < 0.001 |
| Day 7 | 416.67 ± 19.711 | 439.00 ± 45.664 | < 0.001 |
The mean pulmonary shunt was not significantly different on the first day, while there was a significant difference between the two groups after the first day (Table 4).
| Days | Intervention | Control | P-Value |
|---|---|---|---|
| Day 1 | 2.59 ± 0.314 | 3.26 ± 0.623 | 0.063 |
| Day 2 | 2.49 ± 0.321 | 3.22 ± 0.656 | 0.001 |
| Day 3 | 2.42 ± 0.298 | 3.22 ± 0.638 | 0.001 |
| Day 4 | 2.33 ± 0.265 | 3.21 ± 0.666 | < 0.001 |
| Day 5 | 2.26 ± 0.239 | 3.23 ± 0.650 | < 0.001 |
| Day 6 | 2.15 ± 0.175 | 3.32 ± 0.701 | < 0.001 |
| Day 7 | 2.12 ± 0.154 | 3.31 ± 0.799 | < 0.001 |
The mean minute ventilation was not significantly different on the first and second days, while there was a significant difference between the two groups after the first day (Table 5).
| Day | Intervention | Control | P-Value |
|---|---|---|---|
| Day 1 | 8370.67 ± 1708.460 | 8500.00 ± 1402.087 | 0.750 |
| Day 2 | 8332.67 ± 89.871 | 8322.00 ± 1279.087 | 0.970 |
| Day 3 | 7744.67 ± 942.201 | 8538.00 ± 1500.339 | 0.017 |
| Day 4 | 7309.33 ± 831.081 | 8385.33 ± 1397.189 | 0.001 |
| Day 5 | 6867.33 ± 828.650 | 8461.00 ± 1685.092 | < 0.001 |
| Day 6 | 6452.33 ± 821.276 | 8560.00 ± 1871.942 | < 0.001 |
| Day 7 | 6184.00 ± 822.014 | 8421.33 ± 1990.446 | < 0.001 |
5. Discussion
The results of this randomized clinical trial showed that nebulized heparin is effective in reducing ICU admission duration and mechanical ventilation duration.
In a recent RCT conducted by Dixon et al., patients were randomly assigned into the nebulized heparin or placebo groups. Their results demonstrated that the intervention group had significantly lower odds of re-admission to the ICU (21). In 2010, Dixon et al. randomly assigned 50 patients into the nebulized heparin or control groups and found that the heparin group had significantly fewer days of mechanical ventilation (23). They found no significant difference regarding the average daily PaO2/FiO2 ratio while we found a significant difference after four days of intervention. Ghiasi et al. randomly assigned 60 patients into the nebulized heparin and control groups and found that the average daily PaO2/FiO2 ratios were not significantly different between the two groups, and heparin administration was associated with more ventilator-free days (although the difference was not significant) (26). Their results also demonstrated that the ICU admission and hospital stay durations were not significantly different between the two groups.
Mohammad et al. enrolled 25 patients in the nebulized heparin group and 25 patients in the control group in Egypt. They reported that ICU-free days on day 28 and ventilator-free days on day 28 were not significantly different between the two groups (27). Glas et al. conducted a systematic review and meta-analysis of five studies with 286 patients and found that ventilator-free days and alive at day 28 were not significantly different between the nebulized heparin and control groups (28). Dixon et al. in 2008 reported that nebulized heparin helped coagulation activation to reduce in patients with acute lung injury (25), which was confirmed by their further publication in 2010 (17). These findings could be due to the anti-inflammatory effects of heparin, which leads to the reduction of hyaline membrane formation and microvascular thrombosis (17).
Our results showed that mean tidal volume, minute ventilation, and pulmonary shunt were significantly higher in the control group, which is indicative of better pulmonary and respiratory status and the possibility of earlier weaning off in the intervention group. One explanation for early extubation in the heparin group may be the decrease of fibrin deposition in the hyaline membrane (pulmonary microcirculation and alveolar sacs) (23). Alveolar perfusion and ventilation reduction are the results of gas exchange barriers, which occur after fibrin deposition (13, 23, 29, 30). On the other hand, leukocyte recruitment, according to the pro-inflammatory role of fibrin, would cause lung damage (31).
Nebulized heparin clearance occurs slowly, and after 24 hours, 40% of its initial amount is present in the lungs, which can have anti-coagulant effects (32, 33). Some previous studies also showed that heparin may inhibit the growth of bacteria and viruses in the lungs by restricting their adhesion to respiratory surfaces (34, 35) while another study did not support this finding (23).
This study had some limitations. First, the number of patients was limited. Second, it was a single-center study. The third limitation was the varying doses of heparin used in different studies. Larger multicenter studies are recommended.
5.1. Conclusion
The results of the present study showed that the inhalation of heparin in intubated ARDS patients admitted to the ICU could improve the respiratory and pulmonary status of patients and reduce the need for mechanical ventilation and the days of ICU stay. In general, nebulized heparin can be used as an effective and safe drug for ARDS patients on mechanical ventilation.