1. Background
Cerebrovascular accident (CVA) is the most common disabling neurological disorder (1) and the fourth leading cause of death in the United States after heart disease, cancer, and chronic lung disease (2). CVA is a vascular lesion that causes a neurological deficit and begins acutely and lasts over 24 hours (3). To diagnose CVA and find its causes and rule out other disorders similar to stroke, a number of evaluations such as electrocardiogram (ECG), computed tomography (CT) scan, magnetic resonance imaging (MRI), echocardiography, angiography, and Doppler sonography can be performed (4, 5). In addition to causing death, strokes cause disability of the patient throughout life, which can be in the form of various movement, sensory, verbal, memory, visual, etc. disorders that depend on the anatomical location of the affected arteries. These side effects can severely affect a person’s future (6, 7). Many patients can experience unexpected clinical deterioration during hospitalization, which is associated with in-hospital mortality (8-10).
The primary goal in predicting hospital mortality is to improve patient prognosis. Several scoring systems are currently used to predict mortality in hospitals (11-13). Acute physiology and chronic health evaluation (APACHE) and Simplified Acute Physiology Score (SAPS) are examples of disease prognosis models. However, these scales are relatively complex and include several items that cannot be used as rapid and accessible clinical tools (14).
Another system used at the Royal College of London is called Modified Early Warning Score (NEWS), which is a good development (15, 16). NEWS is a tool used to identify at-risk patients. Scores are based on initial clinical observations, including heart rate, respiration rate, systolic blood pressure, oxygen saturation, level of consciousness, body temperature, and ventilator respiratory support. High scores indicate that the patient is progressing to a critical condition. This system is currently used in several countries (17-19).
2. Objectives
To date, several studies have evaluated NEWS, but no study has been conducted in this regard in Iran. So, the effectiveness of this new, fast, and accessible prognostic model should be evaluated. In this method, the information about the parameters is recorded upon admission to the ICU, which increases the accuracy of data collection. Accordingly, this study examines the ability of NEWS in predicting mortality in critical stroke patients admitted to the ICU.
3. Methods
The present cross-sectional study was conducted in Alavi Hospital of Ardabil, Iran, for six months in 2016 - 2017. We included 90 patients who had a definite diagnosis of CVA based on clinical criteria (such as loss of consciousness, paresis, palsy, speech disorders, etc.) and para-clinical criteria (such as CT scan and MRI), which were evaluated by a neurologist. The number of patients was determined through considering the number of patients in similar articles and cases admitted to the ICU in six months and approved by statistical consultants.
For all patients in any age group and with any underlying disease with a definitive diagnosis of CVA, all the required NEWS parameters were measured and evaluated at the beginning of ICU admission and up to the first 24 hours. It should also be noted that underlying diseases do not interfere with NEWS scoring and were not among our exclusion criteria. Respiratory rate, heart rate, and oxygen saturation detected by Saadat B5 ICU monitoring device, respiratory support managed by observation, body temperature measured by Beaver digital thermometer model FT09, systolic blood pressure measured with Rosemax GB102 hand barometer, level of consciousness assessed by the AVPU scale (Alert, Voice, Pain, Unresponsive scale), and checklists designed based on NEWS for each patient were completed.
Patients who underwent cardiopulmonary resuscitation (CPR) during hospitalization and before admission to the ICU were excluded from the study due to increased risk of mortality and disruption of outcome. Table 1 depicts the NEWS score calculated for each patient.
| Physiological Parameters | Score | ||||||
|---|---|---|---|---|---|---|---|
| 3 | 2 | 1 | 0 | 1 | 2 | 3 | |
| Respiratory rate | ≤ 8 | 9 - 11 | 12 - 20 | 21 - 24 | ≥ 25 | ||
| Oxygen saturation | ≤ 91 | 92 - 93 | 94 - 95 | 96 - 100 | |||
| Supplemental oxygen | Yes | No | |||||
| Temperature (°C) | ≤ 35 | 35.1 - 36 | 36.1 - 38 | 38.1 - 39 | ≥ 39.1 | ||
| Systolic BP | ≤ 90 | 91 - 100 | 101 | 110 | 111 - 219 | ≥ 220 | |
| Pulse rate | ≤ 40 | 41 - 50 | 51 - 90 | 91 - 110 | 110 - 130 | ≥ 131 | |
| A | V, P, or U | ||||||
Scores Related to the Physiological Parameters of the NEWS a
According to the NEWS scores, patients were classified into three groups of high risk (total scores greater than or equal to 7), moderate risk (total scores of 5 - 6 or 3 scores from only one parameter), and low risk (total scores of zero or 1 - 4) (Table 2).
| Clinical Risk | NEWS scores |
|---|---|
| Low | 0 |
| Aggregate 1 - 4 | |
| Medium | Red score (Individual parameter scoring 3) |
| Aggregate 5 - 6 | |
| High | Aggregate 7 Or more |
The NEWS Thresholds and Triggers
Patients were followed up during their stay in the ICU. Regarding the patients who died in the ICU, the relationship between NEWS scores and mortality was assessed. Also, in the deceased ones, each of the NEWS parameters was statistically examined separately to determine which of them was more disturbed.
This study was approved by the ethics committee of Ardabil University of Medical Sciences (code: IR.ARUMS.REC.1398.652). The collected data were entered into SPSS software V24 and presented in the form of frequency tables and graphs. Chi2, t-test, and logistic regression tests were used to examine the relationship between variables. A P-value less than 0.05 was considered significant.
4. Results
In this study, out of 90 patients (female: 50 vs. male: 40), 23 (25.6%) died. The mean age of patients was 53.90 ± 12.68 years, and the age range was 24 to 92 years. In the assessment of the level of consciousness with AVPU, 71 (78.9%) patients had a score of 3, meaning that in the first 24 hours of entering the ICU, they had a response to sound or pain or did not respond to the painful stimulus. Among the 90 patients studied, 54 (60%) were low-risk, 24 (26.7%) were moderate-risk, and 12 (13.3%) were high-risk.
Among all the subjects, 60 (66.7%) patients had a heart rate of 51 - 90 beats per minute (a zero score), 83 (92.3%) patients had systolic blood pressure of 111 - 219 mmHg (a zero score in terms of systolic blood pressure), 88 (97.8%) patients had a body temperature of 38.0 - 36.1°C (a zero score), 64 (71.2%) patients had oxygen saturation ≥ 96% (a zero score), 79 (87.8%) patients had a respiratory rate of 12 - 20 breaths per minute (a zero score), and 69 (67.7%) patients did not have respiratory support (a zero score). According to the data in Table 3, out of 90 patients studied, 54 were low-risk, 24 were moderate-risk, and 12 were high-risk (Table 3).
| Level of risk Scores | No. (%) |
|---|---|
| Low (0 - 4) | 54 (60) |
| Moderate Red Score (5 - 6) | 24 (26.7) |
| High (≥ 7) | 12 (13.3) |
| Total | 90 (100) |
Distribution of Clinical Risk in CVD Patients
Among the patients who died, 56.5% were female, and 43.5% were male. There was no significant relationship between sex and age with patient mortality. Also, 5.3% of the patients who received a score of zero from the level of consciousness parameter died, while 30.98% of patients with a score of 3 died. There was a significant relationship between the level of consciousness at the onset and mortality of CVA patients.
There was a significant relationship between heart rate at the onset and mortality rate of CVA patients. In addition, there was a significant relationship between systolic blood pressure at the onset and the mortality rate of CVA patients.
The body temperature of 97% of alive patients was between 38.0 - 36.1 (a zero score), and all the deceased patients had a score of zero in terms of body temperature. There was no significant relationship between body temperature at the onset and mortality of CVA patients in this study. Among the patients who survived, most of them (71.6%) had a score of zero, and among the patients who died, most of them (69.6%) had a score of zero and oxygen saturation ≥ 96. There was no significant relationship between oxygen saturation and mortality rate in CVA patients. Among the patients who survived, nearly all (92.5%) cases had a score of zero, and among the patients who died, most (73.9%) cases had a score of zero (12 - 20 breaths per minute).
There was no significant relationship between the number of breaths per minute at onset and the mortality rate in CVA patients. Also, 79.8% of patients who did not have respiratory support at onset survived, but 42.8% of patients who had respiratory support at onset died. There was a significant relationship between respiratory support and mortality of CVA patients. Based on the data in Table 4, individuals with medium clinical risk, without considering the mortality or discharge status, had a relatively longer stay in the ICU compared to those who had low and high clinical levels. Assessing the relationship between NEWS and length of stay with T-Test showed no significant relationship between them.
| Level of clinical risk | Length of Stay; Mean ± SD | P-Value |
|---|---|---|
| Low | 12.7 ± 2.5 | 0.5 |
| Moderate | 17.3 ± 3 | |
| High | 12.3 ± 8.3 |
The Relationship Between NEWS and ICU length of Stay Among the Studied CVA Patients
The mean length of stay of patients who survived was 15.4 ± 1.2 days, which was significantly higher than that of deceased patients (9.2 ± 5 days). Based on Table 5, according to the NEWS, at the time of admission, 16.7% of low-risk, 25% of moderate-risk, and 66.6% of high-risk patients died.
| Level of risk Scores | Survived | Died | Total | P-value |
|---|---|---|---|---|
| Low (0 - 4) | 45 (83.3) | 9 (16.7) | 54 (100) | 0.002 |
| Moderate (5 - 6) or (Red Score) | 18 (75) | 9 (25) | 24 (100) | |
| (Red Score) High (≥ 7) | 4 (33.3) | 8 (66.6) | 12 (100) |
Relationship Between Clinical Risk Level at Admission and Mortality of Patients
The results showed that there was a significant relationship between clinical risk at the onset and the mortality rate of CVA (P = 0.002). According to the data obtained from the logistic regression test (Table 6), among the above variables, only AVPU and length of stay had a significant relationship with the mortality rate.
| Variables | ODDs | 95% CI | P-Value | |
|---|---|---|---|---|
| Upper | Lower | |||
| Sex | 1.51 | 5.19 | 0.44 | 0.51 |
| Age | 1.04 | 4.09 | 0.99 | 0.09 |
| AVPU | 0.44 | 0.97 | 0.2 | 0.039 |
| HR | 0.43 | 1.09 | 0.17 | 0.074 |
| SBP | 0.27 | 1.2 | 0.06 | 0.084 |
| SO2 | 1.23 | 2.6 | 0.58 | 0.59 |
| RR | 0.78 | 1.71 | 0.36 | 0.54 |
| Respiratory support | 0.6 | 1.2 | 0.3 | 0.15 |
| LOS | 1.074 | 1.14 | 1.009 | 0.024 |
The Results of the Logistic Regression Test to Detect the Effective Factors on Mortality Prediction in Hospitalized Patients in ICU
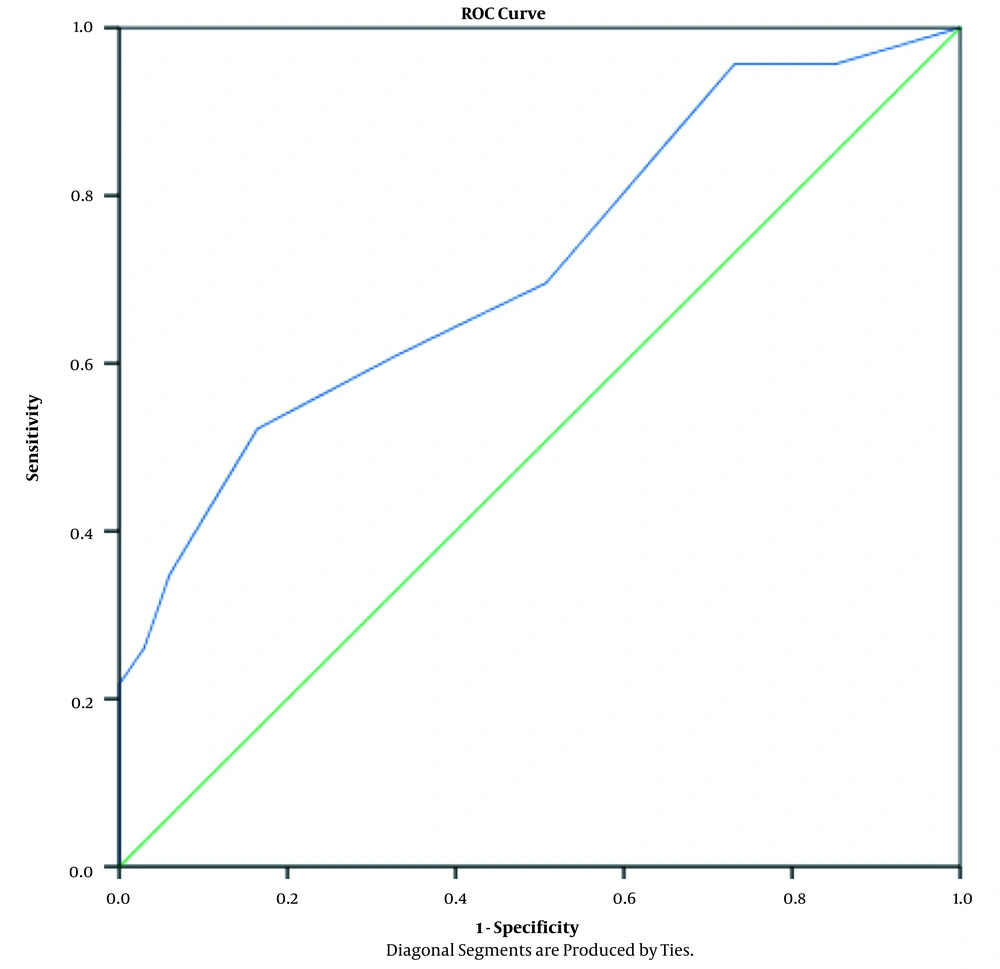
Based on the receiver operating characteristic (ROC) curve, the area under the ROC curve (AUC) was 72%. Regarding the cut-off point 3, the sensitivity and specificity of this indicator for detecting and predicting mortality was about 96% and 76%, respectively (Figure 1).
5. Discussion
The ICU has been provided for management of critically ill patients (19, 20). Since there are always limitations in the services that can be provided in the ICU (21), achieving appropriate criteria to predict the mortality of patients admitted to these units is very important for prioritizing patients to provide services (22-24). So far, several scoring systems such as SAPSП and APACHEП have been used to quantify patient status and predict mortality. However, these scales are relatively complex and include several items that cannot be used as rapid and accessible clinical tools (4).
NEWS is a scoring system used to identify at-risk patients; scores are based on initial clinical observations, including heart rate, respiratory rate, systolic blood pressure, oxygen saturation, level of consciousness, body temperature, and oxygen respiratory support (6). So far, studies have assessed the ability of the NEWS scoring system in patients admitted to different wards. In the present study, we evaluated the effect of NEWS upon admission to the ICU in predicting the mortality of 90 CVA patients in Ardabil, Iran. We also investigated the relationship between each of the NEWS parameters with mortality. Our results showed a significant relationship between the parameters of level of consciousness, heart rate per minute, systolic blood pressure, and respiratory support independently with patient mortality, so that the higher the score of these parameters, the mortality will likely be higher during hospitalization. However, the parameters of sex, age, body temperature, oxygen saturation, and respiratory rate could not predict the mortality of CVA patients. The patients’ length of stay was not predictable based on NEWS at the onset. Our study also showed that when the relationship between each of the NEWS parameters (independently and not as a total score) is measured in conjunction with the variables of age, sex, and length of stay by logistic regression test, this relationship is only significant at the level of consciousness and length of stay. In other studies, the parameters of NEWS have not been studied separately so far. Our study also showed that in CVA patients admitted to the ICU, the higher the calculated score at the time of admission, the higher the risk of mortality during ICU hospitalization. However, in this study, the patients’ mortality after discharge was not followed up due to time limitation.
The aim of our study was to prioritize critically ill CVA patients to provide them intensive and specialist care due to limited hospital facilities and not to predict overall mortality, as it seems that due to differences in post-discharge care, different factors after discharge can influence the patients’ conditions. In a study conducted by Liljehult and Christensen (6) in 2015, the mortality of stroke patients with NEWS Vital signs was measured immediately after admission and continuously during the hospitalization period. A total of 24 (8.8%) patients died within 30 days. The mortality rate was lowest for the 0 - 1 score at admission (2%) and highest for the score ≥ 5 (63%). Similarly, in our study, the statistical population was only stroke patients, NEWS was able to predict the mortality of stroke patients, and patients with a NEWS score less than 3 at the admission were estimated to have a 96% chance of survival.
A study by Lee et al. (4) showed that the NEWS was effective in predicting in-hospital mortality. According to Kaplan-Meyer survival curves, the survival time of patients who are at high risk according to NEWS is significantly shorter than the patients at low risk. In addition, Lee et al. showed that the combined model, which includes other factors such as age and diagnosis, is more effective in predicting in-hospital mortality than NEWS alone (4). In our study, the need for the NEWS scoring system was able to predict the mortality of CVA patients admitted to the ICU; but in an independent study, there was no significant relationship between age and mortality.
A study by Uppanisakorn et al. (13) showed that NEWS could be an independent predictor of early clinical deterioration in ICU discharge. In fact, NEWS showed 93.6% sensitivity and 82.2% specificity in predicting clinical deterioration in the first 24 hours after ICU discharge (13). In our study, like the study by Uppanisakorn et al., NEWS was effective in predicting the mortality of ICU patients, and the sensitivity and specificity of this index for predicting mortality was about 96% and 76%, respectively (13).
Smith et al. reported that NEWS has a great ability to diagnose patients at risk of premature cardiac arrest, unexpected hospitalization in the ICU, or death within 24 hours (14). In our study, we showed that this scoring system can predict the patients’ clinical conditions even in more than 24 hours and after the ICU discharge. However, continuous monitoring of patients during ICU admission with NEWS may help to predict patients’ conditions accurately until discharge. However, a meta-analysis and systematic review by Hamilton et al. showed that NEWS could not predict mortality of patients with sepsis (15). Comparing this study with our study showed that the predictive power of the NEWS scoring system in patients with stroke is greater and better than the predictive power of this system in patients with sepsis. However, various factors such as accuracy in data collection and even the feature of disease due to its unpredictable and critical nature and the possibility of multisystem involvement can affect the outcomes.
5.1. Conclusion
In this study, we evaluated the effect of NEWS on predicting mortality of stroke patients in the ICU. We witnessed a significant relationship between clinical risk based on NEWS scoring system and patients’ status, which indicates a significant increase in mortality in patients with higher NEWS scores. Further studies with larger sample sizes and on other diseases are needed to evaluate the ability of this system in predicting mortality and survival of discharged patients. It is also suggested that this scoring system be studied in comparison with other scoring systems.