1. Background
The coronavirus disease 2019 (COVID-19) has generated more changes in our personal and professional lives than the previous coronavirus epidemics of SARS and MERS. Healthcare providers are at the epicenter of this crisis with overworking of specialists (1, 2) while disrupting professionals in training. COVID-19 has forced all governments of the world to modify the patterns of healthcare activity in health centers, as has been the case in Spain (3). Healthcare personnel has performed functions outside their specialty frame, when necessary, showing a great capacity for adaptation. The residents, a group of physicians in training as specialists, faced the pandemic state from a position of particular "vulnerability", with experiences of stress and uncertainty about their role within the system (4-8). One of the specialties most involved in managing patients with COVID-19 was Anesthesiology and Critical Care (9-11). During the pandemic, some countries decided to use the services of anesthesiology residents, with superior autonomy and decision-making capacity. This was evaluated by the residents themselves within their medical education process, as constructive, both concerning their training and provision of clinical services (12).
2. Objectives
The main aim of this study was to determine the impact of COVID-19 pandemic on the training of residents and to determine the consequences that the change in the practice of care has had both at the teaching and personal level in this group. Training alternatives are proposed that would be useful in new situations similar to the one that occurred to ensure the proper training of the residents. The study's secondary objective was to analyze the influence of different variables such as demographics, type of hospital, or year of residency on the stress perceived by this group.
3. Methods
A 28-question digital questionnaire was developed about residents' experiences during the pandemic's first wave from March to May 2020 (Appendix A in Supplementary File). After receiving approval from the Research Ethics Committee of the Hospital General Universitario de Valencia (HGUV), the survey was distributed nationally through digital dissemination media, including email, instant messaging services, as well as social and professional networks. The survey link remained available from July to October 2020.
The target population was all Anesthesia and Critical Care residents who were active in clinical practice, during COVID-19 crisis period. Informed consent was obtained for all surveys, and those incomplete ones, or not completed properly were excluded. The residents from specialties other than Anesthesia and Critical Care, those on sick leave, and those on external rotation during this period were not included.
The " Objective Formative Impact Score " (OFIS) was the primary variable. This is an ordinal quantitative variable, resulting from the addition and subtraction of favorable and unfavorable responses, being proportional to the level of destructing in the routine. This score considers the suspension of internal and external rotations, the modification of the work area, the reorganization of care activity, the alteration of on-call dynamics, or the loss of training opportunities. Based on the survey responses, the calculation of the OFIS was set to 0 as the initial value, adding one point if the respondent was found to be in each of the following cases:
- If you failed the planned rotational (question 7)
- If you stayed at home for several days due to lack of attendance activity, without considering periods at home for window periods or on-call rest (question 8.1).
- If you did not maintain the assistance activity in the same area you were in. (question 8.2)
- Whether transfer to a COVID or non-COVID resuscitation area (questions 8.3 and 8.4)
- If you maintained scheduled surgical activity (question 8.5)
- If you participated in the activity in another unit outside of the anesthesiology department (question 8.6)
- If you had to extend your regular working hours (question 11)
- If you had to stop attending congresses and/or training courses (question 25)
- If you did not sign up for congresses or other virtual training events (question 26.1)
- If you did not dedicate time to self-study (question 26.2)
- If you were not part of a research team (question 26.3)
- If your planned external rotations in this period were postponed with or without an agreed date or were definitively canceled (question 27).
Finally, according to the result of the sum of these scores, the excess, or shortage of monthly on-call duty performed during this period proportional to the last months before the pandemic was added. The significance given to the ordinal numerical scale obtained from the questionnaire implied that the higher the numerical value obtained, the greater the negative impact that the pandemic had had on the training of anesthesiology residents.
After data collection, statistical analysis was performed using SPSS software version 20 (13). A statistical significance level was established at P < 0.05, and parametric analysis of variance (ANOVA) and Pearson correlation tests were performed to associate the quantitative variables OFIS and the subjective assessment score with the categorical variables and Student t-test to associate the categorical variables with each other. Tukey's test was used for post hoc analysis in cases of significance with the ANOVA test. All values and scores were expressed as means and standard deviations or percentages.
4. Results
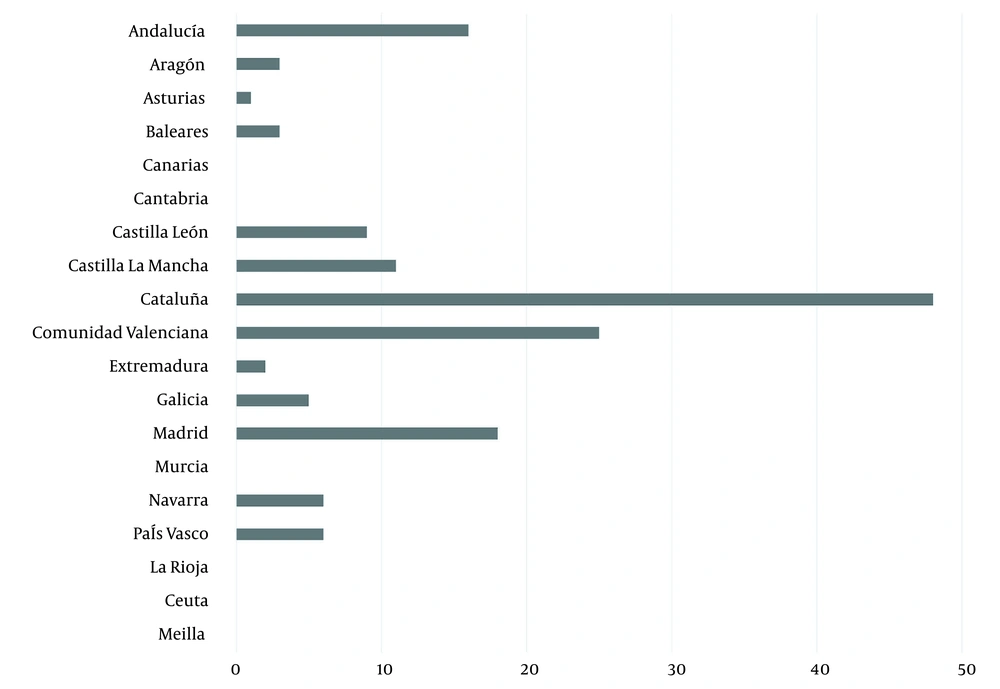
The total number of valid surveys was 150, distributed in the regions as shown in Figure 1. The mean age was 27.44 years ± standard deviation (SD) 1.80, with 69.33% (n = 104) of the respondents being female and 29.33% (n = 44) male. Of the responses obtained, 28.00% (n = 42) corresponded to first-year residents (R1), 32.00% (n = 48) to R2, 29.00% (n = 44) to R3, and 11.00% (n = 16) to R4. A total of 90.66% (n = 136) of the respondents had to suspend their planned rotation during the first wave of the pandemic. Of the total number of residents, 70% (n =105) went on to practice in a COVID-19 resuscitation unit.
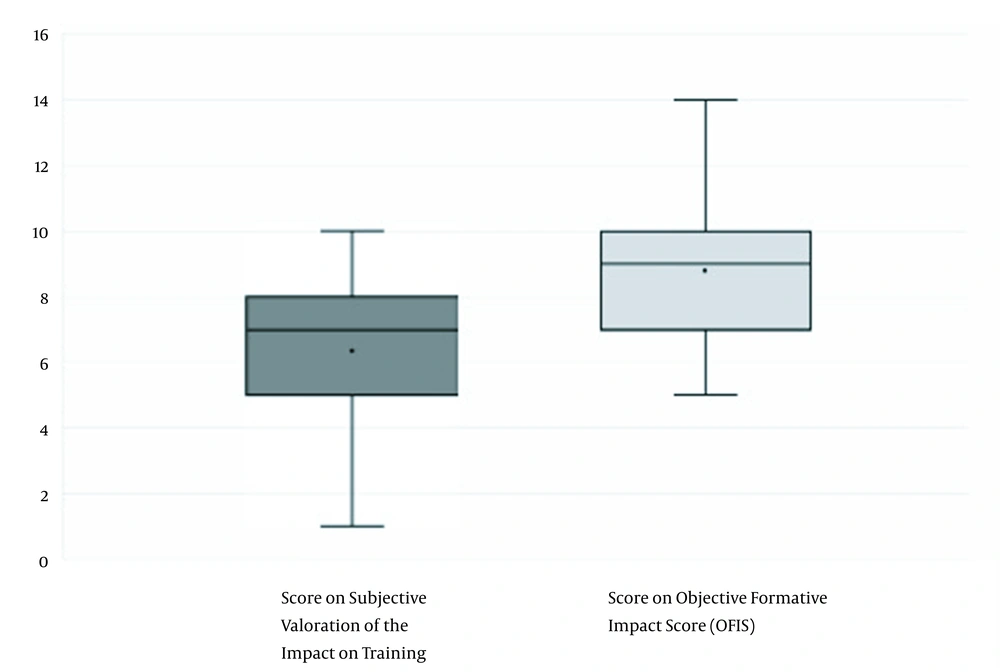
Regarding the degree of exposure to COVID-19 patients, 10.66% (n = 16) of the respondents had no exposure at all. A total of 19.33% (n = 29) declared a sparse and limited direction, including techniques with a lower risk of contagion, such as airway cannulation. In comparison, 70% (n = 105) had a complete exposure, with advanced airway management with techniques such as orotracheal intubation. A statistically significant relationship was found between higher degrees of exposure and higher OFIS values (P = 0.002) (Figure 2). Residents rated their learning in anesthesiology and critical care from 1 to 10 during the first wave of the pandemic. A mean result of 6.34 (SD 1.88) was obtained (Subjective assessment graph in Figure 2). On the other hand, a value was obtained by calculating OFIS = 9.11. This value is intended to objectively represent the global impact on the training of the anesthesiology resident (represented in the objective assessment graph in Figure 2).
The mean number of shifts performed by residents in the pre-pandemic period was 4.96 (SD 7.22). This value increased during the emergency situation to a mean of 6.03 (SD 1.73). In addition, 58.66% (n = 88) of the respondents reported an additional increase in the regular working day. During the pandemic, the residents faced stressful situations, with experiences that presented them with ethical conflicts. A total of 41.30% (n = 62) stated that working under suboptimal conditions was the leading cause of high emotional burden that they endured. The application of restrictive criteria for admitting patients to critical care units was the most significant ethical conflict in 16% (n = 24), while it was the Limitation of Therapeutic Effort (LTE) in 15.30% (n = 23). A total of 70% (n = 105) of the respondents assumed an increase in autonomy, which was significantly related to higher OFIS values (P = 0.001).
A total of 70% (n = 105) introduced feelings of fear for their own safety. The lack of Personal Protective Equipment (PPE) in the workplace was the cause of this feeling in 72.60% of the cases. This significantly correlated with higher OFIS values (P = 0.003). A total of 60.66% (n = 90) had to take measures of social distancing from their family or social relationships such as, temporarily moving house so as not to expose their loved ones. Of those surveyed, 54.66% (n = 82) expressed feelings of loneliness during the first wave of the pandemic; however, only 16 cases sought psychological help to cope with this situation.
Study at home was the most frequently used resource to minimize the impact of the loss of training (70.60%, n = 105). Residents rated the learning from 1 to 10 in Anesthesiology and Critical Care during the pandemic's first wave. A mean score of 6.34 (SD 1.88) was obtained. Some 70% (n = 105) considered that the level of learning during this period was lower than expected if they had maintained their programmed activity. Residents in the areas with the highest incidence of COVID-19 infection cases performed significantly worse personal ratings than the medium and low incidence groups (P < 0.001). Specifically, significantly higher scores were obtained by residents assigned to COVID-19 critical care units (P < 0.001) or to units outside the anesthesia service (P = 0.020). However, no differences were found in subjective ratings according to the year of residency or type of hospital.
5. Discussion
Healthcare professionals have suffered a high level of work-related stress as a consequence of the COVID-19 pandemic (11-17). In Spain, after the State of Health Emergency was decreed, the training of medical residents took a back seat, and they were faced with an uncertain and changing role in the face of the challenge posed by the new disease (2, 8, 12). Different studies have reported the effect that the pandemic has had on residents, analyzing the impact at the psychological and formative levels (4-8, 18, 19). However, none of them makes a global assessment with an objective approach of the situation of residents during the pandemic. The Ministry of Health is responsible for accrediting the different teaching units and their training programs (20). There is no tool for objectively assessing the training of residents at the national level. The OFIS parameter was explicitly created for the present study to find the most objective indicator possible of the disruption that the crisis has caused to the usual process of care provision and training of residents.
The care activity of the residents increased during regular working hours and the hours of continuous care. In our study, we have seen that, in the regions most affected by the pandemic during the first wave, the lack of PPE by Anesthesia and Critical care residents was the most prevalent, and there was a more excellent perception of exposure to COVID-19. A higher degree of exposure was statistically significantly related to higher OFIS and the need for increased autonomy and responsibility (Figure 2). This fact seems to be related to the change in the area of care activity performance. Most of the respondents moved to work in COVID-19 critical care and intensive care areas, altogether abandoning other areas of anesthesiology practice, especially those that pertain to surgical anesthesia. This change of location and clinical practice had an impact on the OFIS value.
A total of 70% (n = 105) of the surveyed residents were exposed to situations with a high risk of infection such as airway management, which correlates with a more significant personal impact. The initial lack of knowledge about the characteristics of COVID-19 caused great emotional stress in both general population and healthcare professionals (14-16, 21, 22). One of the risk factors identified was the solitary experience of the first pandemic (17). In our results, we showed that a significant proportion of residents (60,60 %; n = 91) took measures to protect their immediate family, such as moving house, with the corresponding feeling of loneliness. At the same time, those who remained in their usual home experienced the fear of acting as a vector of disease transmission. Other studies have related the geographical location of the highest incidence of cases with a more significant psychological impact on healthcare workers (19). This relationship is also reflected in our results, where a statistically significant relationship was found between the geographical regions with the highest incidence and an increase in OFIS values.
One of the most striking aspects is that both the residency year and the type of hospital did not influence the formative and emotional impact of the residents in this pandemic. According to these findings, we deduce that the contingency and rotational alteration teams have been applied to the total number of residents in each service regardless of the year of their training. This responds to the need to mobilize all available human resources regardless of the training stage of each resident. The COVID-19 pandemic has, at the same time, provided an opportunity to look for alternatives to classical standardized training. Telematic learning through online courses and webinars are training resources widely used in the pandemic (22-26). The main advantages of this training modality are organizational flexibility as it avoids significant travel in situations of restricted mobility. The use of simulation as an educational resource has also gained prominence in resident training.
Our study has some limitations. The parameter used (OFIS) has not been validated, which makes it impossible to establish comparisons with other studies or to draw extrapolatable conclusions. We consider this parameter to be interesting from the point of view of research into resident training, both in relation to COVID-19 and to possible future adversities faced by training. This opens up the possibility of carrying out its validation and application in different settings. Of the total number of Anesthesiology and Critical Care residents in Spain, estimated at 1,200 according to the offer of residents places by the Ministry of Health in the years 2016 - 2019, 150 surveys were obtained, a number that represents 12.50% of the residents, a relatively small sample with respect to other surveys carried out in healthcare personnel referring to the COVID-19 pandemic (13). The data were collected in the months following the pandemic (June-August), with the possibility of the participants incurring a memory bias that could distort the data.
5.1. Conclusions
The COVID-19 pandemic has had a high impact on residents at both educational and personal levels. The OFIS parameter designed by our group provides an objective value on resident training and broadens new horizons to future surveys with similar characteristics. This research allows us to anticipate the additive effect that successive waves of the COVID-19 pandemic will have on resident training and to direct efforts to compensate for the suspension of rotations.