1. Background
Acute moderate to severe postoperative pain is common in surgical patients (1). Some physiological side effects of un-controlled postoperative pain can be problematic for the patients, and inefficient pain management in perioperative period may result in some annoying medical, social, economic, psychological, and individual complications (2-4). Appropriate pain management can reduce morbidity and mortality and hasten recovery and discharge rate, especially in the laparoscopic surgeries (5-10).
Central sensitization after surgical incisions can precipitate acute postoperative pain and may evolve in development of chronic pain syndromes (11, 12).
Non-steroid anti-inflammatory drugs (NSAIDs) and opioids administration have been shown to be effective in controlling pain in perioperative period; however, there are some concerns about their side effects (13-17). Therefore, adjuvant drugs such as ketamine and dexmedetomidine can play a special role in this regard (18-21).
Nowadays, neuraxial and regional techniques are very popular among anesthesiologists, and they are more effective analgesic modalities in the major thoracic and abdominal surgeries compared to systemic medications; however, the need for equipment, postoperative care, and necessary experience, as well as the occurrence of some complications may limit their general application in all the medical centers (22-28).
Considering all these pros and cons, we are always looking for safer alternative analgesia techniques in our daily practice of anesthesia. In this regard, the relationship between high arterial blood pressure and reduced sensitivity to pain has been studied and proved in several investigations (29-32). Therefore, the relationship between pain and hypertension is of great pathophysiological and clinical interest in the field of pain management. Although the clear mechanism of this privilege for intraoperative hypertension has been poorly defined, we assume that this preventive analgesic modality may affect postoperative pain intensity through inhibiting central sensitization process that occurs during surgery.
2. Objectives
In this study, we aimed to evaluate acute postoperative pain score after laparoscopic cholecystectomy in patients undergoing general anesthesia who were deliberately managed with either controlled high blood pressure or controlled normal blood pressure in a restricted range of 20% higher or lower than their baseline preoperative values.
3. Methods
In this double-blind, randomized clinical trial, we included 85 patients according to the American Society of Anesthesiologists (ASA I) in the age range of 20 - 60 years, who had been scheduled for elective laparoscopic cholecystectomy in Firuzgar Hospital of Tehran, Iran.
Assuming a confidence interval of 0.05 and a power of 90%, the sample size was determined to be about 36 in each group:
The Ethics Committee of Iran University of Medical Sciences (IUMS) approved the study (IR.IUMS.FMD.REC.1399.116), and it was registered in the Iranian Registry of Clinical Trials database (IRCT20210607051501N1). Also, written consent was taken from all patients before entering the study.
Inclusion criteria were ASA I patients aged 20 - 60 years, having no comorbidities other than gallbladder disease, and not taking analgesic drugs or herbal medicine two weeks before the surgery.
The exclusion criteria were uncontrolled bleeding during surgery, any change in intraoperative mean arterial blood pressure (MAP) beyond 20% of baseline values recorded before anesthesia, any change in the heart rate more than 100/min or less than 45/min requiring rescue therapy by propranolol or atropine, and change of surgical plan from laparoscopic approach to open surgery by the surgeon for any reason.
After recording the baseline preoperative MAP and heart rate, basic ASA monitoring was applied, and hydration with infusion of 5 mL/kg of 0.9% isotonic saline was started. Moreover, premedication by midazolam 0.015 mg/kg and fentanyl 3 mcg/kg and induction with propofol 1.5 - 2 mg/kg followed by cisatracurium 0.2 mg/kg were considered for each patient. Maintenance of anesthesia was done by continuous infusion of propofol and intermittent bolus infusions of cisatracurium 2 mg every 20 to 30 minutes.
Depth of anesthesia was monitored by bispectral index (BIS) monitoring in a range of 40 to 60 by modifying propofol infusion rate and bolus intermittent infusions of fentanyl 50 μg/h from the beginning to the end of surgery.
Since inducing the pneumoperitoneum by CO2 generally stimulates the sympathetic nervous system and by developing systemic vasoconstriction usually elevates blood pressure, we used a table of random numbers to randomly divide patients into two groups: Group A in whom MAP was allowed to increase up to 20% above the rate measured before anesthesia after induction of pneumoperitoneum, and group B in whom MAP was tightly controlled at baseline or up to 20% lower than preoperative baseline values by infusion of trinitroglycerine (Caspian Tamin Co., Iran) titrated in 5 - 10 mcg/min. Non-invasive MAP measured during anesthesia and recorded regularly at 5-minute intervals.
Intraabdominal pressure after induction of pneumoperitoneum was confined in the range of 14 - 16 cmH2O in both groups by limiting gas insufflation rate.
If MAP during surgery changed more than 20% of baseline values or heart rate increased to more than 100/min or decreased to less than 45/min for any patients in group A or B, the patients were excluded from the study, and rescue therapies were considered. For rescue therapy in such conditions, a predetermined protocol was followed: after confirming that BIS value is in the favorable (40 - 60) range, in case of MAP elevation more than 20% of baseline values, a bolus dose of nitroglycerine (TNG) 200 mcg, and if heart rate increased to more than 100/min, propranolol 500 mcg was given intravenously (IV). In case of reduction of MAP to more than 20% of baseline preoperative values in group B, TNG infusion was hold, and if not corrected, ephedrine 5 mg was considered. In any case of bradycardia to less than 45/min, a bolus 0.5 mg IV dose of atropine was given.
For the management of acute postoperative pain in recovery period and during the first postoperative 24 hours, if VAS was more than 3, parenteral meperidine 0.5 mg/kg was given, and if pain did not reduce properly, the IV morphine 0.1 mg/kg was administered.
Postoperative pain scores were recorded after 2, 8, 12, and 24 hours of surgery by a physician blinded to the patients’ groups (A or B), and the total amount of analgesic medications were recorded. All data were analyzed by SPSS software version 26. To compare data between the two groups, independent t-test, repeated measures analysis of variance (ANOVA), chi-square, and Fisher’s exact tests were used. A P-value less than 0.5 was considered as statistically significant.
4. Results
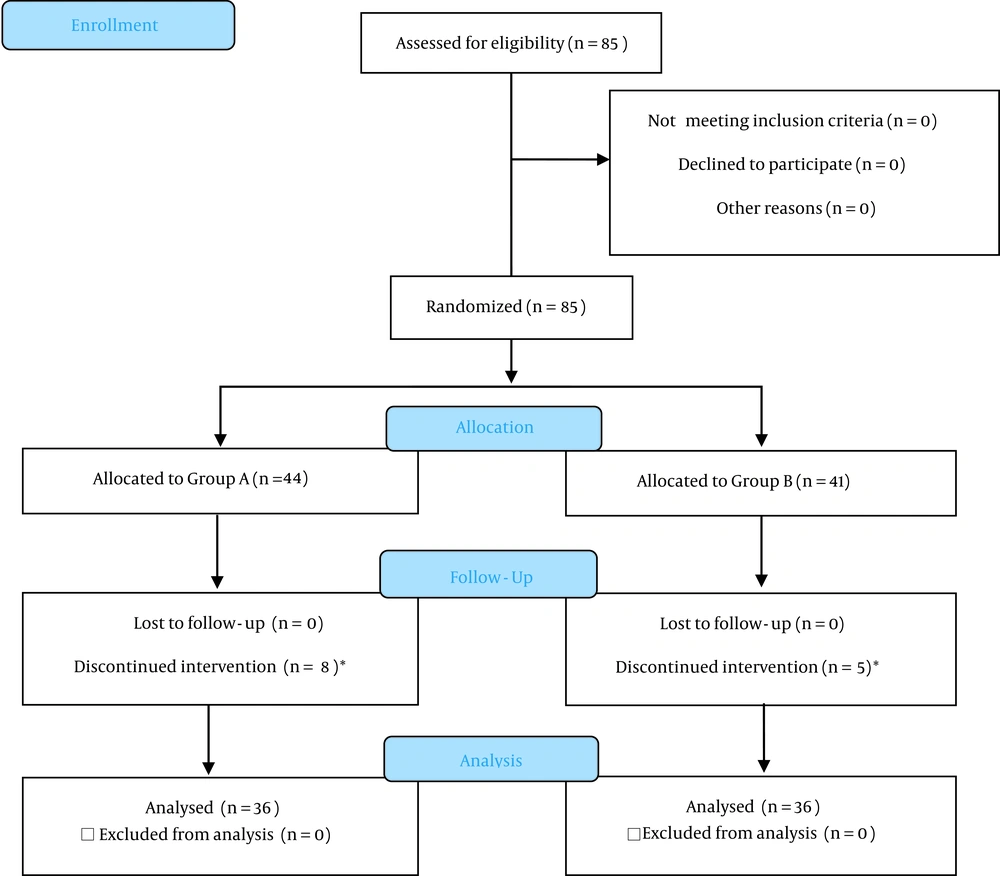
In this study, 85 were randomly assigned into two groups. During follow-up, 13 patients were excluded from the study (Figure 1). Six patients in group A due to the 20% rise of MAP, three patients in group B due to the 20% decrease of MAP, two patients in group A due to uncontrolled bleeding, and two patients in group B due to the change of surgical approach from laparoscopy to open surgery because of technical difficulty and tissue adhesions. Finally, 36 patients remained in each group and were followed up. To compare weight and age between the two groups, student’s t-test was used. For comparison of analgesic dosage and the time elapsed from the end of anesthesia to injecting the first dose of meperidine to manage postoperative pain, Man-Whitney U test was used. We also used Fisher’s exact test for gender comparison and repeated measures ANOVA test for pain score comparison 2, 8, 12, 24 hours after the surgery.
As Table 1 shows, there was no significant difference between the demographic information of the two groups (P > 0.05).
| Variables | A (N = 36) | B (N = 36) | P-Value |
|---|---|---|---|
| Age (y) | 41.9 ± 6.9 | 43.5 ± 7.6 | 0.33 a |
| Weight (kg) | 65.1 ± 8.4 | 67.1 ± 7.3 | 0.28 a |
| Gender, No. (%) | |||
| Male | 4 (11.1) | 5 (13.9) | 0.1 a |
| Female | 32 (88.9) | 31 (86.1) | 0.1 a |
| Surgical time (min) | 46.1 ± 11.3 | 45.6 ± 11.3 | 0.83 a |
| Pain Score (VAS) | |||
| 2 h | 2.69 ± 0.98 | 5.28 ± 1.41 | 0.001 |
| 8 h | 2.08 ± 0.87 | 4.28 ± 1.43 | 0.001 |
| 12 h | 1.67 ± 0.83 | 3.05 ± 1.09 | 0.001 |
| 24 h | 1.33 ± 0.68 | 2.03 ± 0.88 | 0.001 |
| First analgesic request (h) | 2.86 ± 0.58 | 3.33 ± 0.42 | 0.533 a |
| Meperidine (mg/d) | 14.72 ± 2.29 | 38.47 ± 1.54 | 0.001 |
Demographic Information and Pain and Analgesic Data of Patients
The mean duration of surgery in group A did not have a significant difference (P = 0.834).
The mean postoperative VAS scores at 2, 8, 12, 24 hours in groups A and B are depicted in Table 1. The analysis of data by repeated measures ANOVA showed a significant difference between the two groups (P = 0.001).
There was no significant difference between the two groups in terms of administering meperidine for the first time (P = 0.533). The mean meperidine administered during the first 24 hours after surgery in group A showed a significant difference (P = 0.001).
5. Discussion
Laparoscopic cholecystectomy is a frequent surgery even conducted as an outpatient surgery in many medical centers, and it is usually associated with severe postoperative pain. Many clinical studies have evaluated different analgesic modalities to reduce postoperative pain (33). This study aimed to evaluate the effect of intraoperative blood pressure on postoperative pain intensity of patients undergoing elective laparoscopic cholecystectomy under general anesthesia.
Some investigations have observed a relationship between high blood pressure during surgery and postoperative pain (34). In another study conducted on patients undergoing laparoscopic cholecystectomy, phenylephrine was used to induce intraoperative controlled hypertension, and postoperative pain and morphine requirements were evaluated (35). They concluded that the control group had higher pain score and needed more morphine for the alleviation of postoperative pain.
Another study investigated the effect of inducing acute mild arterial hypertension on postoperative analgesic requirements after laparoscopic ovarian cystectomy (36). The results showed that pain intensity and analgesic consumption in hypertensive patients (systolic blood pressure 20 - 30% higher than baseline) were less than the controlled group (systolic blood pressure 20 - 30% lower than baseline).
In this study, 72 patients undergoing general anesthesia for elective laparoscopic cholecystectomy were randomly assigned into two groups: Group A with higher than baseline preoperative blood pressure (MAP allowed to increase up to 20% higher than baseline MAP by inducing pneumoperitoneum) and group B with normal to low blood pressure (MAP deliberately controlled at a tight limit from normal baseline MAP values to 20% less than baseline by titrating TNG infusion). According to the results, group B had a higher pain score and more meperidine request 24 hours after the surgery.
Therefore, a higher MAP during surgery may be inversely correlated with the intensity of acute postoperative pain in these patients.
Guasti et al. studied the relationship between familial predisposing factor to hypertension in patients with a positive familial history of hypertension and the level of blood pressure and pain sensitivity. They argued that hypertension may increase the threshold of pain perception through stimulating and modulating baroreceptors, and thereby endogenous opiate system (37).
In a study conducted by Luo et al., the effects of uncontrolled preoperative essential hypertension on postoperative pain after major abdominal surgery was evaluated (38). The researchers divided 60 patients into two groups of hypertensive and normotensive undergoing abdominal surgery and recorded the postoperative morphine requirement and pain scores. According to the results, a higher blood pressure in hypertensive patients was related to less pain scores, and less opioids were required to suppress postoperative pain.
King et al. evaluated the relationship between blood pressure and acute postoperative pain in endodontic patients and found an inverse relationship between preoperative blood pressure and pain intensity after an endodontic procedure (39).
In 2013, a systematic review by Sacco et al. revealed that high blood pressure reduces acute pain, which is assumed to be due to the role of hypertension in stimulating baroreceptors, and thereby increasing endogenous opiates (40).
Chiang et al. conducted a prospective study to evaluate the relationship between hypertension and postoperative pain in 200 patients classified into three groups of normal blood pressure, hypertensive patients under treatment by antihypertensive medications, and uncontrolled hypertensive patients (34). They found a significant difference in the amount of analgesic medications required at first, second, and third postoperative days. The results of this study were in line with our study. However, we should consider the plausible confounding effect of antihypertensive medications used by a group of patients before study.
In a study conducted by Kholdebarin et al., patients with preexisting chronic hypertension who were under management by antihypertensive drugs and scheduled for total abdominal hysterectomy were randomized into two groups (41). A group with intraoperative blood pressure in the normal range and a second group with high blood pressure (stage 1 hypertension) during surgery. In this study, there was no significant difference between the two groups in terms of postoperative pain severity and morphine requirements 2, 4, 6, 12 after the surgery.
It was assumed that in both groups, the endogenous opioids may have been elevated due to preexisting chronic hypertension, and maintaining intraoperative blood pressure in normal or high range could not increase the level of endogenous opioids any more. Therefore, they did not find any difference in acute postoperative pain.
In contrast to some previous studies, we considered only ASA I patients in our study to eliminate the presumable effect of any preoperative confounding factors, like medication or comorbidities that may have a role in patient’s pain perception or hemodynamic variables, such as blood pressure or heart rate, that are compared between the two groups.
Although we used TNG to deliberately restrict MAP variations intraoperatively in the normal to low ranges in one group of patients, in the literature, there was no analgesic effect attributable to TNG (42). If TNG has any unknown analgesic effects, this effect is still in favor of our results, because the same group of patients who received TNG (group B) had more postoperative pain intensity and analgesic requirements in our study.
Also, we did not use drugs like phenylephrine to increase MAP in the other group (group A) because gas insufflation to produce pneumoperitoneum during laparoscopic surgery stimulates the sympathetic system per se, and thereby usually increases the blood pressure. So, in our study, we eliminated the confounding effect of any other drugs like phenylephrine (used in other studies) on the postoperative pain.
To consider the overall effect of both systolic and diastolic blood pressure on pain intensity, we applied mean arterial pressure in this study. To elucidate any confounding effect of hypnotic and analgesic drugs used intraoperatively in both groups, we used BIS monitoring to standardize the depth of anesthesia in all patients. So, anesthetic drugs were tailored according to BIS irrespective of patients’ groups.
5.1. Conclusions
Maintaining the intraoperative blood pressure in high range seems to ameliorate postoperative pain by some undetermined physiologic mechanisms. As Duschek proposed, an increased sensitivity to pain may be related to hypotension. Thus, we should also consider the likelihood of hyperalgesic effect of controlled hypotension (in group B) (43). Therefore, it is suggested that further investigations be accomplished to evaluate the probable hyperalgesic effect of controlled hypotension in comparison to normal blood pressure in patients undergoing surgery.
Accordingly, it is recommended that anesthetists avoid mild intraoperative hypotension and consider high blood pressure (up to 20% above baseline) during surgery as a preventive analgesic modality for postoperative pain.