1. Background
Pain control after cesarean section decreases the patient discomfort, duration of hospital stay, and hospital costs, as well as increases the speed of walking and patient satisfaction. Furthermore, adequate and rapid pain control after cesarean section has a positive impact on early breastfeeding, which contributes to uterine contractions in the postpartum period and facilitates the conditions to support the infant and feed him/her. There are several methods to control postoperative pain, including systemic analgesia (opioids and non-opioids) and local analgesic techniques (a neuraxial and local). Meperidine is the most common opioid used during labor. Nowadays, spinal anesthesia is an effective and safe approach with the help of anesthetics; it is also the most common method of applied anesthesia for performing cesarean section due to several advantages, including rapid onset, high probability of success, and minimum impact on mother and infant (1-3). Adding opioids to a local anesthetic through its intrathecal administration usually increases the postoperative analgesic effects. Spinal anesthesia using meperidine leads to a long period of analgesia after surgery, but its side effects, such as nausea, vomiting, hypotension, urinary retention, etc. are considered as restricting factors for its consumption (4).
2. Objectives
Given the facts, including the importance of pain control – especially in cesarean section – as well as the need for conducting further studies on drugs to replace meperidine in order to prevent side effects of injecting this drug (e.g., hypotension, vomiting, itching, and nausea) while maintaining its analgesic effects through its intrathecal administration in different methods and doses, the present study was carried out to compare the effects of spinal injection of single meperidine, meperidine-bupivacaine, and single bupivacaine on analgesia after elective cesarean section.
3. Methods
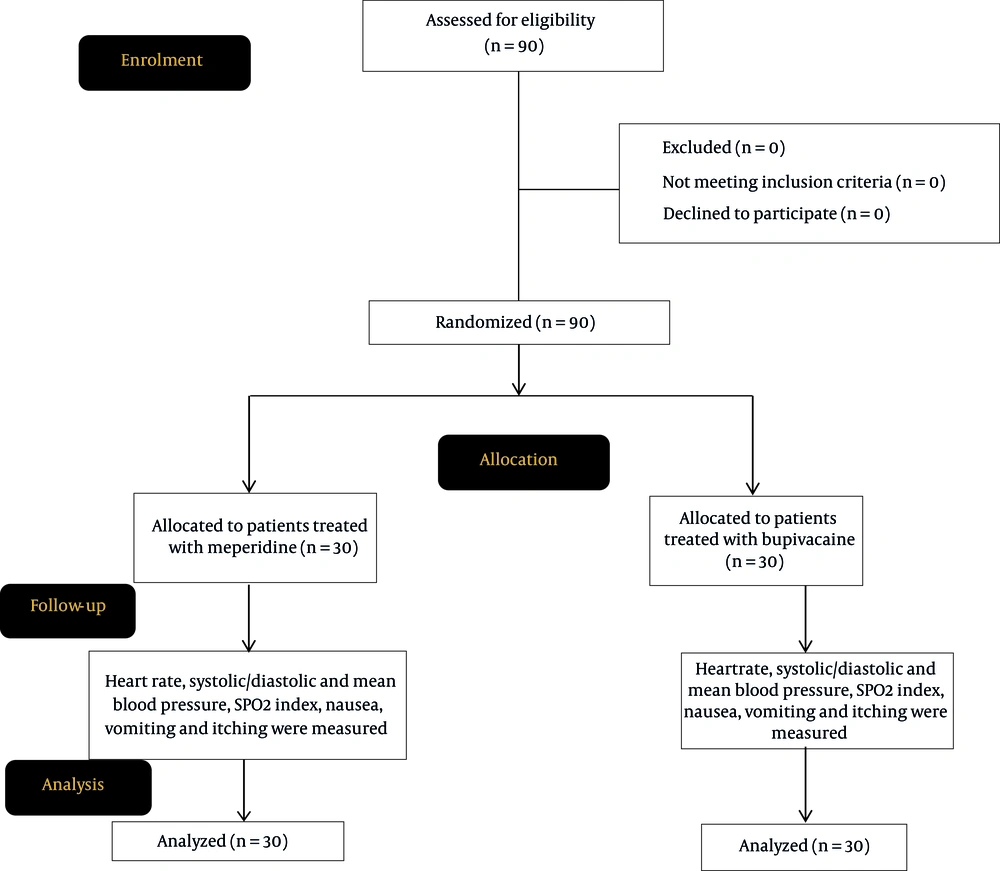
This clinical trial (Trial registrations IRCT20200413047056N2) was conducted in Valiasr Hospital from January 2021 to March 2021 after obtaining the code of ethics (Ir.bums.REC.1398.144). It mainly aimed to examine the level of postoperative analgesia in healthy patients undergoing elective cesarean section with spinal anesthesia by meperidine, bupivacaine, and a combination of these two drugs. The method and objectives of the study were fully explained to all patients, and they were included in the study after obtaining their informed consent. In this double-blind clinical trial and out of 90 sealed pockets, which included three classes of meperidine, bupivacaine, and a combination of meperidine and bupivacaine, one pocket was randomly selected by the patient, and the drug was prepared by an independent researcher (i.e., anesthesia technician). The data collection in recovery was performed by the recovery technician, and the data collection in the ward was done by the ward nurse who was unaware of the study groups. Inclusion criteria of the study were: (1) ASA 1 and ASA 2 patients (i.e., patients with healthy or mild controlled disease) aged between 20 to 40; (2) non-smokers and those not having drug addiction; (3) those with no history of hypertension and diabetes; (4) those having elective cesarean section; (5) those having no chronic pain; and (6) those having no mental and hysterical diseases. Exclusion criteria of the study, on the other hand, were: (1) those having emergency cesarean section; (2) those with placental abruption; (3) those with accreta; (4) those with severe bleeding during surgery; (5) those with uncontrolled comorbidities (ASA3 and above); (6) those having taken painkillers or anti-emetics 24 hours before the surgery; (7) those with skin infection at the injection site; (8) those with history of allergy to bupivacaine or meperidine; (9) those experiencing change in the type of anesthesia during the surgery; and (10) those receiving blood injection during the surgery.
After the patient entered the operating room, an intravenous line was established and one liter of fluid was administered; then, the vital signs (SpO2, ECG, BP SpO2, ECG, BP) were measured and recorded before spinal injection and immediately after anesthesia. The drug was prepared in similar syringes for three groups, so Group 1 received 100 mg of meperidine, similar to the study by Sangarlangkarn et al., Group 2 received 50 mg of meperidine and 5 mg of bupivacaine, and Group 3 received 10 mg of bupivacaine (5). After prepping and draping, the spinal anesthesia was performed by using a 25 G Quincke needle in the L4-L5 or L5-S1 intervertebral space in a sitting position. After the injection, the patient returned to the supine position immediately, and standard monitoring, including continuous pulse oximetry and ECG were carried out. Blood pressure was monitored every three minutes after the injection, and this procedure was continued up to the end of surgery. Hypotension or drop in systolic blood pressure to less than 90 mmHg or 25% reduction in basal blood pressure was treated with 10 mg of intravenous ephedrine. Patients received oxygen using a disposable plastic non-rebreathing mask connected to outlet anesthesia machine with flow of 6 to 8 liters; the patients' vital signs, including blood pressure, SpO2, and ECG were checked by the Saadat portable monitoring device. The patient was also asked about the presence of nausea, vomiting, headache, itching, and shortness of breath, and Apgar scores of the infant in the first and fifth minutes were recorded and compared in three groups. In case of itching, 4 mg of ondansetron was injected intravenously, but, in case of vomiting, 10 mg of metoclopramide was injected intravenously. Patients' pain was measured via VAS by marking a graduated ruler. If the patient had a pain score greater than 4, then 50 mg of diclofenac suppository was prescribed for the patient. Pain severity was assessed during 24 hours based on the mean number of drugs used. As for the patients who did not receive drug in each group, no pain was considered; for patients who used one suppository, pain was considered as mild pain; for patients who used two suppositories, pain was considered moderate; and for patients who used three suppositories or more, the pain was considered as severe pain. At the end of study, the mean amount of analgesia needed (diclofenac suppository) after cesarean section was assessed and recorded for all three groups; after collecting the data, they were entered to SPSS-19 software and the normal distribution of data was checked using Kolmogorov-Smirnov test. If the data had a normal distribution, ANOVA, Tukey post hoc test, and paired t-test were used. As for the variable of pain intensity due to its qualitative and rank nature and for quantitative variables in the case of the non-normal distribution of data, Friedman, Mann-Whitney and Kruskal-Wallis, and Wilcoxon tests were used.
4. Results
The flowchart of the study is presented in Figure 1. In the present study, 90 patients undergoing cesarean section were examined. Out of these 90 patients, 30 patients received meperidine injection, 30 ones received bupivacaine injection, 30 ones received meperidine plus bupivacaine injection. No significant statistical difference was observed among three groups in terms of the mean age of the study participants. According to the data presented in Table 1, a significant reduction in mean systolic blood pressure was observed in all three groups after the intervention (P < 0.001); the highest reduction regarding systolic blood pressure was observed in the meperidine group (3.7 mg) followed by the bupivacaine group (16.7 mg), whereas the lowest reduction in this regard was observed in the meperidine+bupivacaine group; and the difference between meperidine group and other two groups was significant (P = 0.001). A significant reduction was observed in all three groups in terms of mean diastolic blood pressure after the intervention compared to pre-intervention stage; the highest reduction was recorded in the meperidine group, and the mean changes regarding diastolic blood pressure were statistically significant in the meperidine group compared to other two groups. According to our data, a significant reduction in mean HR was observed in the meperidine group and the meperidine+bupivacaine group after the intervention compared to the pre-intervention stage, but the difference was not significant in the bupivacaine group. In addition, the mean HR in the meperidine group was significantly higher than those detected in the other two groups. According to the data presented in Table 2, the mean SpO2 index in the two groups of meperidine and meperidine+bupivacaine showed a significant decrease after the intervention compared to the pre-intervention stage; however, this difference was not observed in the bupivacaine group. Furthermore, the mean changes in SpO2 in the meperidine group were significantly higher than those in the other two groups. The prevalence of nausea, vomiting, and itching in the meperidine group was higher than that in the other two groups, but dyspnea in the meperidine+bupivacaine group was higher than that in the other two groups (P = 0.032) (Table 3). According to our data, 53.3% of patients in the meperidine group had absolute analgesia and needed no analgesia. Following statistical calculation, however, no significant difference was recorded for the frequency distribution of diclofenac administration in the three groups (Table 4).
| Study Group | Time | Paired t-test Result | Changes | |
|---|---|---|---|---|
| Before Intervention | After Intervention | |||
| Systolic blood pressure | 84.13 ± 4.5 | 58.12 ± 1.6 | t = 4.14, P < 0.001 | -26.15 ± 3.2 |
| Meperidine | 3.12 ± 5.132 | 102.10 ± 8.5 | t = 4.14, P < 0.001 | -30.11 ± 7.6 |
| Bupivacaine | 3.13 ± 1.131, | 114.15 ± 4.3 | t = 73.5, P < 0.001 | -16.15 ± 7.9 |
| Meperidine+bupivacaine | 123.11 ± 7.5 | 112.17 ± 5.3 | t = 02.4, P < 0.001 | -11.15 ± 2.2 |
| Test result ANOVA | F = 11.5, P = 0.008 | F = 4.5, P = 0.006 | F = 7.14, P < 0.001 | |
| Tukey post hoc test result | ||||
| Meperidine with Meperidine+bupivacaine | P = 0.008 | P = 0.008 | P = 0.001 | |
| Meperidine with bupivacaine | P = 0.032 | P < 0.001 | ||
| Diastolic blood pressure | ||||
| Meperidine | 84.13 ± 4.5 | 6.12 ± 1.58 | t = 48.9, P < 0.001, | -26.15 ± 3.2 |
| Bupivacaine | 80.12 ± 3.9 | 7.15 ± 3.65 | t = 44.4, P < 0.001, | -18 ± 15.5 |
| Meperidine+bupivacaine | 77.11 ± 5.9 | 8.12 ± 9.68 | t = 31.3, P = 0.003 | -8.14 ± 6.3 |
| Test result ANOVA | F = 18.2, P = 0.012 | F = 75.4, P = 0.011 | F = 23.9, P < 0.001 | |
| Tukey post hoc test result | ||||
| Meperidine with Meperidine+bupivacaine | P = 0.009 | P = 0.022 | ||
| Meperidine with bupivacaine | P < 0.001 | |||
| Heart rate | ||||
| Meperidine | 111 ± 9.5 | 84.18 ± 3.2 | t = 96.6, P < 0.001 | -27.21 ± 6.7 |
| Bupivacaine | 99.14 ± 8.4 | 96.19 ± 5.3 | t = 88.0, P = 0.038 | -3.20 ± 2.1 |
| Meperidine+bupivacaine | 98.14 ± 7.8 | 87.16 ± 4.6 | t = 28.3, P = 0.003 | -11.18 ± 3.9 |
| Test result ANOVA | F = 91.7, P = 0.001 | F = 75.3, P = 0.028 | F = 2.11, P < 0.001 | |
| Tukey post hoc test result | ||||
| Meperidine with Meperidine+bupivacaine | P = 0.004 | P = 0.117 | P < 0.001 | |
| Meperidine with bupivacaine | P = 0.002 | P = 0.007 | ||
a Values are expressed as mean ± SD.
| Study Group | Time | Paired t-test Result | Changes | |
|---|---|---|---|---|
| Before Intervention | After Intervention | |||
| Meperidine | 96.1 ± 4.88 | 92.2 ± 1.6 | t = 14.8, P < 0.001 | -4.2 ± 23.8 |
| Bupivacaine | 95.3 ± 5.6 | 95.2 ± 5.4 | t = 42, P < 0.97 | -0.4 ± 3.4 |
| Meperidine+bupivacaine | 97.1 ± 5.8 | 96.2 ± 5.2 | t = 56.4, P < 0.001 | -2 ± 1.4 |
| Test result ANOVA | F = 42.4, P = 0.015 | F = 3.27, P = 0.001 | F = 2.13, P < 0.001 | |
| Tukey post hoc test result | ||||
| Meperidine with bupivacaine | P = 0.011 | P < 0.001 | P < 0.001 | |
| Bupivacaine with meperidine+bupivacaine | P < 0.001 | P = 0.001 | ||
a Values are expressed as mean ± SD.
| Variables | Meperidine | Bupivacaine | Meperidine+Bupivacaine |
|---|---|---|---|
| Nausea and vomiting | |||
| No | 5 (16.7) | 13 (43.3) | 19 (63.3) |
| Yes | 25 (83.3) | 17 (56.7) | 11 (36.7) |
| Headache | |||
| No | 30 (100) | 30 (100) | 28 (93.3) |
| Yes | 0 (0) | 0 (0) | 2 (6.7) |
| Itching | |||
| No | 7 (23.3) | 26 (86.7) | 26 (86.7) |
| Yes | 23 (76.7) | 4 (13.3) | 4 (13.3) |
| Dyspnea | |||
| No | 30 (100) | 26 (86.7) | 24 (80) |
| Yes | 0 (0) | 4 (13.3) | 6 (20) |
a Values are expressed as No. (%).
| Number of Diclofenac Suppositories | Groups | Total | ||
|---|---|---|---|---|
| Meperidine | Bupivacaine | Meperidine-Bupivacaine | ||
| 0 | 16 (53.3) | 14 (46.7) | 10 (33.3) | 40 (44.4) |
| 1 | 7 (23.3) | 9 (30) | 8 (26.7) | 24 (26.7) |
| 2 | 5 (16.7) | 4 (13.3) | 4 (13.3) | 13 (14.4) |
| ≥ 3 | 2 (6.7) | 3 (10) | 8 (26.7) | 13 (14.4) |
a Values are expressed as No. (%).
5. Discussion
Spinal analgesia can be a logical, rapid onset, and safe method for blocking pain, which facilitates rapid recovery, especially in lower limb surgeries (6-9). Using multi-modal analgesia not only does give rise to sufficient pain relief after caesarean section, but also decreases the amount of the analgesic drug doses required for postoperative pain relief and their side effects (10). In the present study, the mean systolic blood pressure after the intervention showed the highest reduction in the meperidine group, but it showed the lowest reduction in the meperidine plus bupivacaine group (P < 0.001), indicating the significant effect of meperidine on reducing blood pressure in patients after cesarean section. Furthermore, meperidine was found to significantly contribute to reducing diastolic blood pressure in patients from meperidine group compared to patients from the other two groups and to cause a significant reduction in diastolic blood pressure in patients after cesarean section; the difference between meperidine group and other groups was significant (P < 0.001). In a similar study conducted by Shami et al. to investigate the intrathecal effect of meperidine on tremor in patients undergoing cesarean section and spinal anesthesia, 150 patients were randomly divided into three groups (11). Spinal anesthesia was performed in the control group using 12.5 mg of bupivacaine 0.5% and 0.5 mL of saline 0.9%. The same dose of bupivacaine along with 5 mg of meperidine (group 2) or 10 mg of meperidine (group 3) was used. Then hemodynamic changes (i.e., systolic and diastolic pressure and heart rate), central temperature, and tremor were measured. According to the results, no significant differences were detected among three groups in terms of hemodynamic changes and central temperature changes. Tremor was significantly reduced in the meperidine group compared to the control group. In general, according to the results of their study, it was suggested that meperidine had the potential to reduce tremors during cesarean section without causing side effects. In our study, in contrast to the results of their study, hemodynamic changes in the meperidine group were significantly reduced. Comparing the means of patients' heart rate, meperidine had the greatest effect, so the mean heart rate in patients decreased significantly after using it (P < 0.001), but no significant difference was observed in the case of bupivacaine group (P = 0.38); this difference in the case of meperidine plus bupivacaine group was also significant (P = 0.003).
In a similar clinical trial study by Shrestha et al. on 60 candidate women, the effects of spinal injection of bupivacaine and meperidine on hemodynamic factors during surgery and analgesia after performing cesarean section were examined and compared (12). Patients were randomly divided into two groups, and hemodynamic factors, as well as the duration of analgesia after surgery in two groups, were recorded and statistically analyzed. There was no statistically significant difference between the two groups in terms of hemodynamic indices (i.e., heart rate and blood pressure); however, the duration of analgesia (8 and a half hours) was longer in the meperidine group and was significantly different compared to that in the bupivacaine group (2 hours and 36 minutes). As for the mean SpO2 and based on the statistical results obtained in the two groups of meperidine and meperidine plus bupivacaine, moreover, a significant reduction was observed after the intervention compared to the pre-intervention, but no difference was discovered in the bupivacaine group. Khan et al. examined the effects of different doses of meperidine in cesarean section patients (13). In the given study, 72 patients receiving spinal anesthesia were assigned to case and control groups, including bupivacaine (control group), bupivacaine plus meperidine (case group). Then blood pressure, heart rate, and pulse oximetry (SpO2) of the subjects were examined, but no significant difference was detected between the groups in terms of blood pressure, heart rate, and pulse oximetry. Their study results also showed that meperidine had no effect on reducing hemodynamic parameters. In our study, the blood pressure, heart rate, and SpO2 decreased significantly in the meperidine group.
According to our study results, the mean of times needed for analgesia after the intervention was not significantly different from that before the intervention (P = 0.14). In a similar study by Murto et al., the effect of adding a low dose of meperidine to lidocaine on increasing the duration of analgesia after prostatectomy in patients under spinal anesthesia was investigated (14). In this clinical trial, patients were assigned to three groups, where the first group received intrathecal injection of lidocaine 5%, the second group received lidocaine plus meperidine at a dose of 0.15 mg/kg, and the third group received lidocaine plus meperidine at a dose of 0.30 mg/kg. According to their study results, adding meperidine at a dose of 0.3 mg/kg to lidocaine increased the duration of analgesia and reduced the need for opioids. In another study by Jabalameli et al., the effects of subcutaneous meperidine and tramadol as well as subcutaneous bupivacaine, on pain after performing cesarean section and using opioids were examined and compared (15). Their study findings revealed that tramadol and meperidine had equal effects, and the analgesic effect of tramadol and meperidine was higher than that of bupivacaine. Although the drug was administrated subcutaneously, the analgesic effects of meperidine on post-cesarean section pain, which is actually equivalent to methadone and more effective than bupivacaine, were demonstrated by the given study, which was consistent with our stud result in this regard. The levels of nausea, vomiting and itching in patients from meperidine group were higher than those in patients from the other two groups, but dyspnea in the meperidine+bupivacaine group was higher compared to that in the other two groups (P = 0.032). In a study similar to ours, Kouzegaran et al. investigated the effect of adding 5 mg of meperidine to 10 mg of bupivacaine on spinal anesthesia on post-cesarean section pain (16). In the given trial conducted on 40 patients aged 20 to 40 years and candidate for cesarean section, the patients were randomly assigned to two groups of meperidine-bupivacaine and normal saline-bupivacaine. The drugs were administered based on the mentioned dose under spinal anesthesia, and the analgesia index was evaluated 2, 12, and 24 hours after the surgery. Their study results revealed that the pain was more severe 12 and 24 hours after the surgery in the normal saline group; however, no significant difference was observed between two groups in terms of nausea, vomiting, and itching. In the given study, in contrast to our study, no significant difference was observed in nausea, vomiting, and itching before and after taking meperidine, while their levels were increased in our study. In a study by Udonquak et al., the effects of meperidine and bupivacaine on 52 patients in need of anesthesia for short-term surgery were evaluated (17). In the given study, the patients were randomly assigned to two groups: the first group received 1 mg/kg of spinal meperidine and 2.5 mL of bupivacaine 0.5%, and the cases such as complete motor recovery, plantar flexion, as well as levels of nausea and vomiting before and after the intervention were assessed. According to the statistical results of this study, vomiting and nausea were not observed in either group after the intervention; however, itching was found in the meperidine group, but it was not observed in the bupivacaine group. Finally, the results of their study indicated that meperidine had a shorter recovery time than bupivacaine and produced no observable side effects shortly after the surgery. In our study, in contrast to their study, nausea and vomiting were found in the meperidine group, but the itching, similar to their study, was observed in the meperidine group.
5.1. Conclusions
It was concluded that the combination of pethidine and bupivacaine had a significant effect on stabilization of hemodynamic parameters (i.e., heart rate, diastolic, and systolic blood pressure as well as mean arterial blood pressure). It was also found that the given combination improved the Apgar score five minutes after cesarean section compared to one minute after it. Furthermore, the prevalence of nausea, vomiting, and itching in the pethidine group was discovered to be higher than those in the other two groups. Due to almost equal performance of pethidine and pethidine plus bupivacaine in analgesia, the stabilization of other hemodynamic indices in the pethidine plus bupivacaine group, as well as the decline in the prevalence of nausea, vomiting, and itching, therefore, this combination may have been a good alternative to pethidine.
5.2. Limitations
In our study, a high-dose pethidine (meperidine) was used alone, which was associated with relatively high incidences of nausea and vomiting. Therefore, it was recommended that lower doses of pethidine alone should be used in later studies in order to reduce the incidences of side effects such as nausea and vomiting.