1. Background
Despite a better understanding of the mechanisms of postoperative pain and progress in pain management methods, improperly controlled postoperative pain remains a significant and unsolved health problem (1). Attempts have been to control pain and anxiety to minimize patient discomfort and distress and improve the recovery (2, 3).
Protective analgesia is administered before surgery to reduce the pain experienced and opioid consumption afterward (4). Adjuvant drugs, such as gabapentin or its congener pregabalin, have been tried and tested as protective analgesics (5, 6). Other studies have used different medications, such as melatonin and acetaminophen, for controlling pain during the regional block (7).
Pregabalin, an r-aminobutyric acid analog that binds to the α2-δ subunit of presynaptic voltage-gated calcium channels in the central nervous system (CNS), has anticonvulsive, analgesic, and anti-anxiety properties (8). Oral pregabalin administered preoperatively is reported to result in reduced acute postoperative pain, decreased postoperative analgesic consumption, and prolonged anesthesia (8, 9). Based on its uncomplicated pharmacokinetics and drug profile, it is frequently used before surgery to reduce acute postoperative pain (9). The efficacy of pregabalin as a premedication needs to be further established, especially for ophthalmic procedures. Additionally, there is a limited number of studies about the effectiveness of pregabalin in regional anesthesia (8).
2. Objectives
This study was designed to examine the effect of a single dose of pregabalin on postoperative pain, anxiety, and analgesia after vitrectomy performed under the peribulbar block (PB) and to assess the satisfaction of the patients as well as the surgeons.
3. Methods
3.1. Design, Setting, and Patients
This randomized, double-blinded, placebo-controlled study was conducted at Magrabi Eye, ENT, and Dental Center, Doha, Qatar after approval by the Hospital Ethics Committee of Magrabi Center, Doha, Qatar, on 58 adult patients aged 37 - 75 years, who met status I and II of the American Society of Anesthesiologists and scheduled for elective retinal surgeries, namely vitrectomy, under the PB.
3.2. Patients’ Randomization
The patients were randomly divided into case and control groups. The case (pregabalin) group involved 30 patients who received LYRICA® CR pregabalin extended-release tablets (150 mg) as premedication, while the control (placebo) group involved 28 patients who received placebo as premedication. Both drugs were administered orally with sips of water 90 minutes before surgery. An independent technician was responsible for computer-generated codes to be able to obtain complete randomization. These codes were kept in sealed envelopes, which were sequentially numbered and opaque. A nurse who was not involved in the study opened these envelopes immediately before administration.
3.3. Inclusion and Exclusion Criteria
Exclusion criteria were patients’ refusal to regional anesthesia, patients more than 75 years old, pregnancy, breastfeeding women, bleeding tendency, history of drug abuse, history of heart failure, taking calcium channel blockers, renal insufficiency, neurological or psychiatric disorders, allergy to the study medication, and intake of narcotics, pregabalin or benzodiazepines within 24 h before the study. Patients aged 18 years and older who consented to participate in this study and who do not have exclusion criteria were included in our study.
3.4. Sample Size Calculation
The sample size was calculated based on the information from a study by Abdul-Latif et al. (10), who found that in each study group, a sample size of 22 patients was needed for detection of a decrease in the visual analogue scale (VAS) score of 20 mm at 80% power.
3.5. Definitions, Procedures, and Surgical Technique
Upon arrival to the operating room, the level of sedation based on Ramsay sedation scale was recorded, with 1 = agitated, anxious or restless, 2 = oriented, cooperative and calm, 3 = obey orders, 4 = abrupt response, 5 = a lazy response, and 6 = no response. When the sedation score was 4 or more, we considered the patients as sedated. The anxiety scores were also expressed in terms of the verbal anxiety scores where a score of 0 to 10 was given (completely calm = 0, the worst possible anxiety = 10). Patients with an anxiety level of 5 or more received midazolam (dormicum, 0.02 mg/kg). Patients were monitored with an electrocardiogram for noninvasive arterial blood pressure and pulse oximetry.
PB was done by the same anesthetist to all patients using 2.5 mL lidocaine 2% and hyaluronidase (150 IU) plus 7.5 mL of chirocaine (25 mg/10mL ampoules that contained levobupivacaine and hydrochloride; Abbott Laboratories Limited/AbbVie Biopharmaceuticals) and after the injection of 5mg/mL into the PB space, the site of injection was percutaneous in the inferior orbital margin and in the same line with the inferior lacrimal canaliculus. Also, needle 25G × 5/8″ (0.50 × 16 mm) was advanced anteroposteriorly for the half of its length (never more than 10 mm) and then, in an oblique direction toward the optical foramen.
Negative aspiration was done, followed by a slow injection of 6 mL of the local anesthetic solution, the volume was adjusted for each patient. The injection was discontinued when the eyelid fill appeared, accompanied by a feeling of full orbit. A 30 mmHg Honan balloon for 10 minutes was used for mechanical orbital compression.
Akinesia was evaluated in the 4 quadrants using a scoring system consisting of 3 points from 0 - 2 (0 = akinesia, 1 = partial akinesia, and 2 = normal movement), giving a maximal score of 8 for the 4 muscles. Sensory block was assessed according to the abolition of the corneal reflex. The local anesthetic (3 mL) was given in the non-affected quadrant if the eye was still kinetic after 10 minutes. The block was defined to be successful when the akinesia score was 3 or less.
Complications if any, were recorded. Need to supplement, duration of anesthesia, and pain during needle insertion were assessed using the VAS score, which is a numerical scale scoring from 0 to 100, where 0 means no pain and 100 represents the worst pain.
A pillow was placed below the knees of the patient to reduce any discomfort in the lower back. Oxygen supply (4 liters) through nasal cannula was applied to all patients, and a blinded observer assessed all measures.
At the end of the operation, the surgeon's satisfaction with the patient's cooperation during the operation was evaluated according to the satisfaction score on a four-point scale, with 1 = bad, 2 = fair, 3 = good, and 4 = excellent. A blinded anesthetist to the group assignment rated the quality of the cooperation on this numerical scale: no pain complaint, calm, and cooperative (4); minor complaint without the use of additional analgesics (3); pain complaint requiring additional analgesics or sedation (2); and unsuccessful and the need for transition to general anesthesia (1).
Upon arrival to the post-anesthesia care unit (PACU) and while patients were connected to the monitors, satisfaction was rated according to satisfaction score. All patients were followed for 2 hours postoperatively for the presence of postoperative pain and the need for analgesics. Paracetamol (1000 mg) was given in case of postoperative pain.
3.6. Statistical Analysis
We analyzed data using SPSS (25 and described quantitative data as mean ± SD and range, whereas qualitative data were described as numbers and percentages. Qualitative data obtained from groups were compared using the chi-square test. Chi-square was replaced by Fisher exact test if one expected cell was equal to or less than 5. Also, quantitative variables (parametric data) were compared using the t-test. Shapiro-Wilk test was used to assess the normality of the variables. Those variables having non-Gaussian distribution were transformed using log transformation. We considered a P-value of < 0.05 significant.
3.7. Ethical Approval
This trial was approved by the Institutional Review Board of Magrabi Eye, ENT and Dental Center, Doha, Qatar.
4. Results
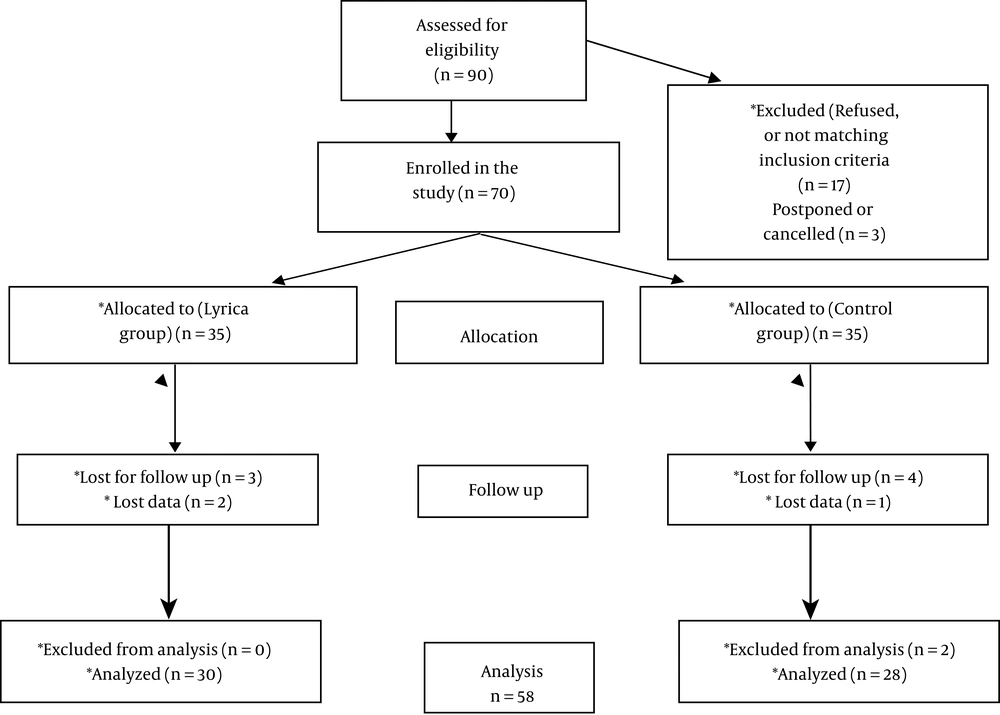
A total of 58 patients were involved in this study. The pregabalin group was composed of 30 cases who received pregabalin (150 mg) as premedication, and the placebo group involved 28 patients who received the placebo. Flowchart of patients is presented in Figure 1. A comparison between the two groups with respect to demographic and operational data showed statistically insignificant differences between both groups (Table 1).
| Variables | Pregabalin (n = 30) | Placebo (n = 28) | P-Value |
|---|---|---|---|
| Age | 55 ± 9.7 | 61.2 ± 13 | > 0.05 |
| Body weight | 74 ± 12.7 | 72.9 ± 11 | > 0.05 |
| Gender | > 0.05 | ||
| Male | 16 (53.3) | 12 (42.9) | |
| Female | 14 (46.7) | 16 (57.1) | |
| Type of surgery | |||
| Pars plana vitrectomy (PPV) | 03 (10) | 04 (14.28) | |
| PPV + scleral buckling (SP) | 09 (30) | 07 (25) | |
| PPV + IOL implantation | 11 (36.67) | 12 (42.86) | |
| PPV + IOL + silicon oil injection | 07 (23.33) | 05 (17.85) | |
| Side of operation | > 0.05 | ||
| Right | 13 (43.3) | 14 (50) | |
| Left | 17 (56.7) | 14 (50) | |
| Duration of surgery | 148 ± 23 | 148.7 ± 24 | > 0.05 |
Demographic and Operative Data a
Upon arrival to the operating room (OR), patients who received pregabalin had a significantly higher sedation score (3 ± 0 vs. 2 ± 0.65, respectively; P < 0.05), and a significantly less anxiety score (3 ± 1.3 vs. 5 ± 1.6, respectively; P < 0.001) compared to the control group. During needle insertion for (PB) patients in the pregabalin group have less pain compared to the control (32 ± 15 vs. 44 ± 15; P < 0.05) (Table 2).
| Variables | Pregabalin (n = 30) | Placebo (n = 28) | P-Value |
|---|---|---|---|
| Sedation score | 3 ± 0.8 (2.71 - 3.29) | 2 ± 0.65 (1.76 - 2.24) | < 0.05 |
| Pain (VAS) | 32 ± 15 (26.6 - 37.4) | 44 ± 15 (38.4 - 49.6) | < 0.05 |
| Anxiety score | 3 ± 1.3 (2.54 - 3.46) | 5 ± 1.6 (4.41 - 5.59) | < 0.001 |
Comparison of the Studied Groups with Regard to Sedation, Pain During Injection, and Anxiety Scores a
On the other hand, the pregabalin group had significantly higher cooperation and patient satisfaction scores (3.2 ± 0.7 and 3.8 ± 0.4, respectively) compared to the placebo group (2.8 ± 0.7 and 3.4 ± 0.5, respectively) with a significant difference among them when using the unpaired t-test. However, there was no significant difference with regard to surgeon satisfaction between both groups (Table 3).
| Variables | Lyrica (n = 30) | Placebo (n = 28) | P-Value |
|---|---|---|---|
| Patient cooperation | 3.2 ± 0.7 (2.95 - 3.45) | 2.8 ± 0.7 (2.54 - 3.06) | < 0.05 |
| Patient satisfaction | 3.8 ± 0.4 (3.66 - 3.94) | 3.4 ± 0.5 (3.21 - 3.58) | < 0.05 |
| Surgeon satisfaction | 3.8 ± 0.4 (3.66 - 3.94) | 3.6 ± 0.5 (3.42 - 3.79) | > 0.05 |
Comparison of the Studied Groups with Regard to Patient Cooperation and Surgeon and Patient Satisfaction Scores a
Comparing both groups regarding the need for midazolam (dormicum) intraoperatively to treat patients’ anxiety showed that the placebo group showed a higher frequency of the need for midazolam compared to the pregabalin group (19 vs. 5; P < 0.001) (Table 4). Moreover, the need for postoperative analgesia was more in the placebo group two hours postoperatively with a highly significant difference in between using the Fisher exact test.
| Variables | Pregabalin, N = 30 | Placebo, N = 28 | P-Value |
|---|---|---|---|
| Receiving dormicum | < 0.001 | ||
| No | 25 (83.3) | 9 (32.1) | |
| Yes | 5 (16.7) | 19 (67.9) | |
| Need to Analgesic | < 0.001 | ||
| No | 25 (83.3) | 14 (50) | |
| Yes | 5 (16.7) | 14 (50) |
Comparison of the Studied Group with Regard to the Need for Intraoperative Dormicum and Postoperative Analgesics a
5. Discussion
In the current study, we recorded the level of sedation based on the Ramsay sedation scale, which is useful in assessing the clinical effects of sedative agents (11, 12). Our results are compatible with the literature where those administered with pregabalin premedication experienced less pain during the procedure, as well as higher sedation scores and low anxiety levels, especially in other ophthalmic surgeries (13, 14). We administered a single, uniform dose of pregabalin (150 mg) alone in this study, but other studies have used different titrations and/or multimodal therapies. These regimens have been helpful in determining the best possible combination for effective postoperative pain management.
Jokela et al. compared patients’ postoperative response following the administration of pregabalin premedication (75 or 150 mg) one hour before surgery and reported better analgesia with the latter dose (15). However, in another study, decreased postoperative pain scores were reported with pregabalin premedication (300mg) in patients undergoing total hip arthroplasty (16). This may lead to accepting the ‘higher dose, higher efficacy’ hypothesis. However, with the potential of pregabalin as an addictive drug discussed below, close regulation is needed, especially in vulnerable populations (17, 18). Ideally, it is recommended not to take doses > 600 mg/day orally (19). In their comparison of administering pregabalin alone to patients undergoing septoplasty with those given pregabalin and dexamethasone combination, Demirhan et al. reported no significant difference in the outcome with the addition of dexamethasone except the within the hour after surgery (20).
We administered a single dose of pregabalin premedication to avoid unwarranted complications during vitrectomy, which is a procedure mostly done in elderly or high-risk individuals.
In their systematic review of over twenty trials involving different analgesics after photorefractive keratectomy, Faktorovich et al. concluded that tetracaine 1% and nepafenac 0.1% had the most analgesic effect among the different classes of analgesics, including nonsteroidal anti-inflammatory drugs (NSAIDs), opiates, acetaminophen, gabapentin, and pregabalin used in other studies. Their increased efficacy may increase by the potential side effect of delayed corneal epithelial repair. Re-epithelialization was slower in studies involving topical NSAIDs and anesthetics compared to other analgesics tested against placebo. Therefore, the authors advised avoiding the former despite increased efficacy in controlling pain (21).
The relatively simple and linear pharmacokinetics of pregabalin cannot make it seem like a ‘pharmaceutically elegant’ (9) choice for postoperative pain management.
Pregabalin is, however, associated with dizziness and somnolence. This does raise concern about its use among the elderly population (9, 22). Like other gabapentinoids, pregabalin also has the potential for abuse, especially by patients with substance use disorders (SUDs). Therefore, its use must be carefully regulated and monitored (17, 18).
Our study also showed that the need for postoperative analgesia was more in the placebo group compared to the group receiving pregabalin. This is also congruent with the findings in the literature, where the duration of analgesia was prolonged postoperatively in cohorts administered with pregabalin (23, 24).
The patients receiving placebo displayed a greater need for midazolam intraoperatively to alleviate anxiety in our study. Owing to its inhibition of excitatory neurotransmitters at the calcium channels, pregabalin is considered a first-line anxiolytic for generalized anxiety disorder (GAD) (25). It trumps the use of SSRIs and SNRIs (25). It is the same mechanism, which allows pregabalin to allay anxiety among patients undergoing surgical procedures. Studies have shown improvement in anxiety scores with the use of gabapentin analogs preoperatively (26, 27).
Although this study was done to bridge the gap in literature on assessing pregabalin effectiveness in reducing postoperative pain and improving post-surgical outcomes in ophthalmic procedures following local anesthesia, we faced some limitations. Firstly, only a single uniform dose of pregabalin (150 mg) was tested for assessing its efficacy; hence, a comparative analysis to evaluate the efficacy of different allowable doses could not be executed. Secondly, patients were evaluated for outcomes only 2 hours after the procedure, preventing the possibility of studying any long-term effects of pregabalin. Thirdly, no comparison was done between preoperative and postoperative pain and anxiety scores.
5.1. Conclusion
In conclusion, the present study reported a significant reduction in pain and anxiety in patients who received a single dose of pregabalin prior to a vitrectomy under local anesthesia. Although our results replicate several other studies, additional efforts are needed to establish pregabalin as an effective postoperative anxiolytic and analgesic agent in ophthalmic surgery under local anesthesia.