1. Background
Difficult airway management is one of the significant challenges in pediatric anesthesia (1-3). The difficult airway in children can quickly turn into a greatly serious situation that may lead to unfavorable and irreversible brain consequences that could even be life-threatening (2, 4). Severe complications of the difficult airway include brain injury, cardiac arrest, and death (1, 5, 6)
Pediatric patients have significant anatomical and physiological differences compared to adults, which affect the clinical judgment of the anesthesiologist to assess difficult airways (7, 8). Difficult intubation in children compared to adults causes a rapid decrease in arterial oxygen saturation in children leading to a reduction in the opportunity for intubation (5). Therefore, early detection of difficult airways, preparing special equipment, and having exceptional skills in pediatric airway management are vital for the anesthesiologist (9, 10).
There has been a significant difference between the prevalence and severity of difficult airways complications in predictable and unpredictable cases in several studies. Paying attention to these predictive factors and performing safe intubation in children under two years of age reduces the complications of the difficult airway (11-14). In previous studies on adults, some anatomical scales, such as acromio-axillo-suprasternal notch index (AASI), stern omental distance (SMD), mouth opening (MO), and neck circumference (NC) have been reported as reliable predictors of difficult airways and intubation (15, 16).
2. Objectives
Since there is no public agreement on the significant predictors of difficult intubation in children, this study was designed to examine anatomical scales (SMD, AASI, MO, and NC) in children under two years.
3. Methods
After approval of the Isfahan University of Medical Sciences Ethics Committee (code No.:1399.433), all parents signed the written informed consent. A total of 405 patients with the American Society of Anesthesiologists physical status I & II scheduled for surgery under general anesthesia with endotracheal intubation were included in this prospective descriptive-analytical study conducted in Imam Hossain Hospital, Isfahan. Inclusion criteria were all children under two years of age and candidates for elective surgery under general anesthesia with endotracheal intubation. Exclusion criteria included emergency surgery, previous neck surgery, previous head and neck radiotherapy, patients with a neck mass, and patients with contraindications of neck movement.
At first, age, sex, and weight were measured and recorded. To reduce separation anxiety, children over six months of age received midazolam at a dose of 0.01 mg/kg intravenously. The patient was transferred to the operating table, and standard anesthesia monitoring (noninvasive blood pressure (NIBP), electrocardiogram (ECG), blood oxygen saturation (SPO2), and temperature) was done. After controlling the vital signs and condition of the patient, the four predictive test measurements were accomplished by two trained anesthesiologists on all patients as follows:
1-AASI: a) A line was drawn vertically from the top of the acromion process to the superior border of the axilla at the pectoralis major muscle named as line A.
b)The second line was drawn perpendicular to line A from the suprasternal notch named line B.
c)Line C was defined as the portion of line A laid above where line B bisects line A. AASI was calculated as the ratio of c to A (C/A) (16).
2-SMD: SMD extension was measured as the straight distance from the upper border of the manubrium sterni to the mentum, with the head in full extension and the mouth closed.
3-MO: The distance between the upper and lower incisors at the midline when the mouth was opened.
4-NC: Neck circumference at the level of the cricoid cartilage was measured.
General anesthesia was induced by fentanyl (1-2 mcg/kg), propofol (3 mg/kg), and cisatracurium (0.1-0.2 mg/kg). After 3 min of ventilation with a bag-mask ventilation and 100% oxygen, an experienced anesthesiologist blinded to the study intubated the patients in a sniffing position. The laryngoscopic view was graded with Cormack-Lehane (CL) grading system, which contains four grades: I: vocal cords visible, II: only posterior commissure or arytenoids visible, III: only epiglottis visible, and IV: none of the preceding visible. Difficult visualization of the larynx (DVL) was defined as CL III or IV views on direct laryngoscopy, and easy visualization of the larynx (EVL) was defined as CL I or II views on direct laryngoscopy.
The IDS score was determined according to scientific criteria so that a value equal to zero indicated intubation in ideal conditions. Patients were divided into two groups based on IDS; patients with
IDS ≥ 4 were assigned to the difficult intubation group and patients with IDS < 4 were assigned to the easy intubation group (17).
Demographic information was collected in a predefined checklist. The researcher was also present as an observer during the intubation process and collected the desired information through a prepared list. No intervention was performed during the procedure, and there was no time waste or risk for the patient.
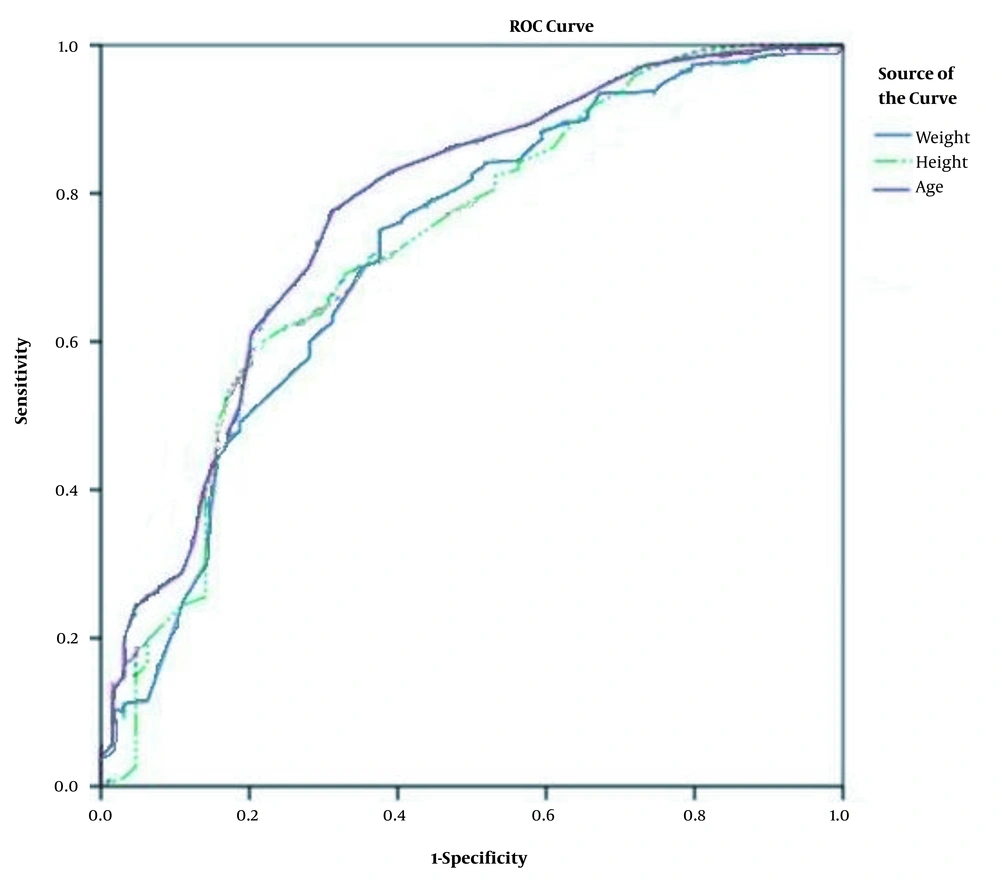
After collecting information, to analyze and compare the variables in the study groups, SPSS software version 25 was used using descriptive statistics, such as indicators of central tendency and also analytical statistics, including receiver operating characteristic (ROC) curve, Spearman's rank correlation coefficient, and Mann-Whitney U test were used. In all tests, a significant level of 0.05 was considered.
4. Results
In this study, 405 children under two years of age were examined, of whom 273 cases (67.4%) were boys, and 132 cases (32.6%) were girls. The age range of children was from 2 days to 24 months, with an average of 9.4 months and a standard deviation of 6.6 months. According to (Table 1), 69 children (17%) had difficult intubation, and 336 cases (83%) had not.
| Variable | Value | P Value |
|---|---|---|
| Age | ||
| Mean | 9.4 | |
| Standard Deviation | 6.6 | |
| Minimum, day | 2 | |
| Maximum, month | 24 | |
| Intubation, No. (%) | 0.48 | |
| Easy | 336 (83) | |
| Difficult | 69 (17) |
Frequency Distribution of Age and Intubation
The variables mentioned in (Table 2) were significantly lower in children with difficult intubation than in children with easy intubation (P < 0.05) and independently predicted difficult intubation. Also, the age < 6 month, weight < 5/9 kg, and height < 61 cm were predictors of difficult intubation in children. Based on the area under the curve, age, weight, height were significant predictors for easy and difficult intubation (P < 0.001). Although the values of SMD and NC were statistically significant, they had a small area under the curve and were ignored (Figure 1).
| Variable | Easy Intubation | Difficult Intubation | P Value | ||
|---|---|---|---|---|---|
| Mean | Standard Deviation | Mean | Standard Deviation | ||
| Age | 10.1 | 6.5 | 6.3 | 4.4 | < 0.001 |
| Weight | 7.9 | 2.5 | 5.9 | 2.7 | < 0.001 |
| Height | 69.4 | 10.4 | 61.3 | 11.8 | < 0.001 |
| SMD | 5.9 | 1.2 | 5.3 | 1.2 | < 0.001 |
| MO | 2.5 | 1.3 | 2.1 | 0.7 | 0.01 |
| AASI | 36.8 | 18.1 | 40.7 | 14.6 | 0.09 |
| Neck Circumference | 21.8 | 2.2 | 20.1 | 3.1 | < 0.001 |
Evaluation of Quantitative Variables Based on Easy and Difficult Intubation
5. Discussion
The primary purpose of our research was a comparison survey of some adult predictors of difficult intubation in children under two years of age. Our study showed that the incidence of difficult intubation is about 17%, which is higher than previous studies. In a study on 1,018 children with difficult airways, the intubation failure rate was reported to be 2% (9). In our referral hospital, children with cleft lip and palate were included in our study; thus, the frequency of difficult intubation was higher than in other studies. Also, the age < 6 month, weight < 5/9 kg, and height < 61cm were predictors of difficult intubation in children. Our results were similar to those found in anesthesia reference books (12, 18, 19).
Baudouin et al. showed that the Mallampati test and mouth opening were not predictive tests for difficult intubation in children less than 18 months (20). Aggarwal et al. found that the interincisor gap (MO) seemed to be an inadequate predictor of difficult intubation in children (21). These results are similar to our study and showed MO (P value = 0.01) with no significant predictive value for difficult intubation.
Kılıç et al. showed that interincisior distance is a predictor for difficult intubation in children (22). The reason for the difference between the results of their study with ours is that the average age of their study population was more than our study (six years vs. nine months).
In this study, we found that in children less than two years, AASI was not a predictor for difficult intubation (P value = 0.09). This finding is contrary to what has been emphasized in adult studies [15, 16]. The reason for this difference could be due to the difference in the anatomy of the upper respiratory tract and the fitness of the body in children compared to adults.
Our findings showed that SMD (mean ± SD = 5.3 ± 1.2, P value < 0.001) and NC (mean ± SD = 20.1 ± 3.1, P value < 0.001) were not strong predictors. This finding is similar to previous studies reporting that SMD may be a predictor for difficult intubation in children under two years (22, 23). Also, Figueroa-Uribe et al. studied the existing difficult airway predictive scales and their possible applicability in pediatric patients in the emergency department and showed that SMD was not helpful (24).
One of the limitations of our study was the cut-off values, which could not be confirmed in different age groups. One of the strengths of the present study is that reasonable sample size was presented. In addition, we tried to predict the difficult airway in children with the simplest and cheapest methods and also at the least possible time. We hope that according to the findings of this study, the necessary measures be taken to prevent severe complications and death of children, which is one of the tragedies of pediatric anesthesia and surgery.
5.1. Conclusion
The variables of SMD, NC, age, weight, and height can predict difficult intubation. These variables can be used simultaneously as a screening tool in airway evaluation before anesthesia to predict difficult intubation in children under two years of age. Unlike adults, AASI and MO are not predictors for difficult intubation in children.