1. Background
Nowadays, the incidence of CABG as a lifesaving intervention has been increasing worldwide (1, 2); however, there may be some intra and post-operative complications (3, 4). BG control during CABG is one of the main tasks of anesthesiologists (5). Higher fasting BG levels with intra-operative fluctuations are strong predictors of intra-and post-operative complications such as morbidity and mortality, neurologic damage, cardiac injury, surgical site infection, and longer hospital stay in diabetic and non-diabetic patients (6, 7). When BG values rise, hemoglobin molecules become glycosylated via a non-enzymatic reaction. This harmful process leads to the free radical formation (8). In this process, the administration of anesthesia drugs and insulin with proper dosage and timing, well-controlled diabetes other co-morbidities, CPB duration, and the use of inotropic agents and interventions to eliminate stress response to surgery stimulants are some of the effective factors (9-11).
2. Objectives
This study aimed to assess the quality of glycemic control in diabetic patients undergoing on-pump CABG surgery in an academic center in the north of Iran.
3. Methods
This prospective-descriptive study was performed at the Dr. Heshmat Hospital, an academic center affiliated with the Guilan University of Medical Science (GUMS), in 2020.
3.1. Inclusion Criteria
Diabetic patients undergoing isolated CABG surgery, aged 35 - 80 years and ASA class II & III.
3.2. Exclusion Criteria
Severe or unexpected complications changing the methods of anesthesia or surgery, patient not willing to submit their informed consent.
Arriving at the operating room, the patients underwent standard monitoring, and general anesthesia and surgery protocols were considered for these patients. BG was measured four times, before the induction of anesthesia (T0), before CPB (T1), during CPB (T2), at the end of CPB (T3), and at the end of surgery (T4). During the surgery, the surgeon took a sample from the coronary sinus and measured BG. Additionally, information addressing gender, age, BMI, ASA class, EF percentage, duration of surgery, duration of the CPB, the volume of administrated IV fluids during surgery, and urine volume at the end of surgery was also recorded. The target was to maintain BG in the range of 80 - 180 mg/dL. When BG > 200 mg/dL, a bolus of 4 units of insulin regular was administrated. For BG < 80 mg/dL, 50 mL/h of dextrose 5% was administered. BG was measured hourly using a touch glucometer, and the dosage was repeated until the reached values were < 200 mg/dL.
3.3. Statistical Analysis
The data were analyzed with SPSS software version 21. Chi-square, t-test, repeated measurement test, and ANOVA analysis were also used for the data analyses. Statistically, a P < 0.05 was set as the significance level.
4. Results
Fifty-five patients (34 (61.8%) men and 21 (38.2%) women) meeting the inclusion criteria took part in the survey. The participants’ mean age was 57.54 ± 9.29 years, 65.5% and 34.5% of whom were the ASA class II and the ASA class III. The mean years of diabetes was 10.6 ± 3.89, the mean duration of surgery was 181.09 ± 45.13 minutes, the mean urine volume was 1292.36 ± 505.8 mL, and the mean administrated IV fluids was 2268.2 ± 512.2 milliliters. Table 1 shows the patient’s demographic information and surgery characteristics. The mean BG was 222.18 ± 75.74 mg/dL, and the trend of BG variations from T0 to T4 was significant (P < 0.0001) (Table 2).
| Variables | Values |
|---|---|
| Gender | |
| Male | 34 (61.8) |
| Female | 21 (38.2) |
| Age (y) | 57.54 ± 9.29 |
| ≤ 60 | 35 (63.6) |
| > 60 | 20 (36.4) |
| BMI (kg/m2) | 26.52 ± 3.24 |
| Normal (less than 25) | 19 (34.5) |
| Overweight (30 - 25) | 27 (49.1) |
| Obese (more than 30) | 9 (16.4) |
| ASA class | |
| II | 36 (65.5) |
| III | 19 (34.5) |
| EF (%) | 41.63 ± 10.45 |
| ≤ 40 | 27 (49.1) |
| > 40 | 28 (50.9) |
| Blood sugar (mg/dL) | 123.1 ± 29.91 |
| Duration of surgery (min) | 181.09 ± 45.13 |
| Duration of cardiopulmonary pump (min) | 68.69 ± 21.8 |
| Fluid volume received during surgery (mL) | 2268.2 ± 512.2 |
| Urine volume at the end of surgery (mL) | 1292.36 ± 505.8 |
a Values are expressed as No. (%) or mean ± SD.
| Title | Period | P-Value | ||||
|---|---|---|---|---|---|---|
| Before Induction | Before CPB | During Pump | After the End of CPB | After the End of Surgery | ||
| Blood sugar levels (mg/dL) | 124.07 ± 29.46 | 148.12 ± 36.3 | 175.61 ± 55.34 | 184.8 ± 60.69 | 168.07 ± 50.49 | F = 32.76, P = 0.0001 |
In this study, the recorded values did not differ significantly in terms of gender (P = 0.873), age (P = 0.99), BMI (P = 0.177), CPB time (P = 0.706), EF% (P = 0.197), the amount of fluids received during surgery (PP = 0.079), and ASA classes (P = 0.269). Although higher levels were observed in older women, the pump period lasted > 60 minutes. Furthermore, the higher values were noticed in the ASA class III compared to ASA classes II, indicating statistically significant differences at T1 (P = 0.01) and T2 (P = 0.025). Moreover, patients with higher BMI showed higher BG levels, suggesting significant differences at T0 (P = 0.0001), T2 (P = 0.004), and T3 (P = 0.015). Patients with urine < 1000 cc at the end of surgery had significantly higher BG levels at T1 (P = 0.03), T2 (P = 0.006), and T3 (P = 0.01). When they received intravenous fluids > 2000 cc during surgery, it was significant at T2 (P = 0.043) (Table 3).
| Variables | Status | Before Induction (T0) | Before CPB (T1) | During Pump, (T2) | After the End of CPB (T3) | After the End of Surgery (T4) | Intragroup Statistical Estimation | Intergroup Statistical Estimation, |
|---|---|---|---|---|---|---|---|---|
| Gender | Male | t = 1.41, P = 0.164 | t = 0.85, P = 0.397 | t = 0.211, P = 0.834 | t = 0.044, P = 0.965 | t = 0.55, P = 0.581 | P = 0.0001 | F = 0.24, P = 0.873 |
| Female | P = 0.0001 | |||||||
| Age | ≤ 60 | t = 0.786, P = 0.434 | t = 0.43, P = 0.669 | t = 0.58, P = 561 | t = 0.402, P = 0.689 | t = 0.565, P = 0.574 | P = 0.0001 | F = 0.04, P = 0.99 |
| > 60 | P = 0.0001 | |||||||
| BMI | Normal (less than 25) | t = 11.44, P = 0.0001 | t = 3.07, P = 0.054 | t = 6.1, P = 0.004 | t = 4.52, P = 0.015 | t = 2.34, P = 0.106 | P = 0.0001 | F = 1.51, P = 0.177 |
| Overweight (25 - 30) | P = 0.0001 | |||||||
| Obese (more than 30) | P = 0.0001 | |||||||
| ASA class | II | t = 0.88, P = 0.383 | t = 2.59, P = 0.012 | t = 2.31, P = 0.025 | t = 1.09, P = 0.279 | t = 1.2, P = 0.234 | P = 0.0001 | F = 1.32, P = 0.269 |
| III | P = 0.0001 | |||||||
| EF | ≤ 40% | t = 1.51, P = 0.135 | t = 1.74, P = 0.087 | t = 1.27, P = 0.207 | t = 0.382, P = 0.704 | t = 0.547, P = 0.587 | P = 0.0001 | F = 1.57, P = 0.198 |
| > 40% | P = 0.0001 | |||||||
| Duration of surgery | ≤ 180 min | t = 1.39, P = 0.17 | t = 0.44, P = 0.661 | t = 0.971, P = 0.336 | t = 0.006, P = 0.995 | t = 0.195, P = 0.846 | P = 0.0001 | F = 1.24, P = 0.296 |
| > 180 min | P = 0.0001 | |||||||
| Duration of the cardiopulmonary pump | ≤ 60 min | t = 0.071, P = 0.944 | t = 1.15, P = 0.252 | t = 0.759, P = 0.452 | t = 0.352, P = 0.746 | t = 1.01, P = 0.313 | P = 0.0001 | F = 0.471, P = 0.706 |
| > 60 min | P = 0.0001 | |||||||
| Fluid volume received during surgery | ≤ 2000 mL | t = 0.345, P = 0.732 | t = 0.811, P = 0.421 | t = 2.07, P = 0.043 | t = 1.14, P = 0.2560. | T = 0.424, P = 0.673 | P = 0.0001 | F = 2.29, P = 0.079 |
| > 2000 mL | P = 0.0001 | |||||||
| Urine volume at the end of surgery | ≤ 1000 mL | t = 0.907, P = 0.368 | t = 2.17, P = 0.034 | t = 2.87, P = 0.006 | t = 2.58, P = 0.013 | t = 1.88, P = 0.065 | P = 0.0001 | F = 2.83, P = 0.038 |
| > 1000 mL | P = 0.0001 |
Furthermore, ASA class III (P = 0.001), longer duration of CPB (P = 0.021), higher IV fluid volume administrated during surgery (P = 0.023), higher BMI (P = 0.0001), and less urine volume at the end of surgery (P = 0.049) were significantly associated with higher BG values of the coronary sinus. However, there was no statistically significant difference between the mean coronary sinus BG levels with gender (P = 0.453), age (P = 0.516), EF% (P = 0.363), and duration of surgery (P = 0.501) (Table 4).
| Variables | Number | Mean ± SD | P-Value |
|---|---|---|---|
| Gender | 0.453 | ||
| Male | 30 | 215.87 ± 1.28 | |
| Female | 25 | 230.73 ± 68.23 | |
| Age (y) | 0.516 | ||
| ≤ 60 | 33 | 216.69 ± 73.79 | |
| > 60 | 22 | 230.79 ± 4.58 | |
| BMI | 0.0001 | ||
| Normal (less than 25) | 19 | 187 ± 64.73 | |
| Overweight (25 - 30) | 27 | 222.85 ± 62.59 | |
| Obese (more than 30) | 9 | 294.44 ± 88 | |
| ASA class | 0.001 | ||
| II | 36 | 198.69 ± 61.98 | |
| III | 19 | 266.66 ± 84.84 | |
| EF (%) | 0.363 | ||
| ≤ 40 | 27 | 212.79 ± 62.64 | |
| > 40 | 28 | 213.39 ± 72.01 | |
| Duration of surgery | 0.501 | ||
| ≤ 180 min | 32 | 216.73 ± 28.46 | |
| > 180 min | 23 | 230.79 ± 39.71 | |
| Duration of cardiopulmonary pump | 0.021 | ||
| ≤ 60 min | 20 | 191.72 ± 25.09 | |
| > 60 min | 35 | 239.72 ± 85.95 | |
| Fluid volume received during surgery | 0.023 | ||
| ≤ 2000 mL | 28 | 199.74 ± 64.86 | |
| > 2000 mL | 27 | 245.70 ± 55.57 | |
| Urine volume at the end of surgery | 0.049 | ||
| ≤ 1000 mL | 17 | 252.05 ± 81.2 | |
| > 1000 mL | 38 | 208.70 ± 81.19 |
5. Discussion
This study revealed that the current protocols on the BG management in CABG patients provided a proper intra-operative glycemic control. The increasing trend of changes in BG values from T0 to T4, peaked in T3, was statistically significant. This finding supported the finding of a previous study suggesting the association between the severity of stress response during CABG surgery and BG values (12).
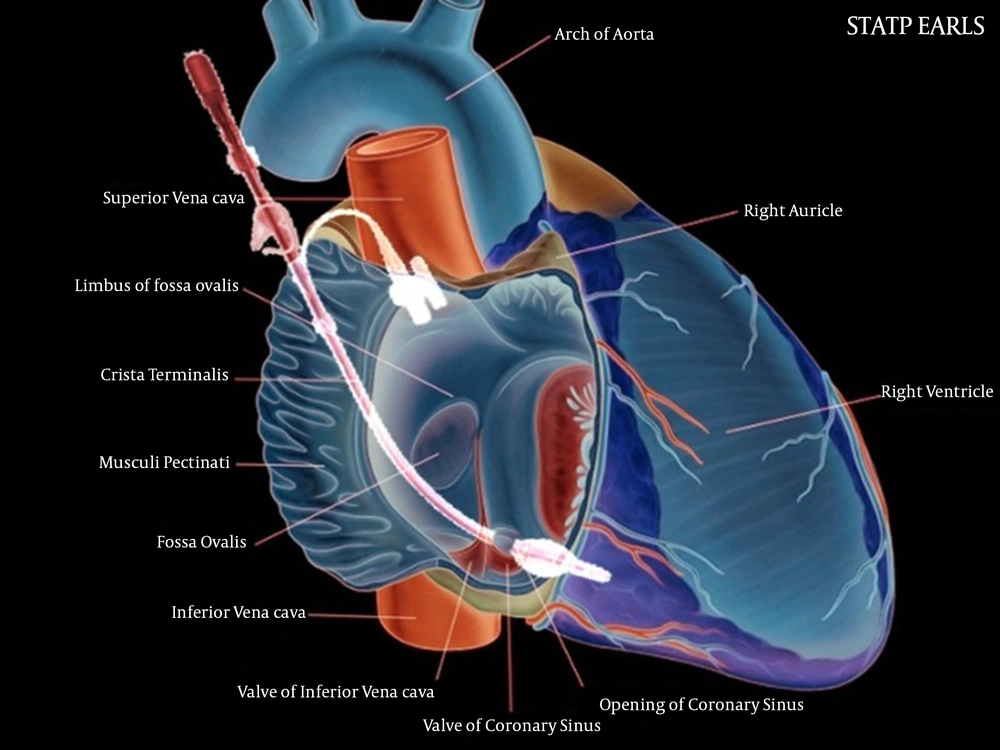
Although the mean BG concentrations were < 200 mg/dL, the mean BG values of the coronary sinus were 222.18 ± 75.74 mg/dL, which was higher than the peripheral sample values at the same measurement time point. The coronary sinus, the largest coronary vein, is formed by converging several vessels. It collects blood from the myocardium and drains deoxygenated blood directly into the right atrium (13, 14). During CABG, the anatomic feature of the coronary sinus plays a critical role as a landmark for the surgeon and an effective place to transmit cardioplegia solution to protect the myocardium (15).
As it was mentioned, the BG levels of the coronary sinus were different from peripheral samples. The exact underlying mechanism of this positive difference has not been well-understood; however, it could be due to hypothermia and cardiologic solutions containing glucose, which led to lower myocardial glucose uptake (Figure 1). Given the specific and critical function of the coronary sinus, directly representing myocardial metabolism, it is theoretically hypothesized that peripheral BG measurement alone could not be a reliable finding. However, the main goal of preoperative glycemic control would be to improve clinical outcomes. Accordingly, further studies are required to achieve practical findings and clarify the effect of coronary sinus BG on short- and long-term outcomes. It is unknown whether the intervention is necessary to correct coronary sinus BG despite proper peripheral glycemic control. A fundamental study showed that coronary sinus BG did not match peripheral sampling; hence, future studies should shed light on several unanswered questions. Previous studies have demonstrated that myocardial glucose increases due to higher coronary sinus blood flow during the increased heart work. Similar studies have indicated that when the human heart is at rest, only 20 - 25% of the myocardial glucose uptake is oxidized (16).
Gertz et al. found that during rest, myocardial energy needs are mainly provided by fat; hence, the BG concentrations increase. In contrast, during the heart’s function, the myocardial section mainly tends to consume glucose (17). Bergman et al. examined the myocardial glucose metabolism by measuring coronary sinus BG during pacing. They found that coronary sinus glucose concentration was significantly lower than arterial samples. Their justification was that during most of the heart’s functions, higher glucose was delivered via high coronary sinus blood flow (18). Sathya et al. detected that moderate glycemic control targeting (150 - 200 mg/dL) led to post-operative mortality and stroke reduction compared to a liberal strategy (> 200 mg/dL). However, there was no definite addition with more intensity (< 150 mg/dL) (19).
According to the existing protocols, the BG levels should be kept < 180 mg/dL, and strict control on BG < 110 mg/dL is no longer recommended (6).
In general, some studies have suggested the increased mortality rate in the CABG patients undergoing strict glycemic control protocols (20). The acceptable results of this study indicate that anesthesiologists in this hospital have a close and continuous communication with the surgeon during the critical surgery stages. A detailed physical examination is performed in preoperative visits, and medical history, including patients' medications and co-morbidities, is obtained.
5.1. Conclusions
These findings indicated that coronary sinus BG was higher than peripheral values. Despite the optimal control of BG based on peripheral sampling, the significance and clinical values of coronary sinus BG should be investigated. Moreover, the existing protocol in the concerned hospital was found to be acceptable. Special attention should be paid to older patients with higher ASA classes.