1. Background
In patients under general anesthesia, laryngeal mask airway (LMA) is a useful substitute for intubation to maintain the airway (1-3). It can be placed without seeing the nasopharyngeal environment and under low pressure around the laryngeal entrance, allowing ventilation with positive pressure (4, 5). This laryngeal mask method was designed by Dr. Brain in 1981 and has been commercially used since 1988 (3-5). The advantages of LMA compared to tracheal intubation are no tracheal injury during tube installation and removal, less airway stimulation, less invasion of the airway tissue, easier installation, and efficient establishment (6-9). Therefore, in adults, it is recommended to use LMA as a substitute for tracheal intubation, especially in patients with a history of intubation, the possibility of difficult intubation diagnosed by an anesthesiologist, and patients whose intubation has failed and ventilation can be performed with a mask (10-12).
Some studies reported hemodynamic alterations and recovery time in the LMA group during general anesthesia were similar to those in the tracheal intubation group (13-15). One of the major problems with plastic and reconstructive surgeries over 2 h is a long-term airway control with a tracheal tube or laryngeal mask, which may cause adverse effects on the airway, including sore throat, ischemia, or damage to the vocal cords, and management decisions can be important and helpful. Therefore, if the patient is nil per os (NPO), the classical LMA can be an appropriate solution (16, 17). Furthermore, in short surgeries, the use of classical LMA with narcotics, midazolam, and propofol without muscle relaxants and with the help of inhaled gasses allows reducing the complications of anesthesia and recovery time at the end of the operation (18, 19).
2. Objectives
We decided to evaluate the effectiveness of classical LMA in comparison with an endotracheal tube (ETT) in plastic and reconstructive surgeries over 2 h on thorax and abdomen under general anesthesia in Hazrat Fatemeh Hospital, Tehran, Iran.
3. Methods
3.1. Study Design
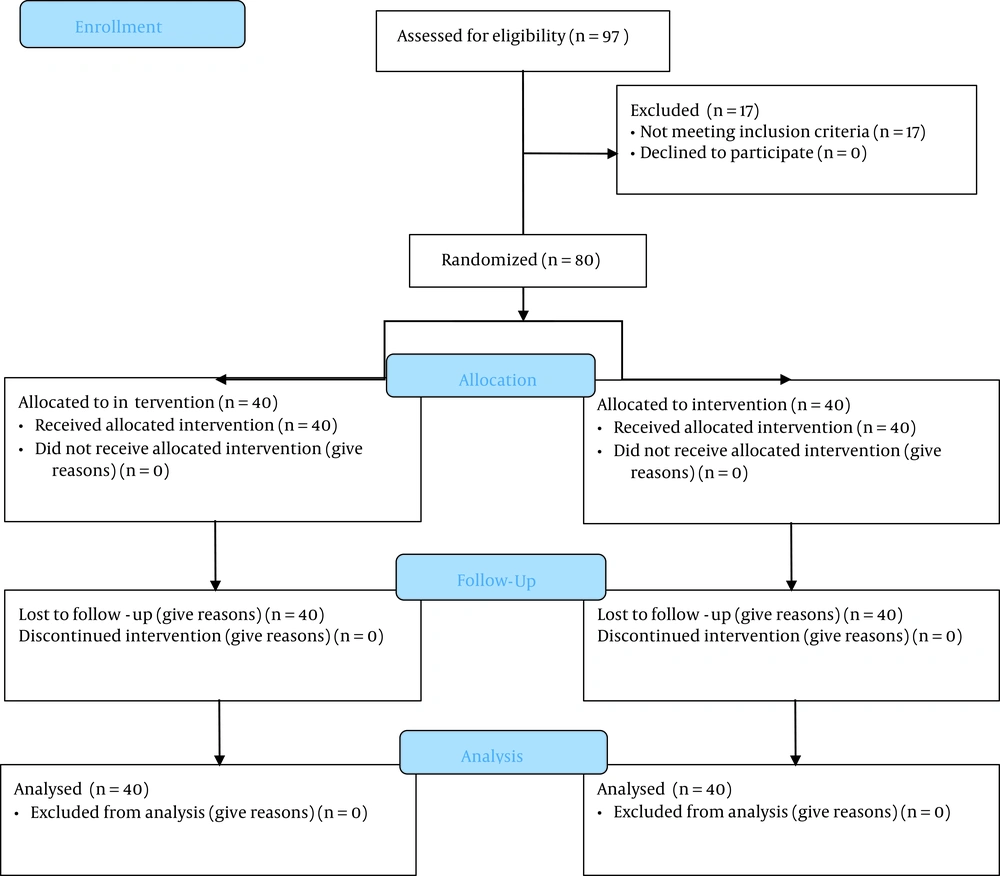
This randomized clinical trial was conducted by a simple randomization method in which a code is given to each patient using a computer-generated random numbers table (MedCalc version 16). Participants were randomly assigned to two groups of LMA and ETT (1:1). This study was performed on 80 patients undergoing thoracic and abdominal surgery under general anesthesia who were referred to Hazrat Fatemeh Hospital affiliated to Iran University of Medical Sciences in Tehran during March 2020-September 2020 (Figure 1). The sample size was calculated to be 40 for each group using a web-based formula considering α = 0.05, 1-β = 0.9, and effect size = 0.71 (12). The inclusion criteria were ASA 1 or 2 based on the physical status classification system and being in the age range of 25 - 60 years. The exclusion criteria entailed being non-NPO, body mass index (BMI) above 35, Latex sensitivity, and history of colds in the last 10 days. By random selection, the participants were assigned to two treatment groups, namely laryngeal mask and endotracheal tube. All patients received the same medication for general anesthesia.
3.2. General Anesthesia
General anesthesia was the same in both groups. For premedication, 0.2 mg/kg of midazolam plus 3 μg/kg fentanil was used. For induction, 2.5 mg/kg of propofol and 0.5 mg/kg of atracurium were administered intravenously. In addition, 10 μg/kg/min atracurium and 1 μg/kg/min remifentanil were used for the maintenance of GA. After completing the surgery, 0.04 mg/kg neostigmine plus 0.02 mg/kg atropine was applied to reverse the effects of anesthesia. Both groups were studied for variables, such as age, gender, Mallampati score, and BMI. The main variables included the ease of placement, EtCO2, arterial oxygen saturation, and laryngeal and tracheal spasm. The sub-variables encompassed the mean duration of anesthesia, nausea and vomiting, sore throat, and abdominal distension.
3.3. Procedures
In the first group of LMA, the appropriate size is 3, 4, or 5 according to the recommendation of the manufacturer with standard placement (manufactured by IranFormis). In the second group, ETTs were 7 or 7.5 for female patients and 7.5 or 8 for male patients (manufactured by TebTolid). Intracuff pressure of LMA and ETT cuff pressure was 60 cm H2O and 25 cm H2O, respectively. Mechanical ventilation was at a tidal volume of 8 ml/kg and adjusted respiratory rate to maintain an EtCO2 concentration of 35 - 45 mmHg.
3.4. Ethical Considerations
The protocol of this research was approved by the Ethics Committee of Iran University of Medical Sciences (IR.IUMS.FMD.REC.1398.539) and the Iranian Registry of Clinical Trials (IRCT20110513006465N2). Moreover, informed consent was taken from all participants.
3.5. Statistical Analysis
The obtained data were analyzed by the SPSS statistical software version 25. Quantitative findings were reported as mean and standard deviation, and qualitative findings as frequency. Furthermore, independent t-test, Mann-Whitney, chi-square, and Fisher’s exact test were used in the study. P-value < 0.05 was considered statistically significant.
4. Results
Overall, 80 patients were compared into two groups, and 76 participants were female. The age of the LMA group and EET Group was 36.33 ± 12.82 and 34.58 ± 5.92 years, respectively. A comparison of the characteristics of participants in the two groups is shown in Table 1. The results of the chi-square test demonstrated no statistically significant difference between spasms in the cases in the two groups at the 95% confidence level. Our findings revealed that 4 out of 40 LMA patients (10%) and nine subjects in the ETT group (22.5%) had postoperative nausea and vomiting. Moreover, the chi-square test indicated that vomiting and nausea were not significantly different between the two groups in the 95% confidence level. According to the chi-square test, there was no statistically significant difference between the sore throat of patients in the two groups at the 95% confidence level. We observed that five subjects in the LMA group (12.5%) and 12 patients in the ETT group (30%) had a postoperative sore throat. Moreover, the chi-square test showed no statistically significant difference between the abdominal distension of patients in the two groups in the 95% confidence level.
| Variables | Intervention | Total | P-Value | |
|---|---|---|---|---|
| LMA | ETT | |||
| Gender | 0.041 | |||
| Female | 36 (90) | 40 (100) | 76 (95) | |
| Male | 4 (10) | 0 (40) | 4 (5) | |
| Spasm | 1 | |||
| Yes | 2 (5) | 1 (2.5) | 3 (3.8) | |
| No | 38 (95) | 39 (97.5) | 77 (96.3) | |
| Nausea and vomiting | 0.13 | |||
| Yes | 4 (10) | 9 (22.5) | 13 (16.3) | |
| No | 36 (90) | 31 (77.5) | 67 (83.8) | |
| Sore throat | 0.056 | |||
| Yes | 5 (12.5) | 12 (30) | 17 (21.3) | |
| No | 35 (87.5) | 28 (70) | 63 (78.8) | |
| Abdominal distension | 0.288 | |||
| Yes | 6 (15) | 3 (7.5) | 9 (11.3) | |
| No | 34 (85) | 37 (92.5) | 71 (88.8) | |
a Values are expressed as No. (%).
The t-test showed that the mean age difference between the two groups was not statistically significant at a 95% confidence level. The results of the independent samples t-test revealed that the mean arterial oxygen saturation was not significantly different between the two groups at the 95% confidence level. We found that the mean BMI of patients did not have a significant difference between the two groups at a 95% confidence level. Descriptive statistics and the comparison of age, O2 saturation, and BMI between the two groups are presented in Table 2.
| Variables | No. | Mean ± SD | P-Value |
|---|---|---|---|
| Age | 0.436 | ||
| LMA | 40 | 36.33 ± 12.823 | |
| ETT | 40 | 34.58 ± 5.926 | |
| O2 saturation | 0.358 | ||
| LMA | 40 | 99.875 ± 0.4634 | |
| ETT | 40 | 99.95 ± 0.22072 | |
| BMI | 0.102 | ||
| LMA | 40 | 28.48 ± 41.51 | |
| ETT | 40 | 30 ± 4.101 |
Comparison of lung ventilation with the recurrent amount of carbon dioxide index and the duration of anesthesia between the two groups is summarized in Table 3. The results of the Mann-Whitney test showed that the difference between the mean amount of recurrent carbon dioxide of patients in the two groups was not statistically significant at a 95% confidence level. This test revealed that the mean duration of anesthesia was not significantly different between the two groups at a 95% confidence level.
| Variables | No. | Mean | Median | Quartile (1,3) | P-Value |
|---|---|---|---|---|---|
| The amount of recycled carbon dioxide | 0.166 | ||||
| LMA | 40 | 35.43 | 35.5 | 36.7, 34 | |
| ETT | 40 | 34.98 | 34 | 36, 34 | |
| Duration of anesthesia (min) | 0.143 | ||||
| LMA | 40 | 346.88 | 330 | 420, 300 | |
| ETT | 40 | 372.25 | 372 | 420, 334 |
5. Discussion
According to the results of the current study, there is a statistically significant difference between the gender distribution of patients in two groups at a 95% confidence level as the number of females in the ETT group was higher than in the LMA group. Furthermore, the difference between the mean anesthesia duration of the two groups was not significant. However, mean age, BMI, mean Mallampati score, mean carbon dioxide amount, nausea and vomiting, sore throat, abdominal pain, spasm, and arterial oxygen saturation were not significantly different between the two study groups.
Suppiah et al. demonstrated that respiratory complications and hemodynamic changes after extubation were more common in adult patients undergoing endotracheal intubation than in patients who were replaced with LMA at the end of tracheal surgery (5). Akhondi et al. showed that the LMA, as a suitable option in adults, can significantly reduce cough and airway complications following general anesthesia (7).
Our results revealed no significant difference in the Mallampati score of the two research groups. According to an investigation by Bhagwat Lawate et al., ProSealTM laryngeal mask airway (PLMA) can also be an effective airway device in laparoscopic oxygenation and appropriate ventilation surgeries (11). The PLMA is also associated with minimal complications during and after surgery, and pulmonary ventilation is effective despite high airway pressures without gastric distention, aspiration, and relapse (13-15). According to Dumas et al., using LMA to control the airways in patients under general anesthesia for dacryocystorhinostomy surgery was safe and effective, and no aspiration occurred during the application of LMA (13).
Furthermore, in the current study, no significant difference was observed between the two groups of patients in terms of nausea and vomiting. Griffiths et al. indicated that Procyl laryngeal mask, in contrast to the endotracheal tube, does not reduce postoperative pain, nausea, and vomiting. The latter findings were consistent with our results (14). The limitation of our study was that the amount of airway bleeding due to laryngospasm and bronchospasm was not measurable.
5.1. Conclusions
According to the results of this study, LMA is not significantly different from the endotracheal tube in airway management of some specific procedures. It seems that LMA for anesthesia in surgeries over 2 h can be considered an alternative to the endotracheal tube. Further studies are required to determine efficacy of LMA in other types of prolonged surgeries.