1. Background
Laryngeal and hypopharynx lesions are common head, neck, and upper airway diseases. In examining these lesions with direct laryngoscopy, in addition to sufficient information on the type, location, and extent of the lesion, there is also lesion sampling and surgical interventions. In various studies, ultrasound is widely used to determine the location of peripheral nerve blocks (1). Laryngeal and hypopharynx lesions are common head and neck diseases in between 85% and 95% of cases of squamous cell carcinoma. One of the main and low-risk methods of examining them is direct laryngoscopy, which, with few complications, can provide important information about these lesions, including the type of complication, location, lesion spread, and macroscopic appearance, as well as the possibility of sampling (2, 3). Since most patients with tumors and supraglottic lesions are in high-age groups and have risk factors for systemic diseases, it is advisable to use less risky anesthesia techniques for diagnostic and therapeutic methods (3, 4). On the other hand, obstructive masses of the supraglottis limit laryngoscopy and intubation, and the risk of airway complications is very high for patients. Most of these problems lead to safer methods, especially regional anesthesia techniques, to select appropriate conditions for diagnostic and therapeutic methods to treat patients in a waking state by maintaining spontaneous breathing and appropriate anesthesia without creating additional risk (5, 6). A bilateral superior laryngeal nerve block (SLNB) can provide complete anesthesia for laryngeal sampling; even a complete and bilateral block of this nerve does not block swallowing, and the movements of the vocal cords remain untouched. This block begins on average 3 minutes after the injection of anesthetic lidocaine, and recovery takes about an hour and a half (7, 8). This procedure is done in minutes and with the possibility of difficult airway management. Accordingly, due to its importance and the lack of similar studies in this field, this study was performed to reduce the risk of general anesthesia and improve patients’ recovery.
2. Methods
This single-blind clinical trial study was performed in the Ear, Nose, and Throat (ENT) Ward of Rasoul Akram Hospital, Iran University of Medical Sciences. Fifty patients aged 18 - 70 years were included in this study who underwent a biopsy of supraglottic masses with direct laryngoscopy in the ENT operating room of Rasoul Hospital in 2019 - 2020. Considering the 15% exclusion from the study, the sample size estimation was based on the study of Ambi et al. (9) with a study power of 99% and according to the following formula:
Patients were randomly divided into 2 groups of 25 by computer with the block randomization method. After providing sufficient information on how to perform the block in this study, written consent was obtained from patients. Patients who did not agree with the procedure and patients with coagulation disorders and lidocaine sensitivity and addiction to any drugs were excluded from the study.
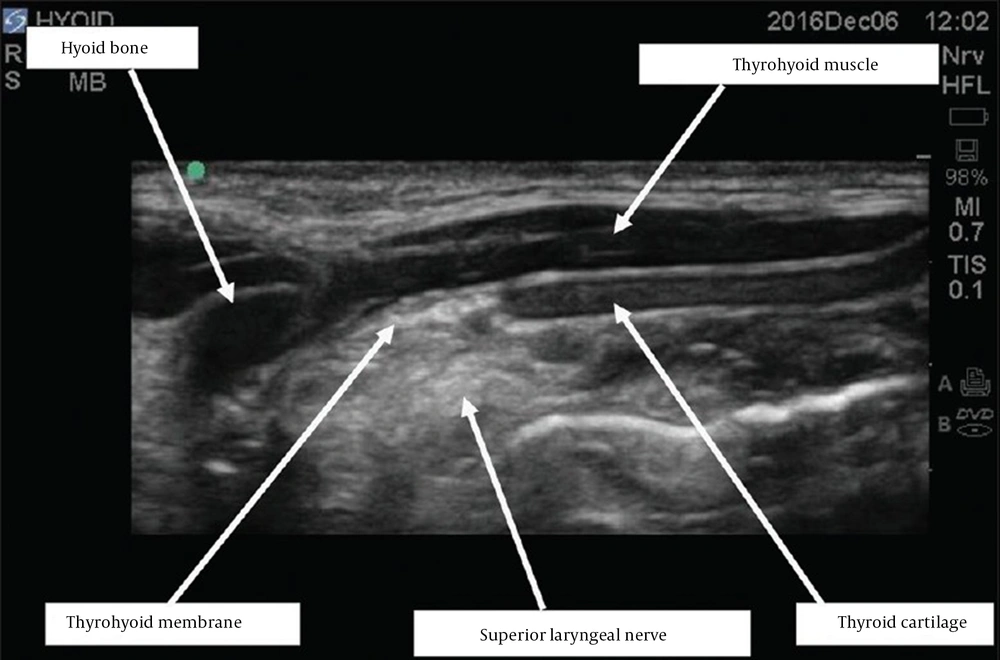
After fixing an IV line and 3 mL/kg normal saline solution, both groups received non-invasive monitoring of blood pressure, heart rate (HR), and 1 - 3 L of oxygen per minute from the nasal cannula and 2-µ/kg fentanyl and then 3 - 4 puffs of lidocaine 10% spray in the mouth. Patients’ neck prep and drop were performed. In the anatomical landmark technique group (C group) patients, in the supine position (their head slightly backward), the large horn of hyoid bone (LHH) and thyroid cartilage were diagnosed. With the 23-gauge needle, 2 mL of 2% lidocaine was slowly injected into the great horn of the hyoid bone (after aspiration to avoid intravenous injection), which was exactly done for the other side. In the sono-guided SLNB group (U group), using a Sonosite MicroMaxx portable ultrasound device and linear 6-13MH2 ultrasound transducer, the probe was placed in the submandibular area (with the parasagittal orientation). The great horn of the hyoid bone was diagnosed from thyroid cartilage, and it was seen as a hyperechoic structure. The thyrohyoid membrane was located between these 2 structures. The SLN space was limited by the hyoid bone at the top, the thyroid cartilage at the bottom and front, and the epiglottic thyrohyoid membrane at the back (Figure 1). Between the GHH bone and thyroid cartilage (above the hyoid cartilage), 2 mL of 2% lidocaine was injected with a 23 gauge eco-visible needle (after aspiration to avoid intravenous injection). Before the block and at the beginning of laryngoscopy and then after the block, after the biopsy, and in the recovery room, mean arterial pressure (MAP), HR, and oxygen saturation were checked and recorded. At the end of the surgery, surgeon satisfaction was recorded by the Numerical Rating Scale (NRS; 0 for very bad surgical condition and 10 for the best surgical condition). Also, the patients’ pain was recorded after surgery and in the recovery room by NRS. To evaluate the quality of the technique, a 5-point scale method was used, scoring from 0 to 4 from no symptoms to very acute symptoms (0, no gagging or coughing in the direct laryngoscopy; 1, mild gagging or coughing that does not inhibit direct laryngoscopy; 2, moderate gagging or coughing that opposite slightly; 3, severe gagging or coughing that made direct laryngoscopy difficult; 4, very severe gagging or coughing that needs extra local anesthetic or change in technique to reach successful direct laryngoscopy). The surgeon and anesthesiologist performing the block were the same in both groups.
Data were analyzed using SPSS version 23 (SPSS Inc., Chicago, Ill, USA). The results of the analysis were reported as a percentage of frequency (for qualitative variables) and mean and SD (for quantitative variables). A Mann-Whitney U test, analysis of variance (ANOVA), independent sample t test, and Fisher exact test were used to examine the relationships between qualitative and quantitative variables. The confidence level was 95%, and P values less than 0.05 were considered statistically significant. The Ethics Committee of Iran University of Medical Sciences approved this study (code: IR.IUMS.REC.1398.490). Also, this research was registered on the Iranian Registry of Clinical Trials website (code: IRCT20191003044963N1).
3. Results
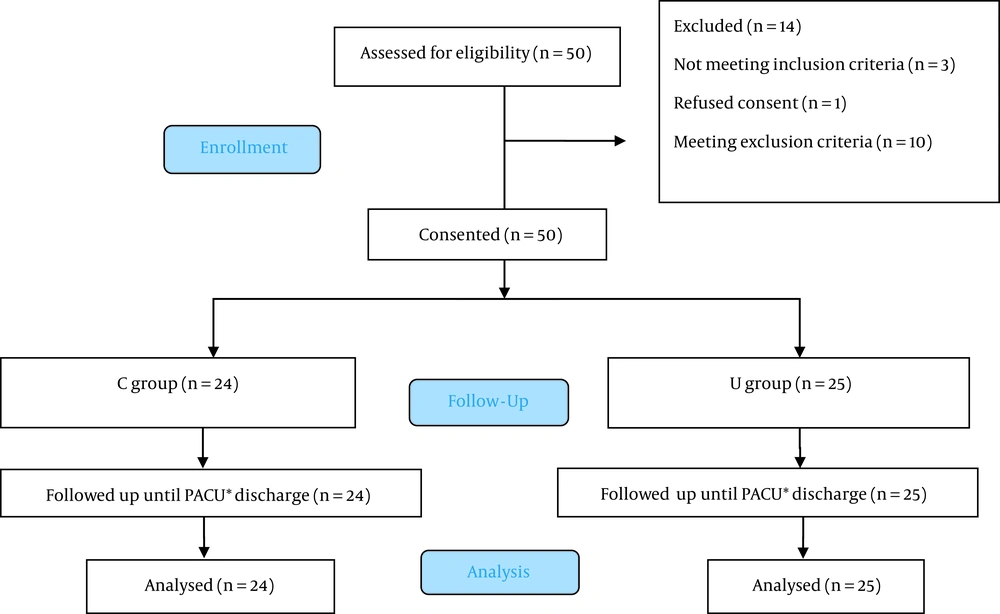
Table 1 compares the demographic characteristics of the 2 groups. As shown in the table, the mean age of patients was 45 ± 13.5 years in the control group and 46 ± 14 years in the case group, but no significant difference was observed between the 2 groups (P = 0.445). Also, in the C group, there were 21 males (84%) and 4 females (16%), and in the U group, there were 25 males (100%) and no female (0.00%), but no significant difference was observed between the 2 groups (P = 0.110). The mean neck circumference of patients was 40.8 ± 5.5 cm in the C group and 40.4 ± 4.03 cm in the U group, which was not significantly different between the 2 groups (P = 0.748). The weight of patients was 70.6 ± 14.05 kg in the C group and 71.3 ± 10.42 kg in the U group, which was not significantly different between the 2 groups (P = 0.847). In addition, the Mallampati score was 2 (2 - 3) in the C group and 3 (3 - 2) in the U group, which was not significantly different between the 2 groups (P = 0.288). As this table shows, no significant differences were observed in demographic variables, but they may potentially play the role of confounding variables. Therefore, it can be claimed that none of the contextual and demographic variables are confounding. The CONSORT (Consolidated Standards of Reporting Trials) diagram is shown in Figure 2.
| Variables | C Group (n = 25) | U Group (n = 25) | P Value |
|---|---|---|---|
| Age (y) | 45 ± 13.5 | 46 ± 14 | 0.445 |
| Gender | |||
| Female | 4 (16) | 0 (0) | 0.110 |
| Male | 21 (84) | 25 (100) | |
| Neck circumference (cm) | 40.8 ± 5.5 | 40.4 ± 4.03 | 0.748 |
| Weight (kg) | 70.6 ± 14.05 | 71.3 ± 10.42 | 0.847 |
| Height | 169 ± 20.4 | 172 ± 23.1 | 0.625 |
| Mallampati score; median (quartile 1 - quartile 3) | 2 (2 - 3) | 3 (2 - 3) | 0.288 |
a Values are expressed as No. (%) or mean ± SD unless otherwise indicated.
Table 2 compares the success of the procedure, the surgeon’s satisfaction with the procedure, and the pain during the procedure. As shown in the table, the success of the procedure was 24 (96%) in the C group (only in 1 case, general anesthesia was performed to continue the biopsy) and 25 (100.00%) in the U group, which was not significantly different between the 2 groups (P = 0.99). The average satisfaction of the surgeon with the procedure was 10 in the C group (9.25 - 10) and 10 in the U group (9 - 10), which was not significantly different between the 2 groups (P = 0.337). In addition, based on the results, the mean score of pain during biopsy was 3 (2 - 5) in the C group and 2 in the U group (1.5 - 3), which was not significantly different between the 2 groups (P = 0.148). The amount of pain in the recovery room was 0 (0 - 2) in the C group and 0 (0 - 1) in the U group, which was not significantly different between the 2 groups (P = 0.614). In addition, the quality of the technique on a 5-point scale was 1 (0 - 1) in the C group and 1 (1 - 0) in the U group, which was not significantly different between the 2 groups (P = 0.956).
| Variables | C Group (n = 25) | U Group (n = 25) | P Value |
|---|---|---|---|
| Successful | 24 (96) | 25 (100) | 0.99 |
| Unsuccessful | 1 (4) | 0 (0) | |
| Surgeon satisfaction | 10 (9.25 - 10) | 10 (9 - 10) | 0.337 |
| NRS during the biopsy | 3 (2 - 5) | 2 (1 - 3.5) | 0.148 |
| NRS in the recovery room | 0 (0 - 2) | 0 (0 - 1) | 0.614 |
| Technique quality | 1 (0 - 1) | 1 (0 - 1) | 0.956 |
Abbreviation: NRS, Numerical Rating Scale.
For analysis of MAP, HR, and oxygen saturation percentage and their changes during procedure we used the repeated measure ANOVA statistical test. As shown in Table 3, there was no significant difference between the 2 groups.
| Variables | C Group (n = 24) | U Group (n = 25) | P Value |
|---|---|---|---|
| Comparison of MAP and its changes | |||
| MAP before the block (1) | 114.4 ± 19.75 | 110.6 ± 18.74 | 0.493 |
| MAP after the block (2) | 109.4 ± 24.16 | 112.6 ± 21.26 | 0.626 |
| MAP after the biopsy (3) | 123 ± 24.26 | 113.9 ± 26.06 | 0.208 |
| MAP in the recovery room (4) | 115.8 ± 16.98 | 119.4 ± 21.26 | 0.514 |
| Mean HR and its changes | |||
| HR before the block (1) | 90.5 ± 20 | 82.7 ± 15.85 | 0.131 |
| HR after the block (2) | 88.9 ± 20.29 | 81.3 ± 15.18 | 0.14 |
| HR after the biopsy (3) | 95.4 ± 15.71 | 81.7 ± 14.59 | 0.002 |
| HR in the recovery room (4) | 96.2 ± 17.87 | 84.4 ± 12.81 | 0.01 |
| The average percentage of oxygen saturation and its changes | |||
| SO2 before the block (1) | 97.6 ± 2.45 | 97.8 ± 2.58 | 0.737 |
| SO2 after the block (2) | 97.3 ± 2.13 | 98 ± 1.37 | 0.14 |
| SO2 after the biopsy (3) | 97.2 ± 2.6 | 98.2 ± 1.47 | 0.101 |
| SO2 in the recovery room (4) | 97.9 ± 2.01 | 98.3 ± 1.6 | 0.396 |
Abbreviations: MAP, mean arterial pressure; HR, heart rate.
4. Discussion
In Iran, the present study is the first to compare SLNB with 2 methods of landmark anatomical and ultrasound guide. In this study, patients were evaluated for age, sex, weight, neck circumference, and Mallampati score. The procedure’s success rate was 24 in the anatomical landmark group and 25 in the group with the ultrasound guide. There was also no difference in the surgeon’s satisfaction with the procedure. MAP and its changes and the mean of oxygen saturation and its changes before the block, after the block, after the biopsy, and in the recovery room were not significantly different between the 2 groups. In addition, mean HR and its changes over time were compared in the study groups. Mean HR before and after the block was not significantly different between the 2 groups. However, in the recovery room and after the biopsy, HR was higher in the C group than in the U group; this difference was significant.
In the study by Mathur et al. (10), to compare lignocaine nebulization and airway nerve block with the help of optical fiber in awake intubation through the nose by bronchoscopy, the introduction of ultrasound and the prevalence of its use as a tool (which provides a proper, sufficient, and instantaneous view of the internal structures of the body) and, at the same time, non-use of ionizing waves in it led to the use of this technique in recent years to perform peripheral nerve block. However, the important point is that ultrasound can not necessarily help improve the quality of the block and its results. For example, when there is not enough vision of the neural structures and important elements around them, or when the ultrasound is performed by an inexperienced person, consequently, it may not be a very useful technique. The main results of their study are consistent with our results.
In various studies, ultrasound has been widely used to determine the location of nerves in various nerve blocks. Potential benefits of using ultrasound imaging for nerve blocks include reducing the amount of local anesthesia, improving success rates, reducing block time, and reducing complications. In studies that have been conducted to compare the 2 methods of ultrasound and landmark anatomical, no diagnosis was made, and most of them have difficulties in fiber optic intubation in patients with airway problems (11, 12). To investigate the ultrasound and anatomical landmark-guided technique for SLNB to assist the process of awake intubation with the help of fiber optics, Ambi et al. (9) conducted a study on 40 patients with ASA I-II anesthesia aged 18 - 60 years with difficulty in predicting intubation in 2 groups. Group L received landmark-guided bilateral SLNB with 1 mL of 2% lidocaine, and group U received bilateral SLNB with 1 mL of 2% lidocaine using an ultrasound transducer to describe the superior laryngeal nerve space. They found that ultrasound for SLNB as a portion of the preparation in awake fiber-optic intubation increased the value of patient acceptance. The results of their study are not consistent with our results.
In China, Zhipeng et al. showed that Ultrasound guided SLNB might successfully decrease the postoperative sore throat after extubation under general anesthesia (13). It is noteworthy that in the present study, the reason for higher HR after the biopsy and in the recovery room in the anatomical landmark group could indicate a better block with ultrasound, but they observed sore throat after general anesthesia, and we evaluated direct laryngoscopy of the supraglottic mass.
Most of the studies that have compared the 2 methods of ultrasound guide and anatomical landmark have pointed out that the method of using ultrasound guide is superior to the anatomical landmark method in patients who have a short and thick neck or in cases of cervical pathologies (6, 9, 14).
We had some limitations in the present study. For instance, we did not calculate the body mass index of patients. Further studies are needed with patients with different neck circumferences, different body mass indices, no good landmarks, and higher sample sizes.
4.1. Conclusions
SLNB for direct laryngoscopic surgery for biopsy of supraglottic masses using ultrasound was not significantly superior to the traditional method. In addition, there was no significant difference between the 2 methods in terms of procedure success, surgeon satisfaction, and patient pain.