1. Background
Effective mask ventilation is vital during general anesthesia; however, upper airway obstruction is a cause of difficult mask ventilation and a common clinical problem after anesthesia induction, especially in children (1-3). The overall incidence of difficult mask ventilation is 1.4% during general anesthesia in adults and 0.15% in cases of mask ventilation (4). However, the rate of difficult mask ventilation in children is 6.6%, even in populations where difficult ventilation is expected with a mask (2). Children have relatively larger heads, tongues, and adenoids, and adenotonsillar hypertrophy is more common in preschool and older children, which is a common cause of ear, nose, and throat elective surgery and is the narrowest part of the airway at the level of the tonsils. These anatomical features may make airway obstruction more likely in children during anesthesia (5, 6).
In one study, the incidence of difficult ventilation with a mask was 5%, which was significantly associated with intubation. In this study, factors such as having a beard, obesity (BMI above 26), no teeth or lack of teeth, age over 55 years, and a history of snoring and difficult ventilation were effective and predictive factors of difficult ventilation (4). Meanwhile, when anesthesiologists use masks, one of the common problems is the possibility of damage to the eyes and nerves of the face, especially in people hospitalized with trauma to the face and eyes. In these people, it is impossible to press the mask firmly and create a proper seal; hence the proper ventilation is not done (7). Radiological studies have shown that neck extension is the most effective maneuver to keep the throat open. Applying force from behind the temporomandibular joint to the front can also be helpful. If these two maneuvers are not successful, tools such as oropharyngeal airway and nasopharyngeal airway should be used (8-10).
Face mask ventilation is a fundamental skill that requires technical and accurate comment. Using a face mask (on the nose and mouth simultaneously) with spontaneous breathing throughout the induction and maintenance of anesthesia with inhalants is the simplest and least invasive method of anesthesia for short surgery. It is appropriate for all patients except those who vomit and return food. Face masks are also used for controlled ventilation before and after the endotracheal tube. Face masks are designed to cover the patient's mouth and nose. There are two main points in using a mask: The complete sealing between the face and the mask and the absence of gas leakage, and the openness of the patient's airways, which should always be checked. The quality of the seal in spontaneous ventilation is determined by the filling and movements of the mask storage bag. Gas leakage usually occurs around the nose and cheeks. On the other hand, the symptoms of airway obstruction depend on the location and extent of the obstruction and whether positive pressure or spontaneous breathing method is used. The most critical sign of clinical airway obstruction is vocal breathing (snoring occurs in supraglottic obstruction and tail stridor occurs in gluteal obstruction), which is a classical sign of airway obstruction in spontaneous breathing (8).
A study of 17 patients over 18 years of age under general anesthesia showed that nasal ventilation was more effective than general ventilation in adults who expelled more respiratory carbon dioxide from the lungs (11). In another study performed on 73 patients with a mean age of 48 years (18 - 65 years) under general anesthesia, more current volume was provided for patients under ventilation with nasal anatomical masks than those with anatomical facial masks. Therefore, nasal mask ventilation was more efficient than face mask ventilation. Nasal mask ventilation during anesthesia also provides more efficiency and safety than anatomical mask ventilation in the natural position of the neck (12).
2. Objectives
Since gas leakage may occur around the nose and cheeks in anatomical face mask ventilation while it is not possible to press the mask firmly and create a proper seal, especially in people hospitalized with trauma to the face and eyes, and airway obstruction is more likely in children due to their anatomical condition, it is assumed that there will be fewer problems in nasal mask ventilation. In addition, since the positive pressure is not applied to the soft tissue of the tongue and mouth in nasal mask ventilation, the entire volume of the tail enters the larynx and airway through a relatively hard-nosed route. Also, the pressure gradient between the nasopharynx and oropharynx moves the tongue and palate forward, resulting in less airway obstruction during ventilation that is more pronounced in patients with ventilation. Therefore, the present study compared nasal mask ventilation with anatomical face mask ventilation in the age group of 3 to 12 years.
3. Methods
This study is a single-blind randomized clinical trial. The study population included all patients aged 3 to 12 years who were candidates for elective lower abdominal surgery under general anesthesia in Al-Zahra Hospital from January 2020 to May 2021.
The sample was calculated as 35 patients in each group with a confidence level of 95%, 80% test power, and the standard deviation of 4.5 and 0.2, based on the previous studies (11) on the difference in mean volume of carbon dioxide per breath equal to 5.
The inclusion criteria included all patients candidates for elective lower abdominal surgery with general anesthesia, age of 3 - 12 years, no obstruction in the nasal passage, no airway obstruction (such as hypertrophy of the adenoids, tonsils, and tongue), any obvious deformity or fracture of the face, and no acute or chronic lung disease. The exclusion criteria included changing the anesthesia plan from general to regional. In case ventilation was impossible, we used an oropharyngeal airway and an anatomical face mask with neck extension.
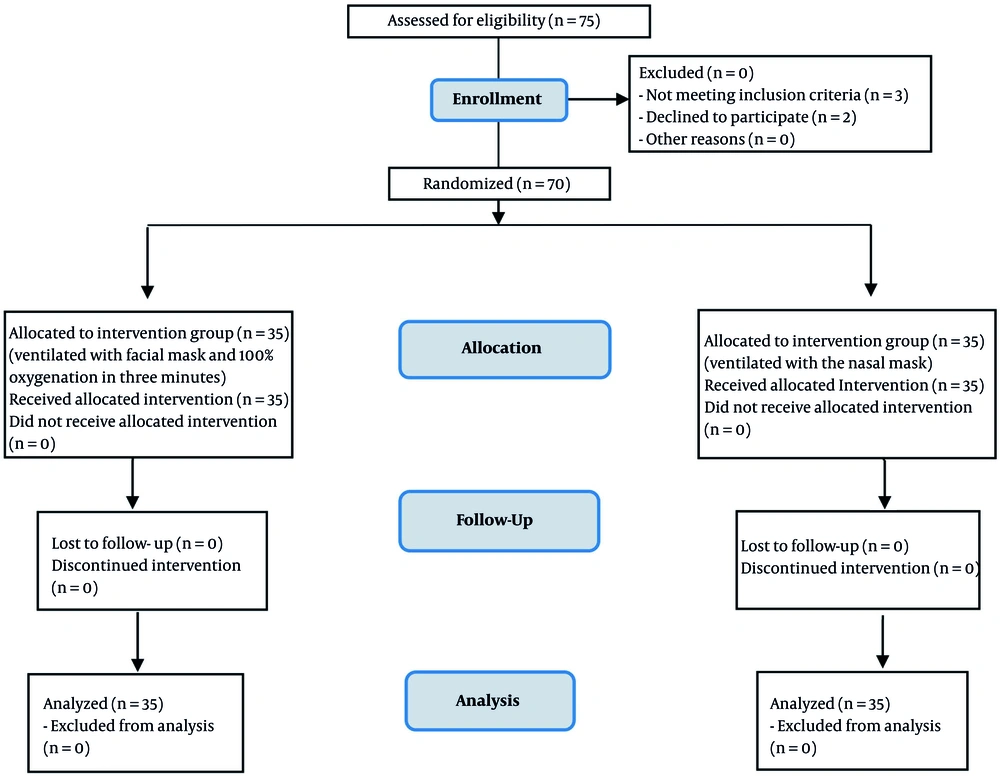
After obtaining the code of ethics from the Medical Ethics Committee of Isfahan University of Medical Sciences (approved code: IR.MUI.REC.1395.3.424), clinical trial code (NCT05018468), and consent of patients' parents, inclusion criteria for all patients were evaluated by an anesthesiologist and the necessary explanations were given to the patients' supervisors. They were given necessary instructions before the operation, and fluid therapy was supplied during fasting and premedication. On the day of surgery, after premedication with midazolam (0.05 mg kg-1) and ketamine (0.5 mg kg-1) and placement on the operating room bed, patients underwent pre-oxygenation with a mask near the face of O2 100% for three minutes. Then, anesthesia induction drugs, including thiopental sodium 5 mg kg-1, atracurium 0.5 mg kg-1, and fentanyl 2 µg kg-1 were given to all patients. At this time, the patients were randomly divided into two groups of 35 (Figure 1).
The first group was ventilated with an anatomical face mask and 100% oxygen for three minutes. In the second group, ventilation was performed through a nasal mask and 100% oxygen for three minutes. In both groups, ventilation was performed with the help of the anesthesia machine control mode with a volume of 8 cc kg-1 and a speed of 12 - 20 breath/ min-1. The mean expiratory flow volume, mean volumes of SpO2 and EtCO2, and mean volume of maximum airway pressure in three consecutive breaths in the second minute after ventilation initiation were measured in both groups (13). After endotracheal intubation and fixation of the tube and its connection to the anesthesia machine, these parameters were measured again in the fifth minute after endotracheal intubation. Hemodynamic changes, including heart rate and systolic and diastolic blood pressure, were also recorded and compared between both groups.
Finally, the collected data were entered into SPSS software (ver. 25). Data were presented as means ± standard deviation (SD) or n (%). As the Kolmogorov-Smirnov test showed that data distribution was normal, an independent t-test was used to compare the mean of quantitative variables between the two groups. Fisher's exact test was used to compare qualitative variables between the two groups. The significance level in all analyses was considered less than 0.05.
4. Results
There were 32 (91.4%) boys and three (8.6%) girls with a mean age of 4.5 ± 2.2 years and a mean weight of 15.2 ± 5.3 kg in the nasal mask group and 32 (91.4%) boys and three (8.6%) girls with a mean age of 4.3 ± 1.9 years and a mean weight of 14.5 ± 4.4 kg (P value > 0.05) in the face mask group.
The mean expiratory tidal volume and maximal airway pressure in three consecutive breaths were not significantly different between the two groups at any time (P value > 0.05). The mean EtCO2 in the second minute after the start of ventilation was significantly higher in the nasal mask group than in the face mask group (P value = 0.04), but there was no significant difference between the two groups in the fifth minute after endotracheal intubation (P value = 0.31) (Table 1).
| Variables | Time | Face Mask Group | Nasal Mask Group | P-Value |
|---|---|---|---|---|
| Expiratory flow volume (mL) | Second minute after the start of ventilation | 117.7 ± 28.6 | 123.9 ± 32.3 | 0.403 |
| Fifth minute after endotracheal intubation | 139.4 ± 41.7 | 135.8 ± 34.1 | 0.701 | |
| Maximum airway pressure (CmH2O) | Second minute after the start of ventilation | 12.5 ± 1.9 | 13.02 ± 2.1 | 0.228 |
| Fifth minute after endotracheal intubation | 15.4 ± 2.04 | 16.2 ± 2.2 | 0.123 | |
| EtCO2 (mmHg) | Second minute after the start of ventilation | 29.5 ± 4 | 31.4 ± 3.5 | 0.041 |
| Fifth minute after endotracheal intubation | 37.2 ± 2.8 | 38.2 ± 4.9 | 0.312 |
Comparison of Parameters Related to Quality of Ventilation Between Two Groups a
The mean SPO2 and heart rate were not significantly different between the two groups in any of the three times (P value > 0.05). Mean systolic blood pressure, diastolic blood pressure, and mean arterial blood pressure (MAP) at baseline were not significantly different between the two groups (P value > 0.05) but were significantly lower in the nasal mask group than in the face mask group at the subsequent times (P value < 0.05) (Table 2).
| Variables | Time | Face Mask Group | Nasal Mask Group | P-Value |
|---|---|---|---|---|
| SPO2 (%) | Baseline | 94.7 ± 2.4 | 95.3 ± 2.4 | 0.301 |
| Second minute after the start of ventilation | 97.7 ± 1.8 | 97.2 ± 3.1 | 0.368 | |
| Fifth minute after endotracheal intubation | 98.3 ± 1.7 | 98.2 ± 1.9 | 0.692 | |
| Systolic blood pressure (mmHg) | Baseline | 96.8 ± 7.6 | 94.2 ± 6.2 | 0.124 |
| Second minute after the start of ventilation | 95.3 ± 8.5 | 89.6 ± 6.4 | 0.002 | |
| Fifth minute after endotracheal intubation | 95.6 ± 7.9 | 90.4 ± 6.7 | 0.005 | |
| Diastolic blood pressure (mmHg) | Baseline | 44.3 ± 6 | 43.3 ± 4.8 | 0.419 |
| Second minute after the start of ventilation | 43.9 ± 7.1 | 41 ± 4.4 | 0.041 | |
| Fifth minute after endotracheal intubation | 44.2 ± 6.4 | 41.4 ± 5.03 | 0.049 | |
| MAP (mmHg) | Baseline | 61.8 ± 6.04 | 60.3 ± 4.9 | 0.244 |
| Second minute after the start of ventilation | 61 ± 7.2 | 57.2 ± 4.4 | 0.009 | |
| Fifth minute after endotracheal intubation | 61.3 ± 6.4 | 57.8 ± 5.1 | 0.012 | |
| Heart rate (bpm) | Baseline | 125.9 ± 10.6 | 123.6 ± 8.8 | 0.307 |
| Second minute after the start of ventilation | 135.5 ± 12.2 | 130.5 ± 9.5 | 0.062 | |
| Fifth minute after endotracheal intubation | 127.3 ± 10.1 | 126.3 ± 5.7 | 0.662 |
Mean SPO2, Systolic and Diastolic Blood Pressure, Mean Arterial Blood Pressure (MAP), and Heart Rate at Different Times in the Two Groups a
Also, there was no significant difference between the two groups in the frequency of SPO2 drop (P value = 0.12) and the impossibility of ventilation (P value = 0.50) during masking (Table 3).
| Variables | Face Mask Group | Nasal Mask Group | P-Value |
|---|---|---|---|
| Drop SPO2 | 0 (0) | 3 (8.6) | 0.12 |
| Impossibility of ventilation | 0 (0) | 1 (2.9) | 0.50 |
Frequency Distribution of SPO2 Drop and Impossibility of Ventilation During Masking Time in Two Groups a
5. Discussion
In the present study, we compared ventilation quality after general anesthesia induction in children aged 3 to 12 years using a face anatomical mask or nasal mask. Based on the results, considering the first type error of 5% and a significance level of 0.05, we measured EtCO2 in the second minute after the start of ventilation and systolic, diastolic, and moderate blood pressure in the second minute after the start of ventilation and the fifth minute after intubation, showing a significant difference between the two groups so that blood pressure variables were lower and EtCO2 was higher in the nasal mask group. Other variables such as heart rate, oxygen pressure, oxygen pressure drop, mean expiratory volume, mean EtCO2, and mean airway pressure did not differ significantly between the two groups of masking methods. However, the results notably indicate that both methods significantly affected ventilation and despite the difference in blood pressure parameters between the two groups, the difference between the two methods in these parameters was in the normal range. It should be noted that although EtCO2 was higher in the nasal mask group than in the other group, EtCO2 in both groups was within the normal range due to the 95% confidence interval.
In other words, it can be said that EtCO2 in the second minute after initiating ventilation in the nasal mask group was significantly better than that in the face mask group, and in the fifth minute after endotracheal intubation, no significant difference was found between the two groups. Therefore, it may be better to ventilate the nasal airway in children than in the face. In fact, it can be said that as the nasal mask method is preferred in patients with difficult mask ventilation, the nasal airway ventilation method can be used in children (especially those with difficult mask ventilation).
Nasal mask ventilation is commonly used in short-term anesthesia, such as anesthesia in dental procedures and continuous positive airway pressure (CPAP) in people with obstructive sleep apnea to create positive airway pressure (7, 14). In the latter case, it significantly affects CPAP due to the physical prevention of upper airway overlap (11). Therefore, it is a reason for justifying nasal masks in general anesthesia. When installing a nasal mask, increasing the pressure in the nasal cavity and not increasing the pressure in the oral cavity causes a pressure difference between the nasopharynx and the oral cavity, which helps push back the soft palate and tongue and prevent the collapse. However, when using a full face mask, an increase in pressure is created in the oral cavity, and this pressure difference is not achieved.
Several studies have compared the quality of ventilation after general anesthesia induction with two methods of mask ventilation. Some have reported the superiority of the nasal mask over the face mask in terms of ventilation parameters for CPAP ventilation. This discrepancy can be explained by the difference in pressure and the positive pressure that the nasal mask creates, preventing the collapse and obstruction of the upper airway (15-17). It has also been shown that a better compliance nasal mask is more comfortable in CPAP and has less gas leakage (18).
In 2008, Liang et al. (11) examined ventilation with a nasal mask compared to a combined nasal and oral mask. In this study performed on 17 patients, the patients first underwent ventilation with a combination mask and then a nasal mask. According to the results, the nasal mask had significantly more effective ventilation than the mouth-nose mask, and less carbon dioxide pressure, more oxygen pressure, and more expiratory tidal volume were obtained. Although our study tried to prove the superiority of the nasal mask over the face anatomical mask, the reason for the difference between the results of our study and the above-mentioned study was the difference in the mask, the difference in the method studied and recruiting individuals to control and the lack of replacement groups studied in Liang et al.'s study (11). In other words, in Liang's study, it was better to put a nasal mask on one group and a mouth-nose mask on the other group from the beginning.
One of the reasons for the difference between the results of the present study and other similar studies is the lack of examination and matching for BMI in the two groups. However, considering that the average weight of the two groups of children was not different, this assumption can be somewhat trusted. In addition, given that our study compared the two methods in children, we can explain the difference in results with other similar studies.
There are two main points in using a mask: complete sealing between the face and the mask with no gas leakage and the openness of the patient's airways, which should always be checked. The quality of sealing in spontaneous ventilation is determined by the filling and movements of the mask storage bag. Gas leaks usually occur around the nose and cheeks. It should be noted that there is no need to seal when using a nasal mask. On the other hand, the symptoms of airway obstruction depend on the location and extent of the obstruction and whether the positive pressure method is used or breathing is done spontaneously. The most important clinical sign is airway obstruction. Snoring occurs in the supraglottic occlusion, and the tail stridor occurs in the gluteal occlusion, a classical sign of airway obstruction in spontaneous respiration (19, 20).
One of the limitations of the present study is the lack of examination and matching for body mass index in the two groups, which makes it difficult to conclude. It is recommended to conduct a comparative study of hemodynamic changes in these two methods because it has been proven that hypotension and the subsequent increase in heart rate are the side effects of anesthetic induction drugs, especially thiopental and opioids (21, 22). However, why was there a significant difference between our two study groups? Whether this difference was random or whether the nasal mask caused a further drop in blood pressure is a subject that should be considered in future studies.
5.1. Conclusions
Since the nasal mask does not create positive pressure on the tongue and soft palate and the difficulty of the nasal airway, a collapse does not occur with this method. Hence, nasal masks can be used as an alternative in children due to the anatomical features of the airways and the possibility of further airway obstruction, and in other people in whom sealing is difficult, and the possibility of preparing a face mask is low. The results of the present study showed that in terms of ventilation parameters, both methods had similar results and performance except for EtCO2, which was significantly higher in the second minute after ventilation in the nasal mask group than in the face mask group; of course, both were in the normal range. Another difference between the two methods was people's blood pressure after ventilation; however, the blood pressure parameters were within the normal range.