1. Background
Ineffective management of postoperative pain following pediatric cardiac surgery conducted through a sternotomy adversely affects a patient’s postoperative course. It could result in delayed recovery, prolonged mechanical ventilation, prolonged intensive care unit (ICU) stay, prolonged hospital stay, and/or adverse psychological sequelae (1). One of the essential requirements of an enhanced recovery program following cardiac surgery is the proper control of post-sternotomy pain without significant sedation or side effects (2). Accordingly, various analgesic tools have been used to alleviate intraoperative and postoperative sternotomy pain. These tools include a number of multimodal analgesics, including paracetamol, nonsteroidal anti-inflammatory drugs (NSAIDs), and opioids. Non-pharmacological techniques used to control sternotomy pain include such thoracic regional analgesic techniques as thoracic epidural anesthesia (TEA), paravertebral block (PVB), intercostal nerve block, transversus thoracic plane block, parasternal plane block, and erector spinae plane (ESP) block (3-6).
The ESP block has been described in the literature regarding perioperative pain management. It has been used unilaterally in thoracic surgeries and bilaterally in cardiac surgeries. It has the advantages of being technically simpler and safer than other local anesthetic techniques, such as thoracic paravertebral and thoracic epidural block (7).
Since 2016, few studies have been conducted to assess the efficacy of the ESP block in thoracic and cardiac surgeries. We hypothesized that bilateral ESP blocks in pediatric patients would decrease intraoperative fentanyl consumption, reduce the need for postoperative morphine consumption, and improve pain scores.
2. Objectives
The aim of this study was to assess the efficacy and safety of bilateral ESP blocks in pediatric patients undergoing cardiac surgeries through a median sternotomy.
3. Methods
This study was a randomized controlled, double-blinded clinical trial. The randomization task was performed by an independent party who used an online random number generator. Patients were divided into 2 groups: the ES group (n = 50) who received bilateral ultrasound-guided ESP blocks, and the N group (n = 48) who received no regional anesthesia. Patient study code numbers and allocations were placed in closed numbered envelopes. Following the induction of general anesthesia, envelopes were opened to reveal group assignments. ESP blocks were carried out by a single regional anesthesia consultant.
To achieve blinding of the study, the same surgical dressing was applied to the back of all the participants. During the intervention, another anesthesia team was out of the operating room and took over when the ESP block and full surgical draping were performed (just before the skin incision). Moreover, the nurses who recorded postoperative data in the ICU were blinded to the nature of the research and intraoperative interventions.
This clinical trial was carried out at Cairo University Pediatric Hospital between July 2020 and August 2021 after receiving approval from the institutional ethical committee. It was registered on clinicaltrials.gov with reference number NCT04452656. Each parent/legal guardian was given a thorough explanation of the procedure before signing an informed consent form for the child to participate in the study.
The study involved 98 children aged 6 months to 7 years who were American Society of Anesthesiologists (ASA) II and III and scheduled for cardiac surgery through a sternotomy. Exclusion criteria included redo surgeries, emergency surgeries, vertebral column anomalies, refusal of the parent/legal guardian, coagulopathy, preoperative injection site infection, history of allergy to any of the utilized medications, cyanotic heart disease, patients with single ventricles, and severe cardiac, renal, or hepatic insufficiency.
3.1. Anesthesia Management
A peripheral intravenous line was secured for each patient in the inpatient ward 1 day prior to the operation. Premedication in the form of midazolam 0.05 mg.kg-1, ketamine 1 mg.kg-1, and atropine 0.05 mg.kg-1 was intravenously administered before transferring the patient to the operating room. As per “standard” intraoperative monitoring, an electrocardiogram, pulse oximeter, and non-invasive arterial pressure monitor were connected to the patient. Induction of anesthesia was achieved with the intravenous administration of 2 mg.kg-1 of ketamine, 0.5 - 1 µg.kg-1 of fentanyl, and 0.5 - 2 mg.kg-1 of atracurium. Additional monitors, including a capnogram, inhalational gas analyzer, invasive arterial pressure monitor, central venous pressure monitor, transesophageal echo (TEE) probe, and near infra-red spectrophotometer (NIRS), were then connected to the patient. After induction, 30 mg.kg-1 of cefazolin was administered as antibiotic prophylaxis. Maintenance of anesthesia was achieved through an inhalational 1.2% - 2% sevoflurane mixture in oxygen and the infusion of 0.5 mg.kg-1.h-1 of atracurium.
Intraoperative analgesia was achieved by administering 0.5 - 1 µg.kg-1 of fentanyl plus 15 mg.kg-1 of paracetamol, given to all patients concomitantly with induction of anesthesia. Additional analgesic medication in the form of boluses of 0.5 - 2 µg.kg-1 of fentanyl was administered in the event of a persistent rise in systolic arterial pressure or heart rate of more than 20% of baseline readings (confirmed by 2 consecutive readings). To control postoperative nausea and vomiting, 0.1 mg.kg-1 of dexamethasone and 10 μg.kg-1 of granisetron were administered to all patients.
The administration of both the inhalational anesthetic agent and atracurium infusion was stopped after the surgeon finished suturing the skin incision. A trial of endotracheal extubation was conducted in the operating room if extubation criteria stipulated by the institutional policy were met. These are the return of motor power, normal arterial blood gas analysis, body temperature ≥ 36°C, and stable hemodynamics. After 30 minutes, patients were transferred to the ICU, whether they were still intubated or extubated. At the ICU, all patients received 10 mg.kg-1 of paracetamol every 6 hours. A trained nurse evaluated and recorded postoperative pain using the FLACC (face, legs, activity, consolability, and cry) pain chart. It consists of 5 categories: (F) face; (L) legs; (A) activity; (C) consolability; and (C) cry. Every category is scored from 0 to 2, resulting in a total score between 0 and 10. If a patient’s FLACC score was ≥ 4, 0.05 mg.kg-1 of morphine was administered intravenously.
3.2. ESP Block Technique
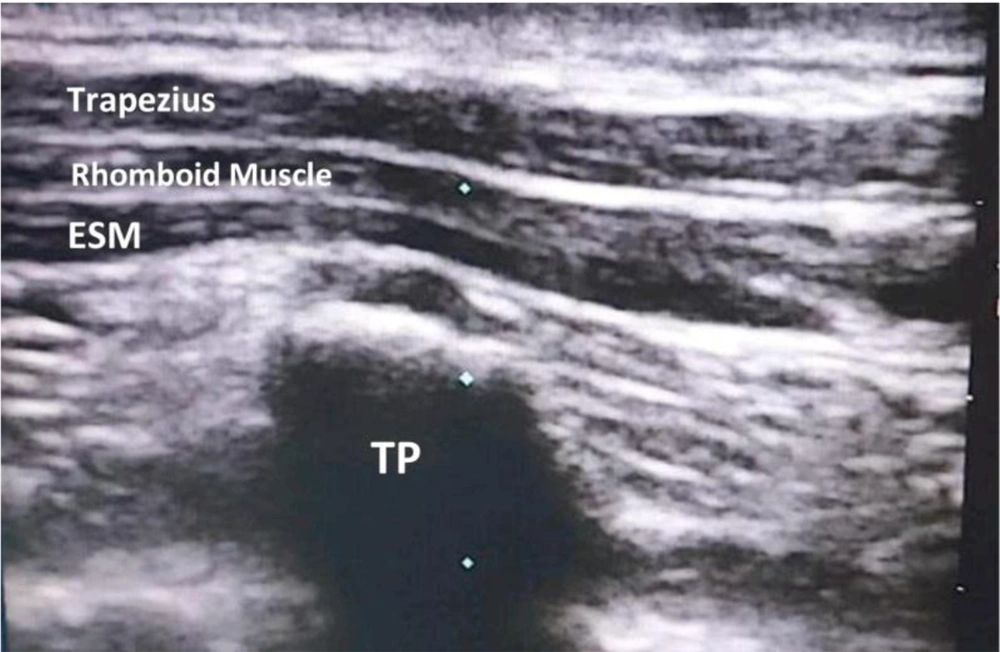
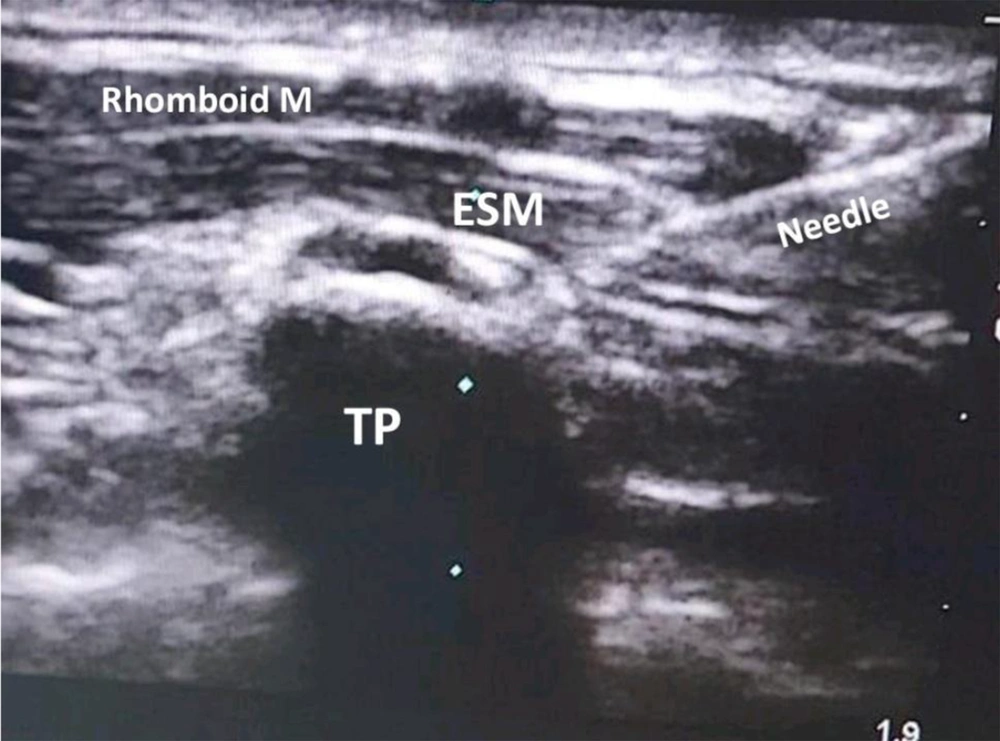
The ESP block was conducted under complete aseptic conditions with ultrasound machine guidance (SonoSite Inc, Bothell, WA, USA). After induction of anesthesia was accomplished, the patient was turned to the prone position. Then, the fifth thoracic spinous process (T5) was identified by palpating and counting down from the seventh cervical spinous process (C7). A high-frequency 7 to 13-MHz linear ultrasound transducer was placed in a parasagittal (parallel) position lateral to the T5 spinous process. Then, the probe was moved from lateral to medial until it was positioned over the tip of the transverse process. Transverse processes could be differentiated from the proximal ribs by their squared-off appearance. The trapezius muscle, rhomboids major muscle, and erector spinae muscle could be recognized overlying the hyperechoic transverse process (Figure 1). Using an in-plane approach, a Simplex® Ultra 360® 22 gauge (35 mm) echogenic needle was inserted in the caudal-cephalad direction until the tip was deep into the erector spinae muscle and hit the transverse process. The correct needle tip location was confirmed by injecting 1 mL of normal saline and visualizing the linear spread in the fascial plane between the erector spinae muscle and the transverse process (Figure 2). Then, 0.4 ml.kg-1 of bupivacaine 0.25% was injected. After that, the procedure was performed on the other side in the same manner as described above (8, 9).
The primary outcome was the total dose of administered fentanyl intraoperatively. Secondary outcomes included the morphine consumption in the first 24 hours postoperatively, the length of time before the first need for postoperative analgesia (defined as the time between extubation and a FLACC score ≥ 4), the place of extubation (operating theatre or ICU), and FLACC scores in the first and second hour postoperatively and at every 4 hours for a period of 24 hours. Incidences of postoperative complications, including postoperative nausea vomiting (PONV), itching, respiratory depression, pneumothorax, and prolonged paresthesia, were also considered as secondary outcomes of this study.
3.3. Sample Size
A statistician calculated the sample size by comparing intraoperative fentanyl consumption between children who had undergone sternotomies and had received ESP blocks with those who had received conventional anesthesia (as reported by a previous study) (10). In that study, the mean ± SD of intraoperative fentanyl consumption stood at approximately 10.45 ± 3.2 µg.kg-1 in the ESP group and approximately 11.46 ± 2.1 µg.kg-1 in the conventional group. Accordingly, using the Student t test for independent samples, the statistician found the minimum proper sample size needed to detect a real difference of 1.2 µg.kg-1 with 80% power at Cronbach α = 0.05 level to have stood at 47 participants for each group. We increased the sample size to 54 patients in each group to compensate for drop-outs. The sample size calculation was performed using the PS Power and Sample Size Calculations software version 3.0.11 for MS Windows (William D. Dupont and Walton D., Vanderbilt University, Nashville, Tennessee, USA).
3.4. Statistical Analysis
Data were analyzed using SPSS version 20 (SPSS Inc, Chicago, Ill, USA). The Kolmogorov-Smirnov test was used to verify the normality of the distribution of variables. Comparisons between groups for categorical variables were assessed using the chi-square test (Fisher or Monte Carlo). The Student t test was used to compare differences between the 2 study groups regarding normally distributed quantitative variables, while the Mann-Whitney test was used to compare differences between the 2 groups regarding not-normally distributed quantitative variables. The significance of the obtained results was judged at the 5% level.
4. Results
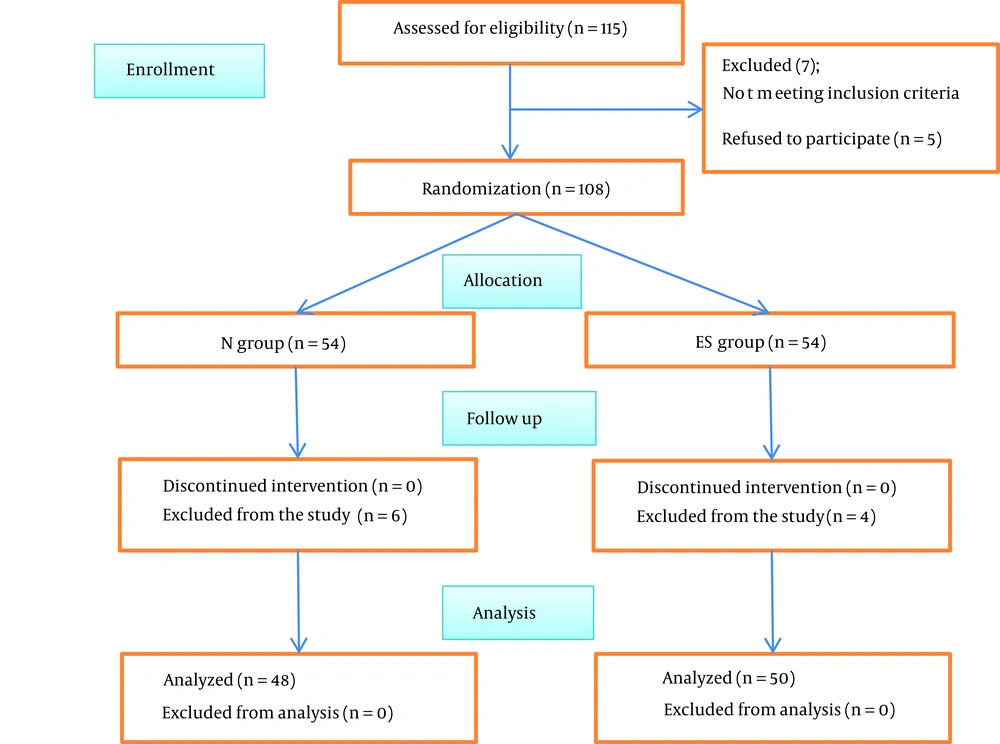
A total of 115 pediatric patients were assessed for eligibility to participate in this study. Five children were excluded from the study because their parents did not consent to participate. Two children were excluded because they were redo cases. A total of 108 children met the inclusion criteria. They were allocated into 2 groups: the ES group who received ESP blocks and the N group who received no block. Fifty-four patients were initially allocated to each group. Four patients from the ES group and 6 patients from the N group were excluded from the study due to complicated postoperative courses. A remaining total of 98 children participated and completed the study, and their data were successfully analyzed (Figure 3).
There were no statistically significant differences between both groups in terms of age, sex, weight, or height. The type and duration of surgical procedures and ASA classifications were also comparable between both groups (Table 1).
| Variables | Group N (n = 48) | Group ES (n = 50) | P Value |
|---|---|---|---|
| Age (mo) | 0.230 | ||
| Mean ± SD | 33.5 ± 24.9 | 28.2 ± 25.3 | |
| Median (min - max) | 33.5 (6 - 84) | 14.5 (6 - 84) | |
| Weight (kg) | 0.201 | ||
| Mean ± SD | 13 ± 7 | 11.7 ± 7.3 | |
| Median (min - max) | 14 (4.8 - 36) | 9.8 (3.2 - 38) | |
| Height (cm) | 0.356 | ||
| Mean ± SD | 88 ± 20.3 | 84.1 ± 20.8 | |
| Median (min - max) | 90 (60 - 129) | 80.5 (56 - 135) | |
| Sex (male/female) | 0.980 | ||
| Male | 21 (43.8) | 22 (44) | |
| Female | 27 (56.3) | 28 (56) | |
| ASA | 0.563 | ||
| II | 27 (56.3) | 31 (62) | |
| III | 21 (43.8) | 19 (38) | |
| Surgical duration (min) | 0.557 | ||
| Mean ± SD | 142.8 ± 27.8 | 145.9 ± 23.7 | |
| Type of surgical procedure | |||
| VSD closure | 19 (39.6) | 27 (54) | 0.153 |
| ASD closure | 14 (29.2) | 11 (22) | 0.416 |
| AVSD closure | 10 (20.8) | 8 (16) | 0.537 |
| SAM resection | 2 (4.2) | 3 (6) | 1.000 |
| Mitral valve repair | 2 (4.2) | 0 (0) | 0.237 |
| Supravalvular AS repair | 1 (2.1) | 0 (0) | 0.490 |
| Pulmonary artery banding | 0 (0) | 1 (2) | 1.000 |
a Values are expressed as No. (%) unless otherwise indicated.
The study showed statistically significantly higher levels of intraoperatively administered fentanyl and postoperative morphine consumption in the N group compared with the ES group (P < 0.001). Moreover, the timing of the first rescue analgesia was significantly delayed in the ES group compared with the N group (Table 2).
| Variables | Group N (n = 48) | Group ES (n = 50) | P Value |
|---|---|---|---|
| Primary outcome | |||
| Intraoperative fentanyl (µg.kg-1) | 6.7 ± 3 | 4.3 ± 1.9 | < 0.001 |
| Secondary outcomes | |||
| Postoperative morphine consumption (mg.kg-1) | 0.5 ± 0.2 | 0.4 ± 0.2 | < 0.001 |
| Time to first rescue analgesia (min) | 108.8 ± 47.8 | 231.6 ± 104.5 | < 0.001 |
| Place of extubation | 0.042 | ||
| OR | 18 (37.5) | 29 (58) | |
| ICU | 30 (62.5) | 21 (42) |
a Values are expressed as mean ± SD or No. (%).
A statistically significantly higher percentage of children from the ES group (58%) were extubated in the operating room compared with those from the N group (37.5%; P = 0.04). Consequently, a statistically significantly lower percentage of children from the ES group (42%) were extubated in the ICU compared with those from the N group (62.5%; P = 0.04; Table 2).
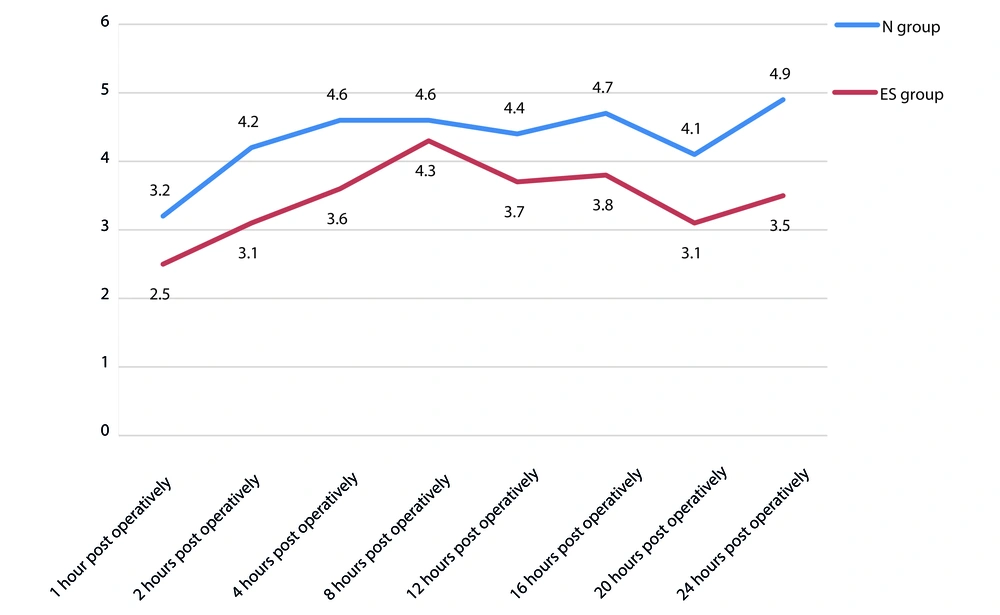
FLACC pain score values were significantly higher in the N group than in the ES group in the first 24 hours postoperatively (Figure 4). The incidence of complications was comparable between both groups with no measurable, significant differences (Table 3).
| Postoperative complications | Group N (n = 48) | Group ES (n = 50) | P Value |
|---|---|---|---|
| Vomiting | 4 (8.3) | 2 (4) | 0.431 |
| Itching | 3 (6.3) | 2 (4) | 0.674 |
| Fever | 2 (4.2) | 3 (6) | 1.000 |
| Respiratory depression | 2 (4.2) | 2 (4) | 1.000 |
| Hypotension | 1 (2.1) | 2 (4) | 1.000 |
| Bradycardia | 2 (4.2) | 0 (0) | 0.237 |
a Values are expressed as No. (%).
5. Discussion
The main findings of the current study are that the bilateral ESP block decreased the perioperative opioid consumption, prolonged the duration of postoperative analgesia, and improved the 24-hour postoperative pain score in children that had undergone cardiac surgery.
The mechanism of action of the ESP block is still not clearly understood (11). Presumably, the injection of a local anesthetic agent in the fascial plane between the erector spinae muscle and the tips of the transverse processes anesthetizes neural structures passing within this space. The local anesthetic agent then presumably spreads out of that space anteriorly and laterally to achieve general anesthesia of the dorsal rami and ventral rami of the spinal nerves and the lateral cutaneous nerve branches. A single-injection ESP block can spread to at least 3 and maximum 8 spinal nerve territories. Thus, a single injection at the fourth or fifth spine process level is presumably sufficient to produce adequate anesthesia for the anterior, lateral, and posterior parts of the chest wall. In this study, we performed a bilateral ESP block to secure complete chest wall anesthesia, with the extension of the anesthetic effect to the sternum (12, 13).
ESP blocks were initially recommended for the management of chronic thoracic pain. Subsequently, a number of clinical trials detailed the role of bilateral ESP blocks in the management of perioperative pain in thoracic and cardiac surgeries (14). Muñoz-Leyva et al published a case series of 5 adult patients for whom they used a catheter technique to deliver continuous bilateral ESP blocks. They reported low intraoperative opioid consumption, early extubation in the operating room, and proper postoperative pain management without supplemental opioids in 4 of 5 cases (15). Tsui et al. also reported decreased intraoperative opioid consumption, early extubation, and decreased postoperative pain in a case report of an adult patient who had received bilateral ESP blocks before a cardiac surgery conducted via sternotomy (16). In a case report of 1 pediatric patient, Wong et al detailed using bilateral ESP blocks to manage perioperative median sternotomy pain. The patient was extubated during the first 3 hours postoperatively, and a pain score of zero was achieved during the 48 hours postoperatively without the use of opioids (17).
Kaushal et al. reported a reduction in intraoperative fentanyl consumption, lower postoperative pain scores, and prolonged postoperative duration of analgesia in pediatric patients who had received bilateral ESP blocks before sternotomy. As with their clinical trial, we aimed to investigate the efficacy of bilateral ESP blocks in pediatric cardiac surgeries. For the most part, our study produced comparable findings to their clinical trial. Some differences existed between the 2 studies. One important difference was the local anesthetic used. We used bupivacaine, 0.25%, as a local anesthetic, while Kaushal et al. used ropivacaine, 0.2%. In addition, our primary endpoint was intraoperative fentanyl consumption, and we used the FLACC score for postoperative pain assessment and morphine for postoperative analgesia. In their study, the primary outcome involved the modified objective pain score (MOPS) at 24 hours postoperatively, and they used fentanyl for intraoperative and postoperative analgesia. Furthermore, our study sample (98 patients) was larger than their sample of 80 patients (10).
Macaire et al. reported a significant reduction of morphine consumption during the 48 hours following pediatric cardiac surgery in patients who had received bilateral ESP blocks with blouses of 0.2% ropivacaine (120 ± 320 µg.kg-1) compared with patients who had received bilateral ESP blocks with saline (512 ± 560 µg.kg-1; P = 0.03). In our study, we noted lower morphine consumption in patients who had received bilateral single-shot ESP blocks with bupivacaine (0.4 ± 0.2 mg.kg-1) compared with those who received no block (0.5 ± 0.2 mg.kg-1; P < 0.001) (18).
Another clinical trial was carried out to assess the efficacy of bilateral ESP block vs. thoracic epidural analgesia in adult patients scheduled for open cardiac surgery. It demonstrated comparable results regarding intraoperative fentanyl consumption and postoperative Visual Analog Scale (VAS), especially in the first 12 hours postoperatively. These results further support the recommendation to use bilateral ESP blocks because of their high efficacy with a low incidence of complications (19).
Krishna et al. found that bilateral ESP blocks with 0.375% ropivacaine produced better analgesia than conventional analgesia with paracetamol and tramadol in an adult population undergoing sternotomy. They reported significant differences between both groups regarding the timing of the first rescue analgesia, standing at 8.9 ± 0.14 hours with the ESP block and 4.6 ± 0.12 hours in the control group (P = 0.0001). In our study, there was a significant delay in the need for first rescue analgesia in the ES group (231.6 ± 104.5 minutes) compared with the N group (108.8 ± 47.8 minutes; P < 0.001) (20).
The safety of ESP blocks was demonstrated by a retrospective study conducted on 164 general and pediatric thoracic surgeries. The authors reported no complications following ESP blocks in pediatric patients. In the current study, we did not record any serious complications in the study population. A small number of complications, such as vomiting, itching, bradycardia, hypotension, and fever, occurred and were managed accordingly with no significant differences between the 2 groups (21).
The limitation of this study was that we did not include complicated cardiac surgeries or cardiac surgical procedures of long duration because it was not included in the scope of our study. Accordingly, we included only ASA II and III patients in our study as per the 2020 ASA classification.
The results of bilateral ESP blocks for the management of perioperative sternotomy pain appear to be promising. Accordingly, we recommend further research to be conducted to compare the efficacy of bilateral ESP block vs other regional techniques in pediatric open cardiac surgeries.
5.1. Conclusions
Bilateral ultrasound-guided ESP blocks can be used to reduce perioperative opioid consumption in pediatric patients undergoing cardiac surgery through a sternotomy. It can also play an important role in decreasing postoperative pain scores and facilitating early extubation.