1. Background
Chronic renal failure (CRF) is an exacerbated and irreversible renal function status. The body’s ability to maintain metabolic and electrolyte balance is impaired, leading to a rise in blood urea and nitrogen and their retention in the body (1). According to the National Kidney Federation (NKF), CRF is defined as each renal damage or diminution in glomerular filtration rate (GFR) up to < 60 mL/min/1.73 m2 of the body’s surface area for above three months (2). The prevalence of renal disease is increasing worldwide, so the number of individuals with end-stage renal disease (ESRD) is estimated to reach 2240000 in the United States by 2030 (3). Hemodialysis is considered the most common treatment for individuals suffering from CRF (4) and needs vascular access.
The establishment of an appropriate vascular pathway, as well as timely dialysis, is the most critical issue in saving a patient’s life. In chronic hemodialysis, several techniques such as arteriovenous fistula (AVF), arteriovenous graft (AVG), and Shaldon and permcath catheters are applied for vascular access (5), the best one of which is the AVF (6, 7). The pain at the region of needle insertion into the fistula can be addressed as one of the reasons of annoyance in hemodialysis patients during dialysis (8), so that above one-fifth of the individuals report this pain as intolerable (8, 9). The patients experience needle pain around 300 - 320 times annually since they often expose to two cannulations in the arteries of the fistula site three times a week (1, 10, 11). The lack of proper pain control leads to more extended hospitalization, higher medical costs for patients and hospitals, dissatisfaction with therapy methods, and frequent referrals to medical centers for controlling pain (12). The patients’ pain relief can increase their acceptance of therapeutic procedures and improve these individuals’ quality of life (QOL). Thus, it is the basis for nursing care (13). As one of the health team members who spend the most time with the patient (14), nurses play a key role in predicting, evaluating, and reducing cannulation pain in patients, especially those undergoing hemodialysis. Accordingly, they should be aware of different pain management techniques to enhance patients’ QOL with a more effective relationship between patients and hemodialysis (15). Nowadays, many advances have been made in pain treatment, and several pharmacological and non-pharmacological approaches have been introduced to relieve pain (1).
Some pharmacological techniques are lidocaine spray, prilocaine, EMLA, and piroxicam creams. Lidocaine is one of the most prevalent and vital agents in local anesthesia. The spray form of this substance is a common formulation clinically utilized with its moderate effect to induce local anesthesia in mucous and cutaneous membranes. The anesthesia is usually generated in 1 - 5 min for 10 - 15 min, depending on its usage site. The theory of pain decline by lidocaine is based on blocking active and inactive sodium channels, leading to conduction blockage and non-stimulation, and consequently, pain distribution or reduction (16). This drug is an aminoamide anesthetic, often used for local anesthesia and pain relief due to the rapid onset of action and moderate effectiveness (17).
Some non-pharmacological approaches to pain reduction are associated with advantages such as easy use, convenience, low cost, less complication, fastness, non-invasiveness, and usability in nursing. Today, researchers have focused on detecting novel methods for managing pain better (7).
Distraction is one of the nursing interventions and non-pharmacological approaches which is effective in pain management. This technique aims at diverting concentration from a painful stimulus, which can lessen fear, anxiety, and pain intensity caused by painful medical procedures (1, 4, 18).
Among the distraction methods, rhythmic breathing is a simple, non-expensive, and non-invasive approach, which is recognized as a solution to increase available oxygen uptake. Nowadays, this method has been welcomed by patients to lower pain. Nurses utilize this technique to care for individuals with acute pain. They can decrease pain intensity by guiding patients to control breathing pattern and learn rhythmic breathing (19, 20). Moreover, safety, lack of complication, non-toxicity, long-term application, and simplicity can be mentioned as the other advantages of this method. Rhythmic breathing causes cognitive distraction and changes in the structure of harmful stimuli such as pain and stress. It makes patients respond subjectively and react behaviorally to pain and anxiety for deceiving the mind in a conscious action to distance from pain. This issue gives individuals a sense of pain and anxiety control and reduces behaviors induced by pain and anxiety (21).
Pain prevention and control are important in hemodialysis patients, so they frequently demand lidocaine spray to reduce dialysis needle pain. Further, non-pharmacological methods such as rhythmic respiration are cost-effective and available, lead to less complication, and can be easily used by nurses.
2. Objectives
The present study compared the effects of rhythmic breathing and lidocaine spray on the pain intensity of hemodialysis needles in patients with AVF.
3. Methods
The present study was extracted from a Master’s thesis on critical care nursing, which was approved by the Ethics Committee of the Gonabad University of Medical Sciences (Code: IR.GMU.REC.1400.040) and registered in the Iranian Registry of Clinical Trials (No.: IRCT20210626051716N1).
This randomized, self-controlled, single-blind two-group clinical trial was conducted among 54 eligible hemodialysis patients referred to the Nikan Farda Clinic in 2021. The subjects were selected based on the inclusion criteria using the convenience sampling method. Sampling continued as long as data saturation was reached, informed written consent was obtained from the participants. Then they were randomly assigned to rhythmic breathing and lidocaine spray groups by applying permuted block technique with four blocks. In each group, the sample size was calculated to be 24 according to the mean comparison formula and the results reported by Asgari et al. (22), regarding the test power of 80%, a confidence level of 95%, and the mean ± SD of pain score in the two groups (3.96 ± 2.14 and 2.3 ± 1.91). Considering the 10% dropout rate, 37 patients were assigned to each group. The formula is as follows:
The inclusion criteria were willingness to participate in this study, aged 18 - 60 years, no addiction to analgesic drugs, and controlled diabetes with fasting blood sugar (FBS) and blood sugar (BS) of 70 - 150 and 120 - 250, respectively. The other criteria were the lack of known lidocaine sensitivity, passing at least three months of fistula placement in the forearm, and having an active record (treating with hemodialysis for three four-hour sessions per week). The other inclusion criteria were having no pacemaker, skin problems, speech, visual, hearing, and cognitive impairment, anesthesia, neuropathic disorders, and vascular diseases in the fistula site.
However, exclusion criteria were failure to insert the needle into the arteries of the fistula area in the first attempt, need for repeated cannulation, lidocaine sensitivity, and unconsciousness at each phase of the study. The patients who were not inclined to cooperate experienced the onset of other chronic pains affecting the assessment of the pain induced by needle insertion into the arteries and did not refer during the research phases (referral to other medical centers to continue treatment, travel, kidney transplant, death) were excluded from the study.
The data were collected using a questionnaire addressing demographic characteristics and information on the history of hemodialysis and the visual analogue scale (VAS) for pain intensity. Many studies have employed the instrument to measure the pain intensity of hemodialysis fistula cannulation (14). VAS is a 10 cm horizontal line from 0 (no pain) to 10 (worst pain) measuring pain intensity based on the patients’ statements. Moreover, the scientific validity and reliability of the questionnaire have been evaluated by several researchers. For example, a study confirmed its reliability by applying the McGill pain questionnaire among individuals with chronic back pain in Tehran (correlation coefficient: 0.86) (23).
Before the intervention, the two groups were examined for pain intensity during needle insertion one minute after completing the hemodialysis needle insertion and fixing the needles in the first hemodialysis session without intervention.
The intervention group was asked to do rhythmic breathing for two minutes before entering the hemodialysis vascular needles. For this purpose, the rhythmic breathing method was taught individually to the subjects in a session prior to the intervention so that they could perform this technique independently without error. In this respect, the patients laid comfortably, closed their eyes, and took a long deep breath via the nose after counting one to three. Then they held their breath in the lungs for three numbers and exhaled through their mouths slowly with three numbers. The subjects repeated this breathing type while inserting hemodialysis vascular needles into the fistula by concentrating on the exercise. Finally, they opened their eyes after one minute of insertion and needle fixation; their pain intensity during the needle insertion was evaluated by the researcher, who was not informed of the type of intervention.
As for the lidocaine group, two puffs of 10% lidocaine spray (20 mg) were sprayed to the needle insertion area from a distance of 5 cm five min before insertion. Then the pain intensity was assessed one minute after the procedure and needle fixation.
Unaware of the type of intervention, the researcher evaluated the pain intensity felt during the insertion of arteriovenous needles using VAS. The intervention was iterated in three consecutive hemodialysis sessions, and pain intensity scores were compared in two groups at pre- and post-intervention phases.
Prior to the intervention, all subjects laid in a comfortable position two minutes before inserting the needles into the fistula vessels, and the insertion site was disinfected with 70% alcohol by the department nurse.
To match the conditions as much as possible, all patients were placed in a supine position under a convenient situation before and after the intervention, the face of whom was rotated to the opposite side of the hand with a fistula, and cannulation was then performed. In all study phases, a dialysis needle (No. 16) was inserted by two skilled nurses into the fistula site from at least a five cm distance with a 30 - 40° angle when the oblique edge of the needle was upside.
Further, SPSS software version 20 was used to analyze the data. The data were analyzed at a significance level of 0.05.
4. Results
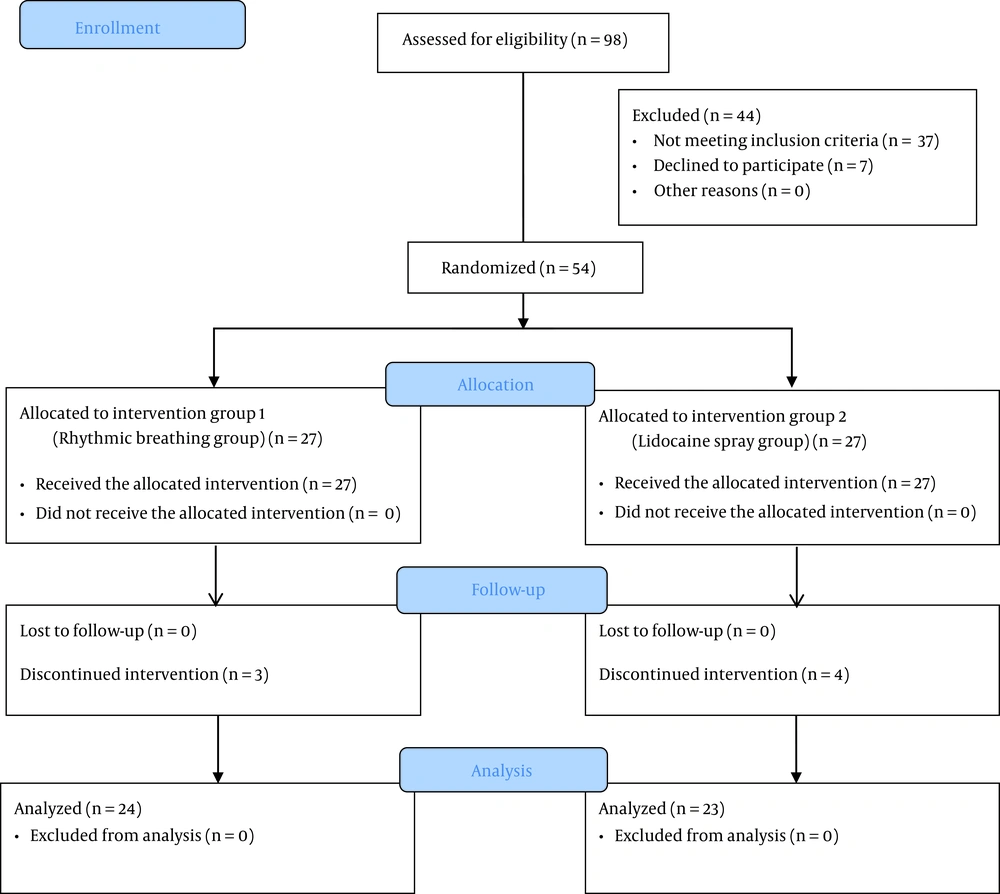
In this study, out of the 98 evaluated patients, 54 individuals met the inclusion criteria. Moreover, seven subjects were excluded from the study due to lidocaine allergy (n = 1), failure in cannulation at the first time (n = 1), non-attendance in hemodialysis session (n = 2), and unwillingness to cooperate (n = 3). In other words, this study was conducted among 47 patients (Figure 1).
According to the study results, the participants’ mean age was 39.5 ± 12.89 years in the rhythmic breathing group and 43.78 ± 10.7 years in the lidocaine spray group. About half of the subjects (53%) were male, and renal failure was caused by diabetes and hypertension in 74% of the participants. Further, 61% of the patients had diplomas and higher degrees, 91% did not smoke, and 70 and 64% were married and unemployed, respectively.
The Kolmogorov-Smirnov test results demonstrated that pre-intervention pain intensity, pain intensity at the first post-intervention phase, and differences in pre- and post-intervention pain scores were normally distributed in the two groups (P > 0.05). However, the other quantitative variables did not follow a normal distribution, at least in one of the groups.
The groups were not significantly different in terms of age, gender, marital status, employment, smoking, FBS, the level of education, etiology of nephropathy, history of hemodialysis treatment, and duration of fistula placement.
Furthermore, no significant difference was observed in the mean pre-intervention pain intensity scores of the two groups despite the higher scores in the lidocaine spray group (P = 0.51). The independent t-test results revealed no significant difference in the pain scores between the groups at the first post-intervention phase (P = 0.192). According to the Mann-Whitney U test results in Table 1, the mean pain scores were not significantly different between the two groups at the second and third post-intervention phases (P = 0.709 and P = 0.67, respectively).
| Pain Intensity Score | Group (Mean ± SD) | Statistical Test | ||
|---|---|---|---|---|
| Rhythmic Breathing | Lidocaine Spray | Independent t-test | Mann-Whitney U | |
| Pre-intervention | 2.54 ± 1.5 | 3.79 ± 2.58 | t = 2.02, df = 35.07, P = 0.051 | - |
| First post-intervention phase | 2.27 ± 1.56 | 3.12 ± 2.63 | t = 1.33, df = 35.51, P = 0.192 | - |
| Second post-intervention phase | 1.87 ± 1.43 | 2.48 ± 2.23 | - | z = 0.373, P = 0.709 |
| Third post-intervention phase | 1.95 ± 1.41 | 2.26 ± 1.84 | - | z = 0.426, P = 0.67 |
As summarized in Table 2, both rhythmic breathing (P = 0.023) and lidocaine spray (P < 0.001) groups experienced a significant decline in post-intervention pain scores.
| Pain Intensity Score | Group(Mean ± SD) | |
|---|---|---|
| Rhythmic Breathing | Lidocaine Spray | |
| Pre-intervention | 2.54 ± 1.5 | 3.79 ± 2.58 |
| First post-intervention phase | 2.27 ± 1.56 | 3.12 ± 2.63 |
| Second post-intervention phase | 1.87 ± 1.43 | 2.48 ± 2.23 |
| Third post-intervention phase | 1.95 ± 1.41 | 2.26 ± 1.84 |
| Friedman test | ||
| df | 3 | 3 |
| χ2 | 9.5 | 20.531 |
| P | 0.023 | < 0.001 |
The difference in the pre-and post-intervention pain intensity scores between the two groups was compared through considering the lack of significant difference each phase of pain assessments between the two groups, as well as evaluating intra-group changes, which reflected less pain intensity scores in both groups. Finally, a larger difference was obtained in the pain intensity scores before and after intervention among the subjects sprayed with lidocaine (1.16 ± 1.56) compared to another group (0.508 ± 1.25). However, the results of the independent t-test represented an insignificant difference (P = 0.117) (Table 3).
| Differences in Pain Intensity Scores | Group (Mean ± SD) | Independent t-test | |
|---|---|---|---|
| Rhythmic Breathing | Lidocaine Spray | ||
| Differences in pre-intervention pain intensity and mean intensity at three post-intervention phases | 0.508 ± 1.25 | 1.16 ± 1.56 | t = - 1.59, df = 45, P = 0.117 |
5. Discussion
The present study compared the effects of rhythmic breathing and lidocaine spray on the pain intensity of needle insertion into AVF in hemodialysis patients. The rhythmic breathing and lidocaine groups were not significantly different in terms of demographic characteristics. However, a statistically significant difference was observed between the two groups in the mean pain intensity before intervention and at three post-intervention phases. Both groups experienced a significant decrease in pain, while the difference in the pre-and post-intervention pain intensity scores was greater in the lidocaine spray group. This was while the difference was not statistically significant.
Several studies have highlighted the effects of lidocaine spray on pain reduction and confirmed the findings of the present study. For example, Asgari et al. reported a significant difference in reducing the mean pain intensity during vascular needle insertion in hemodialysis patients after applying this technique compared to the placebo group (P < 0.001) (22). According to Mirzaei et al. (16), lidocaine spray, EMLA cream, and ice pieces significantly reduced the mean pain intensity during fistula cannulation among the individual’s undergoing hemodialysis compared to the control group. Similar to the present study, they sprayed two puffs of 10% lidocaine spray (20 mg) on the cannulation site of the lidocaine spray group, followed by cannulation after 5 min (P < 0.001). Moreover, aromatherapy with Saliva officinalis and topical lidocaine could significantly decrease the mean pain induced by entering vascular catheters in the hemodialysis patients compared to the control group (17). Aliasgharpour et al. reported a significantly lower mean intensity of the pain induced by entering a needle into AVF in the hemodialysis patients treated with lidocaine gel and lavender inhalation compared to the control group (P <0.001) (24).
Further, the present findings are contrary to Jafarimanesh et al.’s finding indicating an insignificantly further reduction in the pain of vascular access (venipuncture) among the lidocaine spray group compared to the quinine and control ones (P > 0.05). They sprayed 10 puffs of 10% lidocaine spray (20 mg) on the subjects referring to the emergency department 15 min before venipuncture (14). The insignificant effect of lidocaine on decreasing cannulation pain may be justified by differences in patients and the more extended interval between spraying and cannulation in their study despite applying a higher lidocaine dose (25). Some studies revealed the effectiveness of rhythmic breathing, as one of the distraction techniques, in diminishing patient pain, which agrees with the findings of the present study. In this regard, Borzou et al. reported that the mean pain intensity of vascular needle insertion in the individuals with AVF undergoing hemodialysis significantly declined following the rhythmic breathing compared to the non-intervention group (P < 0.001) (19). According to Bagheriyan et al. (26), there was a significant difference in reducing the mean pain intensity of venipuncture among the school-age children performing rhythmic breathing compared to the control group (P < 0.05). Nasirnejad et al. focused on the effects of rhythmic breathing on pain intensity and anxiety in the coronary artery bypass graft (CABG) patients. They found a significant difference in the decreased mean of pain intensity in the intervention group compared to the control one (P < 0.0001) (21). Further, the mean of postoperative pain intensity in the candidates for the same orthopedic surgery significantly decreased by reciting Allah and conducting rhythmic breathing (P < 0.009); hence, those in the Allah’s recitation group experienced less pain (27). The rhythmic breathing significantly decreased pain after changing dressing in the second-degree burn patients and burn ones (28).
Along with distraction for pain relief, breathing has other effects on the body, which include a rise in oxygen uptake (20), posing palliative effects on anxiety, depression, posttraumatic stress disorder, chronic pain, and disease-induced stress (29).
Given that pain is a subjective phenomenon and that no objective criterion is available to measure pain, the findings relied on the patients’ responses, which can be addressed as one of the limitations of this study. Another limitation was the individuals’ previous use of pain control techniques. Finally, further studies are suggested to comment more definitively on comparing the effects of rhythmic breathing and lidocaine on the pain intensity induced by hemodialysis fistula cannulation after removing the above-mentioned limitations.
5.1. Conclusions
The findings rejected the relevant hypothesis posing that rhythmic breathing (non-pharmacological method) and lidocaine spray (pharmacological one) differently affect the pain intensity during needle insertion into the AVF in hemodialysis patients. In other words, both techniques significantly decrease mean pain intensity. Because of the pain reduction following rhythmic breathing, as a non-pharmacological approach with less complication, this method can be applied by nurses in the hemodialysis departments.