1. Background
The most prevalent surgery in the pediatric population is the lower abdomen surgery. During pediatric surgery, regional anesthesia and analgesia procedures are routinely used to reduce narcotic intake, improve pain control, and increase patient-parent satisfaction and the quality of postoperative pain control. Caudal anesthesia is the most general approach used for inguinal hernia repair, urologic surgery, and lower extremity surgery (1). In recent years, special interest has been paid to peripheral nerve blocks (PNBs) to avoid the consequences of neuraxial blocks, which are rare but serious (2). Quadratus lumborum (QL) block is a new abdominal truncal block used for somatic and visceral analgesia in the upper and lower abdomen. Blanco was the first to describe it in 2007 (3). For all Populations (pregnant women, adults, and pediatrics) having abdominal surgery, QL block is currently used as a perioperative pain control (4). Anesthesiologists who provide regional anesthesia increasingly use ultrasonography (US). The US transducer has become the modern anesthesiologist’s new stethoscope, making regional nerve blocks easier to perform (5). Ultrasound-guided PNBs have multiple advantages. The problems’ frequency is reduced when the nervous system and surrounding structures are directly visualized. A more accurate deposition is ensured by direct real-time surveillance of the distribution of the local anesthetic. This increases block quality by making the block start sooner and last longer. It also reduces the number of local anesthetics (6).
2. Objectives
This study compared caudal block with ultrasound-guided QL block, considering block accuracy, hemodynamic stability, pain alleviation, and complications.
3. Methods
After obtaining Fayoum University’s (D141) ethical committee permission and the clinical trials.gov number (NCT03646630), as well as the informed consent from the parents, 52 patients aged 1 to 7 years old of both genders scheduled for unilateral lower abdominal surgery (inguinal hernia, hydrocele, undescended testicles, etc.) were randomly assigned into 2 groups. The randomization sequence was kept hidden in sealed opaque envelopes. After recruitment and admittance to the operating room, the authors unwrapped the envelopes. The group’s allocations were only blinded to assessors, data collectors, and parents of children.
The study was conducted between January 2018 and January 2019. Each group consisted of 26 patients: group QL [unilateral QL block (n = 26)] and group C [caudal block (n = 26)]. Pediatric patients were 1 - 7 years old, with an ASA physical status I - II. The study comprised lower abdominal surgery. The study excluded children having a history of mental retardation, allergic responses to local anesthetics, developmental delay, rash or infection at the injection site, parental refusal, bleeding issues, or anatomical abnormalities. The participants were assessed clinically, excluding those not meeting the criteria. All patients were given atropine (0.02 mg/kg) and IM midazolam (0.2 mg/kg) as sedatives. Continuous pulse oximetry, non-invasive arterial blood pressure monitoring, and electrocardiogram (ECG) were used during the perioperative period. After induction of general anesthesia, an intravenous (IV) cannula was conducted with a face mask using 50% oxygen and sevoflurane 8%. Fentanyl was given intravenously at a rate of 1 μg/kg, and a laryngeal mask airway was used to secure the upper airway, with the patient breathing on his own. Isoflurane and 50% oxygen were used to maintain anesthesia. Following the induction of general anesthesia, group C achieved a lateral position with the lower hip flexed at a 45° angle and the upper hip flexed at a 90° angle.
The sacral hiatus was approximated by drawing a line connecting the posterior superior iliac spines bilaterally and using it as one-half of an equilateral triangle. The sacral hiatus could be detected as a dimple between the sacral cornua’s 2 bony prominences. If the posterior surface of the sacral bone was encountered, a 22 gauge needle was inserted at a 45° angle to the sacrum and redirected toward the sacral canal after penetrating the sacrococcygeal ligament, depending on the traditional loss of resistance technique or by auscultation of the gush of local anesthetics on the back during the injection. Children received caudal block as 1 mL/kg of 0.25% bupivacaine. Unlikely, in group QL, the ultrasound system used was Sonosite M Turbo (USA), and the scanning probe was the linear multi-frequency 13 - 6 MHz transducer (L25 x 13 - 6 MHz linear array). The used needles were B Braun Stimuplex D needles (Germany). For needle insertion, patients were kept in the lateral position while the US site was blocked and sterilized. A high-frequency linear probe was used on the lateral abdomen, cephalic to the iliac crest. After observing the QL muscle, the probe was turned slightly to the caudal direction to reveal the QL muscle’s largest slice and confirm its posterior aspect. A 22-G block needle was put in-plane, ~1 cm ventral to the probe (Stimuplex D, Braun, Hongo, Bunkyo-Ku, and Tokyo).
The needle tip was inserted until it reached the posterior fascia of the QL muscle. After injecting a small quantity of saline to confirm the tip’s position between the QL muscle, the erector spinae, and latissimus dorsi muscles (posterior or QL block type 2), the local anesthetic was given as a bolus of 0.5 mL/kg bupivacaine (0.25%). The surgery could be started 10 minutes after the block was applied. All patients received acetaminophen 15 mg/kg IV after surgery. Any issues that occurred during the procedure were documented. After completing the surgical operation and waking up from anesthesia, the patient was referred to the post-anesthesia care unit (PACU). At 30 minutes and 1, 2, 4, 6, 12, and 24 hours after surgery, the quality of analgesia was measured using the face, legs, activity, cry, consolability (FLACC) scale (7). If the FLACC scale was more than 4, diclofenac sodium (1 mg/kg) was given rectally as a rescue analgesic to patients in all research groups in the PACU.
Parents were told about the pain evaluation and instructed to give their children oral paracetamol (30 mg/kg) if they felt pain at home. An anesthesiologist recorded the data acquired from the parents over the phone. Intraoperative measurements, such as hemodynamic parameters [heart rate (HR)] and diastolic and systolic arterial blood pressures), were monitored every 15 minutes until the end of the operation and postoperatively. Under ultrasound guidance, problems such as injury to the underlying structures (injury to the liver or a vicious), hemodynamic instability, and hematoma development were documented. Signs of local anesthetics toxicity were also recorded. Postoperative parameters were measured as time to first analgesic rescue as a primary outcome for 24 hours postoperatively. The FLACC Scale was assessed at 30 minutes and 1, 2, 4, 6, 12, and 24 hours by investigators until hospital discharge and then through a telephone interview with parents as a secondary outcome (8). Parents’ satisfaction was recorded as a secondary outcome. Satisfaction measures were measured on a 3-point scale as follows: unsatisfied, satisfied, and very satisfied.
3.1. Sample Size Calculation
Prior to the investigation, the sample size was determined by the G* Power software version 3.1.7 (Heinrich Heine University, Dusseldorf, Germany). Every group consisted of a minimum of 26 subjects to gain significant values based on previous similar research with an estimated effect size (d) of 0.85, 2 tails (2-sided), type 1 error of 0.05, and increasing the power of the study to 90% (8, 9).
3.2. Statistical Analysis
SPSS version 18 (SPSS Inc., Chicago, Ill, USA) was used to analyze the data. Qualitative data were represented as numbers and percentages. Arithmetic means represented central tendency, and SDs represented the dispersion of quantitative parametric data. An independent Student t test was used to compare measures of 2 independent groups of the quantitative data. The chi-square test was used to compare 2 or more qualitative groups in the qualitative data. P values equal to or less than 0.05 were considered statistically significant.
4. Results
The collected demographic data, including weight, ASA classification, age, gender, and operation duration, revealed non-significant variations between the 2 groups (P > 0.05), indicating good demographic matching. About 71% of the study population was male (Table 1).
| Variables | QL Group (n = 26) | Caudal Group (n = 26) | P Value |
|---|---|---|---|
| Age (y) | 4.06 ±1.6 | 4.31 ±1.9 | 0.6 |
| Gender b | |||
| Male | 18 (69.2) | 19 (73.1) | 0.9 |
| Female | 8 (30.8) | 7 (26.9) | |
| Weight (kg) | 14.3 ± 2.2 | 14.9 ± 2.7 | 0.35 |
| Duration of surgery (min) | 46.2 ± 3 | 45.7 ± 4.9 | 0.64 |
Abbreviation: QL, quadratus lumborum.
a Values are expressed as mean ± SD or No. (%).
b P values equal to or less than 0.05 were considered statistically significant.
A non-significant variation was observed in the type of surgery between the study groups (P > 0.05), indicating that they were matched correctly (Table 2). For 45 minutes intraoperatively, a non-significant difference was determined between the groups regarding hemodynamics systolic blood pressure (SBP), diastolic blood pressure (DBP), and HR (P > 0.05), except for measurement at 30 minutes, revealing a statistically significant higher SBP in group C than in group QL (P < 0.03; Table 3).
| Blood Pressure | QL Group (n=26) | Caudal Group (n=26) | P Value |
|---|---|---|---|
| SBP | |||
| Preoperative | 99 ±12.1 | 101.9 ±9.8 | 0.4 |
| 15 minutes | 99.04 ±14.5 | 104.3 ±10.6 | 0.1 |
| 30 minutes | 98.2 ±16.2 | 106.9 ±12.4 | 0.03 b |
| 45 minutes | 99.4 ±16.1 | 100.7 ±20.7 | 0.8 |
| DBP | |||
| Preoperative | 51.4 ±10.4 | 53.9 ±15.2 | 0.5 |
| 15 minutes | 51.7 ±13.3 | 55.2 ±15.8 | 0.4 |
| 30 minutes | 51.1 ±15.6 | 51.8 ±16.2 | 0.9 |
| 45 minutes | 53.8 ±13.2 | 51.9 ±12.8 | 0.6 |
| HR | |||
| Preoperative | 114 ±16 | 112 ±12 | 0.6 |
| 15 minutes | 109 ±15 | 105 ±9 | 0.3 |
| 30 minutes | 110 ±13 | 104 ±10 | 0.07 |
| 45 minutes | 104 ±13 | 103 ±7 | 0.6 |
Abbreviations: QL, quadratus lumborum; SBP, systolic blood pressure; DBP, diastolic blood pressure; HR, heart rate.
a Values are expressed as mean ± SD.
b P values equal to or less than 0.05 were considered statistically significant.
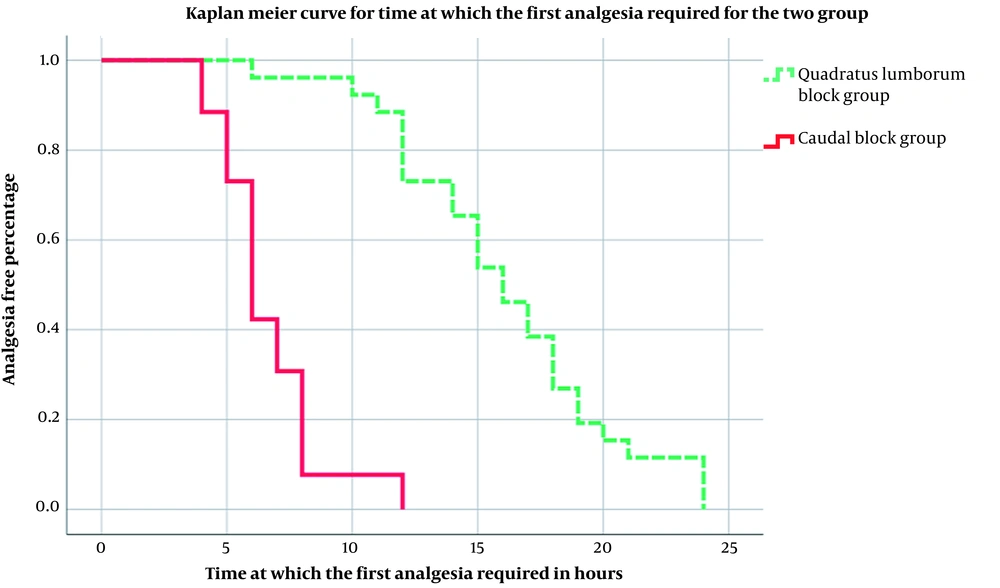
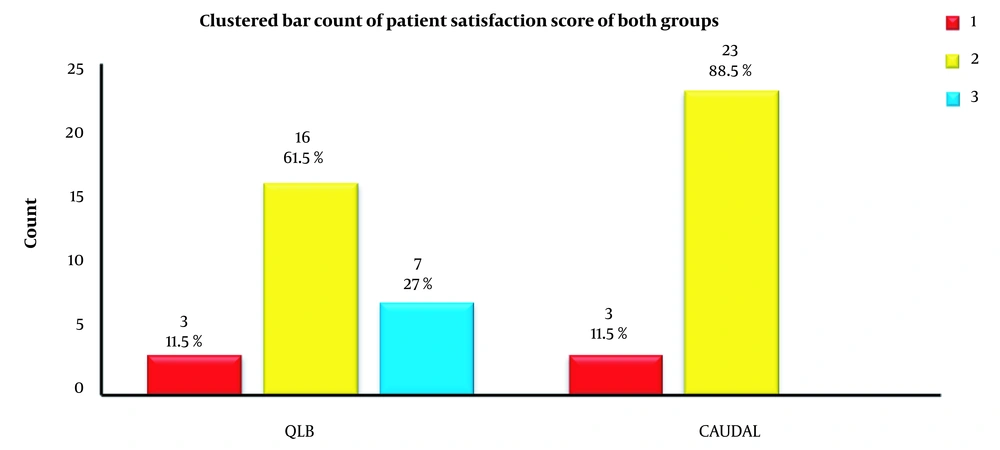
No intraoperative complications were detected regarding the regional anesthetic techniques or local anesthetic systemic toxicity. Regarding intraoperative complications, a non-significant difference was observed between research groups (P > 0.05). Considering postoperative pain assessment, a non-significant difference was observed regarding the severity of postoperative pain (P > 0.05), as assessed by the FLACC score up to 24 hours postoperatively, indicating that patients undergoing both types of anesthesia had a low level of postoperative pain (Table 4). Regarding postoperative analgesic requests, patients in group QL stayed longer until they asked for an analgesic. A significant difference was observed in the time until the first request for analgesia postoperatively (P < 0.001), with group QL (16.1 ± 4.47) having a significantly longer time than group C (6.7 ± 2.03; Figure 1). Among the majority of parents of both study groups who were reported to be satisfied (88.5), about 27% of group QL were very satisfied, indicating that group QL showed a higher level of satisfaction than group C. The degree of parent satisfaction demonstrated a statistically significant difference (P < 0.02; Figure 2).
| FLACC Score | QL Group (n=26) | Caudal Group (n=26) | P Value |
|---|---|---|---|
| 30 minutes | 3 (2) 2-4 | 2 (1) 2 - 3 | 0.187 |
| 1 hour | 2 (1) 1-2 | 2 (1) 1 - 2 | 0.377 |
| 2 hours | 1 (1) 1-2 | 1 (1) 1 - 2 | 0.292 |
| 4 hours | 1.5 (1) 1-2 | 1 (1) 1 - 2 | 0.755 |
| 6 hours | 2 (1) 1-2 | 2 (0) | 0.472 |
| 12 hours | 2 (2) 1-3 | 2 (1) 2 - 3 | 0.138 |
| 24 hours | 3 (1) 2-3 | 3 (1) 2 - 3 | 0.703 |
Abbreviations: QL, quadratus lumborum; FLACC, face, legs, activity, cry, consolability.
a Values are expressed as median (interquartile range) 25th percentile to 75th percentile.
5. Discussion
For lower abdominal procedures in children, many regional anesthetic approaches have been applied to achieve effective and long-lasting postoperative analgesia with reliable parent satisfaction. Our prospective randomized controlled study in pediatric individuals who underwent unilateral lower abdominal surgeries showed that the posterior QL block provided long-lasting postoperative analgesia maintained for up to 16 hours compared with caudal block with greater parent satisfaction in group QL. In both groups, no significance was observed in the FLACC scores up to 24 hours postoperatively.
Hemodynamic stability was recorded in both groups. In most of our discussion, we focused on 7 randomized controlled studies performed with lower abdominal surgeries in pediatric populations, comparing the analgesic efficacy of QL block to other regional anesthetic techniques by Zhao et al. in their recent meta-analysis study. We considered our results a recent addition to their findings to ensure the analgesic efficacy of posterior QL block (10). Our primary finding was the time of the first analgesia required postoperatively, which was significantly longer in group QL than in group C (16.1 ± 4.47 and 6.7 ± 2.03, respectively). Studies by Sato, Ipek et al., and Oksuz et al. (11-13) compared QL block and caudal block, reported in the meta-analysis study by Zhao et al. (10). Only Ipek et al. recorded the required time of first postoperative analgesia. Despite using the same concentration of local anesthetic (0.25% bupivacaine, 0.5 mL/kg) in QL block, their results were against ours as it was 2.17 ± 1.94 h in the QL1 (lateral QL block) group compared to 5.08 ± 5.71 in the caudal group. This discrepancy might be due to the difference in QL block technique, as Ipek et al. performed lateral QL block, while we used posterior QL block, or it might be due to our usage of multimodal analgesia as we used 1 µcg/kg fentanyl during induction, and 15 mg acetaminophen was given IV postoperatively. Ipek et al. used 1 µcg/kg fentanyl during induction but did not use IV non-steroidal analgesic (12).
In the study by Samerchua et al., when they recorded the time of the first dose of oral acetaminophen given postoperatively to 40 children aged 1 - 7 years who underwent ilioinguinal (IL) herniotomy, 20 of them had US-guided QL block, and the other 20 children had US-guided IL and iliohypogastric (IH) nerve block. They found that the time of the first dose of oral acetaminophen was insignificantly longer in the QL block group than in the IL/IH group (8.4 ± 4.1 and 4.8 ± 2.2, respectively) (14). The time of the first analgesic required was recorded by Genc Moralar et al. when they studied the effect of QL1 block compared to IV opioids on the postoperative analgesic requirement in pediatrics in lower abdominal surgeries, and it was significantly longer in the QL1 block group than in the IV opioid group (8.00 ± 5.29 and 3.5 ± 2.06 hours, respectively) (15). Aksu et al. recorded the time of first postoperative analgesia when they compared QL3 block with erector spinae paravertebral block; their results are insignificantly consistent with the current study (16). Oksuz et al., in an earlier study, reported a prolonged postoperative analgesic duration in QL2 block, reaching up to 15 hours when 0.5 mL/kg of 0.25% bupivacaine with IV acetaminophen (15 mg) given postoperatively (13). This long-lasting maintained postoperative analgesia of QL block was also reported in other studies that used QL block in other surgical procedures in pediatrics. An earlier study by Öksüz and Doğan reported that the time of first required analgesia reached up to 17 hours when they compared QL2 block using 0.25% bupivacaine (0.7 mL/kg) with wound infiltration block in laparoscopic-assisted surgery pyeloplasty (17). It was also reported that QL block in adults in cesarean section reached up to 24 - 48 hours with multimodal analgesia (18, 19). In present study, the QL2 block and caudal block demonstrated statistically similar results when compared based on the FLACC scores at 30 minutes and 1, 2, 4, 6, 12, and 24 hours postoperatively. Our results agreed with Sato’s study when comparing QL2 block to caudal ropivacaine/Marcaine in children who underwent vesicoureteral reflux, showing a non-significant difference in postoperative pain scores at 0, 4, 24, and 48 hours postoperatively (12).
The current results are consistent with Samerchua et al., who found similar pain scores at 30 minutes and 1, 2, 6, 12, and 24 hours between the groups, attributing this to the small sample size or children might have their doses of oral acetaminophen 1 or 2 hours before recording pain scores (14). Oksuz et al. found that at 4, 6, and 12 hours after surgery, FLACC scores were significantly lower in the QL block group than in the caudal group, while at 30 minutes and 1, 2, and 24 hours, FLACC scores were not significantly different between the groups. In their study, they used a relatively larger volume of 0.25% bupivacaine (0.7 mL/kg) while we used 0.25% bupivacaine (0.5 mL/kg) (13). During the QL block, local anesthetics diffused between the posterior aspect of the QL muscle and the medial layer of the thoracolumbar fascia, close to the thoracic paravertebral space (TPVS) (20). Børglum et al. described the ultrasound-guided QL block in 2013 (21).
For retroperitoneal and abdominal surgeries, QL block was reported to have excellent postoperative pain management. The original QL block was shown to anesthetize both anterior and lateral cutaneous branches from T7 to L1. The impact of the QL block was thought to be caused by the local anesthetic, spreading cranially from its lumbar deposition into TPVS (21). Carney et al. verified this spread when they discovered evidence of local anesthetic with a contrast agent in TPVS after applying QL block (22). QL2 block was investigated by Blanco et al., who studied the original bilateral QL block after cesarean section (18). The authors found that injecting a local anesthetic into the QL muscle’s posterior border (between the latissimus dorsi and QL muscles) provided enough analgesia, represented in a reduced visual analog scale (VAS) score and reduced postoperative morphine consumption. Unlikely, the epidural space is known for its high vascularity, which fastens the absorption of local anesthetics, explaining the shortened duration and the less effective analgesia of the caudal block (23). This was demonstrated in a relatively recent meta-analysis performed in hypospadias surgery, comparing caudal anesthesia with other PNBs and reporting that caudal anesthesia had a significantly shorter analgesia duration, higher pain scores up to 24 hours, and higher analgesia consumption (24). This pattern of caudal analgesia, in turn, made anesthesiologists look for other regional analgesic techniques. However, caudal anesthesia is the most frequently used regional anesthetic technique in the pediatric population because of its simplicity and low complication rate (25-27).
According to our data, the comparison between QL block and caudal block in pediatrics who underwent lower abdominal surgeries was limited. In their studies, Ipek, Oksuz et al., and Sato ensured the analgesic efficacy of QL block while the superiority of postoperative analgesia was in favor of QL block, as reported by both Oksuz et al. and Sato (11-13). Regarding hemodynamics, we were aware of the effect of caudal anesthesia on hemodynamics, such as hypotension and the spread of local anesthetics toward TPVS, which might lead to a sympathetic block in QL block and its effect on hemodynamics (28, 29). This effect was mentioned by Sa et al., who observed severe hypotension and tachycardia at 30 to 40 minutes after giving QL block to 2 patients who underwent total gastrectomy and right hemicolectomy (29). We found hemodynamic stability in both groups as a non-significant difference between the groups regarding SBP, DBP, and HR for 45 minutes, except at the reading of 30 minutes, as SBP was significantly higher in group C with no clinical significance. This study did not report any intraoperative complications due to needle insertion or adverse effects of local anesthetic, including arrhythmia, convulsion, hypotension, or allergic reaction during the intra- or postoperative periods. This agrees with Sato’s study, as he did not record any complications associated with local anesthetic toxicity (11). Blanco et al. found that adult patients with QL block had lower serum levels of local anesthetics than those with Transverse abdominis plane (TAP) block, suggesting that QL block might be more reliable (19). This could be a reason for selecting the QL block for children. Blanco et al. reported that no complications related to needle insertion were encountered in patients receiving QL2 block who had a cesarean delivery; the reason is that QL2 block is superficial and safe because the QL muscle is superficial and isolates the needle tip from the peritoneum, limiting the danger of intraperitoneal injection and bowel injury. In our study, parent satisfaction was statistically higher in the QL2 block than in the caudal block. Ipek et al. also found significantly higher parent satisfaction in the QL2 block than in the caudal block (12).
5.1. Limitations
Measurements could not be taken to the sensory block level of QL, and caudal blocks were applied to children aged 1 to 7 years, which could be a limitation of the study. We did not know if a higher level of dermatomal sensory block was provided compared to the caudal block.
5.2. Conclusions
According to the outcomes of this work, the QL2 block is more effective and sustains postoperative analgesia time with greater parents’ satisfaction in pediatric individuals undergoing unilateral lower abdomen surgery than the caudal block, which has been in use for many years.